Assessment 5 Rheumatology
advertisement
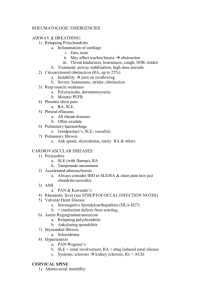
Assesment 5 Rheumatology Module Professor Hints Metabolic Bone disease Know biochem markers of bone turnover Formation: BSALP, Osteocalcin, carboxyterminal propeptide of type 1 collagen (P1NP) Resorption: Pyridinium crosslinks, n-telopeptide, carboxyterminal of type 1 collagen (CTX-1) Recognize key clinic features of the metabolic bone disorders Know about OI, Paget’s etc. Know the pathophys basis of each Know about OI, Paget’s etc. Regional Rheumatic Pain Syndromes know the anatomy and name of common regional non-articular pain syndromes Rotator cuff tendinitis (recall Neer’s sign), Bicipital tendonitis (Yergason’s sign, Speeds test, Popeye’s sign), Adhesive capsulitis (frozen shoulder, associated with diabetes), Olecranon bursitis (golf ball elbow), Lateral (tennis elbow) epicondylitis, medial epicondylitis, Ulnar nerve entrapment, Flexor tenosynovitis, de Quervain’s tenosynovitis (abductor pollicis longus, extensor pollicis brevis, recall finklestein’s test), Ganglion, Carpal Tunnel syndrome (Tinel’s sign and Phalen test), Dupuytren contracture, Trochanteric bursitis (point tenderness over greater trochanter), Meralgia parasthetica, Baker’s cyst, prepatellar bursitis (can be septic), Achilles Tendinitis (Thompson sign), Plantar fasciitis (pain in plantar area of heel), Pes planus (flat foot), mortons neuroma, Hammertoe (flexion of PIP and tip of toe points down), Bunionette (prominence of metatarsal head) know the clinical features of fibromyalgia Widespread pain>3mo., 11/18 tender points, could be involved with cortical centers involved in pain stimulation, tx. educate patients,exercise, improve sleep, Normal Joint Structure and Lab Testing understand the structure of the normal diarthrodial joint Have a synovial lining, freely movable, includes all peripheral joints Synarthrosis has no synovial lining, fixed joints (skull,tooth socket, tibiofibula jxn., manubriosternal joint, symphysis pubis) Assesment 5 Rheumatology Module Professor Hints understand the components and properties of cartilage Avascular, no nerve supply, low cell content (chondrocytes only), rich in matrix Matrix composed of 60-85% water, collagen, proteoglycans (hyaluronic acid, link proteins), other glyoproteins, lipids know which autoantibodies are present in which rheumatic diseases RF present in RA (80%), SLE (40%), Sjogren’s (90%), Cryoglubinemia (>90%) o RF should only be used to confirm, not diagnose ANA sensitive for SLE (95%) o Can be drug induced or caused by MCTD, Sjogrens, scleroderma, myositis, vasculitis SSA-A/Ro o Sjogrens (75%), SLE (25%), Congenital heartblock (remember this) Sm o Lupus in African Americans (more specific) U1RNP o MCTD, SLE Anti-dsDNA o More specific, less sensitive for SLE o Correlates with renal disease o Usually negative in drug induced lupus Jo1 o Inflammatory myositis o Directed against tRNA histidyl synthetase Anti-Centromere o Scleroderma Antiphospholipid antibody o Lupus o Actually a pro-coagulant C-ANCA o Proteinase 3 o Wegener’s P-ANCA o Myeloperoxidase o Microscopic polyangiitis (glomerulonephritis happens) o Churg-Strauss (remember eosinophilia and asthmatics) Cryoglobulin o Ig precipitate when serum is cooled to 4 degrees or lower o Associated with malignancy and Hep C understand the limitations of laboratory tests in rheumatology Assesment 5 Rheumatology Module Professor Hints CRP more sensitive than ESR Laboratory tests can’t always diagnose, many test are used to confirm (e.g., RF and FANA) if they are used as screening procedures we will get many false positives Rheumatoid Arthritis (RA) recognize articular and extra articular features of RA Inflammatory condition affecting synovium, symptoms >6 wks, symmetrical presentation, MCP, PIP, wrists affected most. Swelling usually confined to joint cavity. Ulnar deviation, swan neck, boutonnière deformity, flexion contractures etc. , cervical spine subluxation, Felty’s (neutropenia, leucopenia), Keratoconjunctivitis sica, xerostomia, episcleritis, scleritis, understand the pathogenesis of RA, including the role of cytokines, T cells HLA-DR4 (0401,0404,0408) bind and present antigens to T cells leading to activation, second signal (CD86/28) leads to T cell activation and cytokine release. Recall CTLA4 inhibits this second signal. RA is involved with Th17 and Th1 pathways. Cytokines destroy synovium and cause pannus formation. B cells also involved in RA, Th1 pathway (TNF-alpha, IFN-gamma). Drugs exist to inhibit TNFalpha (infliximab) and CD20 on B cells. understand the inflammatory nature of RA See above. Spondyloarthropathy recognize the key clinical features of each of the spondyloarthropathies Common features o RF negative o HLA-B27 association o Axial involvement with sacroiliac joint o Enthesitis o Dactylitis o TNF alpha Ankylosing Spondylitis o Inflammation of spinal joints, fusion of bony spine o More common in first degree relatives of HLA-B27 o Back pain, stiffness, worse in morning and improves with exercise o Anterior uveitis o Aortic regurg, apical lung fibrosis secondary amyloidosis, o Sacroiliac tenderness, limited spine motion, loss of lumbar lordosis Assesment 5 Rheumatology Module Professor Hints o Abnormal schober’s tes o Reduced chest expansion Enteropathic arthritis o Crohn’s, IBS, etc. o Peripheral arthritis o Asymmetric o Pyoderma gangrenosum o E. nodosum Reactive arthritis o Arthritis, Urethritis, conjunctivitis o Shigella, salmonella, campylobacter, o Asymmetric o Enthesitis, Oral ulcerations, Keratoderma blennorrhagica o Oncholysis Psoriatic arthritis o Synovial inflammation o DIP involvement o Arthritis mutilans o Axial involvement o Nail pitting! o Pencil in a cup o Enthesitis, Dactylytis understand the role HLA-B27 plays in spondyloarthropathies Class I MHC that binds peptides and presets to CD8+ T cells Scleroderma understand the role of fibrosis in scleroderma o o o o o o o o o Thickening and fibrosis is main defect in scleroderma. Sclerodactyly Raynauds (fibrosis of vessels) Telangectasias Nailfolds Calcinosis Watermelon stomach Pulmonary fibrosis * cause of death PDGF, Collagenase 1, important in pathogenesis, Th2 and CD4 mediated recognize scleroderma renal crisis o IF blood pressure rises slightly, put on ACE-I Assesment 5 Rheumatology Module Professor Hints distinguish between limited and diffuse forms of scleroderma o Limited o Not with systemic disease o Scl-70 negative o Generalized o Scl-70 positive Infectious Arthritis distinguish between gonococcal and non gonococcal septic arthritis Gonococcal typically seen in pt. who are sexual active (younger). Non-gonococcal is primarily S. auerus (except for prosthetic joints which is coag. Neg. staph, and i.V.DA which is candida and pseudomonas). Non-gonococcal is typically isolated in aspiration, gonococcal is not (have to look to sites of primary infection). understand the role of synovial fluid analysis in the diagnosis of septic arthritis – interpret results Typically purulent in bacterial arthritis. >80k WBC’s, >75% PMN’s, Gram stain + in 60-80%, crystals may co-exist. Note: Parvovirus can mimic RA, Rubella is involved with squatting pose, and Hep B /C can mimic OA distribution (knees). Hep C is in hands, wrists, knee’s also associated with cryoglobunemia (I and II). Lyme disease is monoarticular or pauciarticulr (usually involves Knee and TMJ), TB commonly infects spine/knee. Gout distinguish between under excretors and over producers of uric acid, recognize urate crystals under polarizing microscopy, know pathophys basis of the disease Urate crystals under polarizing microscopy when parallel to polarizer are negatively birefringement (yellow). Under excretors are those who can’t get rid of uric acid (e.g, URAT1 mut., low dose ASA, Hctz, over producers make too much (HGPRT def., PRPP synthetase over active). Uric acid accumulates in joints and crystallizes at the appropriate Ksp producing monosodium urate crystals. PMN’s engulf these crystals and release cytokines and enzymes which cause inflammation, pain, and damage to surrounding tissues. sUA can be normal in acute gout attacks. Never start chronic treatment in acute attacks. Assesment 5 Rheumatology Module Professor Hints distinguish between gout and other crystalline arthropathies Gout and pseudogout more present in men. Family history is often present in gout but not pseudogout. Primary site of pseudogout is knee, primary of gout is MTP. Both present with fever, tophi are not common in pseudogout. Bursa affected in gout, tendons in pseudogout. know the effects of diet on urate production, other non-pharm treatments At best diet decrease sUA 1-2mg/dl. Allopurinol, Febuxostate both decrease uric acid production (inhibit XO) Other Crystalline Arthropathies recognize calcium pyrophosphate crystals under polarizing microscopy Positively birefringement (blue when parallel, yellow when perpendicularbirefringment means has two different colors). know clinical features of the various non-urate crystal diseases See above for pseudogout. Most attacks of pseudogout are spontaneous. Synovial fluid has poor viscosity, and is moderatey cloudy. WBC>20k. Rhomboid shaped crystals (CPPD) in pseudogout. No erosions in pseudogout, but yes in gout. BCP accumulates sometimes in OA. BCP stain with azilarin red stain. They also accumulate in Milwaukee shoulder syndrome which can mimic rotator cuff tendinitis. It is not known whether the tear’s in Milwaukee shoulder syndrome correlate with crystals, or if the crystals actually cause the tears. MSS is a disease of older white women*. CPPD comes from transglutaminase-2 enzyme. Primary oxalis is a rare calcification of articular joints (typically hand) and renal calcifications, can also be acquired due to secondary conditions. Systemic Lupus Erythematosus (SLE) and Sjogren’s Syndrome understand the role of immune complexes in the pathogenesis of SLE o Complement is deposited, ADCC causes inflammatory cascade. recognize clinical features of SLE and Sjogren’s syndrome o SLE: Malar rash, oral ulcers, alopecia, dermatitis, arthralgias, arthritis, muscle pain, serositis, renal disease (correlates to dsDNA Ab), Neuropsychiatric, Hematologic (anemia), GI, pulmonary effusions, Neonatal lupus associated with SSA/Ro and congenital heart block. FANA is helpful for screening, use Anti-Sm to rule in (better in African Americans). All SLE has + FANA. o Sjoergen’s: Keratoconjunctivitis sicca (schirmer test), xerostomia, parotid enlargement, +FANA,+RF, +SSA/Ro, SSB/La Assesment 5 Rheumatology Module Professor Hints o Recall: DILS in HIV has dry eyes also (CD8 mediated) understand the role of autoantibodies in Sjogren’s syndrome o AutoAb destroy exocrine glands (salivary/lacrimal) o Mainly CD4+ Osteoarthritis (OA) understand the pathogenesis of OA, and the contributors to secondary causes o Hemochromatosis, Wilson’s disease (OA in wrist), Ochronosis (Alkaptonuria), acromegaly o Cystic changes in bone, osteophyte formation, increased water in collagen early on, join space narrowing, bony sclerosis, misalignment o DISH o Excessive tendon calcification Vasculitis recognize the key clinical features of Wegeners, HSP, PAN, PMR, temporal arteritis, Kawasaki’s, Takayasu’s This objective basically says recap the entire vasculitis lecture, which we have in our handout. Note to self: Remember polymyalgia rheumatic can lead to temporal arteritis. Takayasu’s not associated with GMN. Multiple aneurysm’s seen on arteriogram. Kawasaki: Strawberry tongue, desquamation, ertythema, coronary disease.