The Evaluation and Treatment of the Acutely Agitated
advertisement

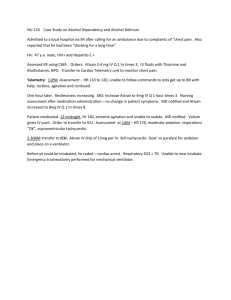
The Evaluation and Treatment of the Emergency Psychiatric Patient W. Scott Griffies, M.D. LSUNO Department of Psychiatry An ER Behavioral Healthcare Infrastructure • ER physician assessment includes mental status exam. • Crisis Assessment S.W., P.N.P., or P.R. include complete psychosocial assessment. • Psychiatric Consultant rounds bi-daily. (possible telepsychiatry) • Social Service (S.W.) Discharge Plan/Resources. CIU/BHETU • Stabilization Units • In Conjunction with ER • 5-30% have medical illness Disposition Evaluation • • • • • Nature and duration of Illness Relationship to baseline Adequacy of self-care Level of social supports Risk of homicide/suicide Differential Diagnosis • • • • Delirium Psychotic Disorders Mood Disorders Developmentally Disabled – have above diagnoses, but, since they are often nonverbal, diagnoses will be primarily based on behavioral observations and descriptions. Medical Delirium • Acute Onset • Fluctuating, Altered Sensorium • Abnormal MMSE Life-Threatening - WWHHIMP • • • • • • • • Drug withdrawal Wernicke encephalopathy Cerebral hypoxemia Hypoglycemia Hypertensive encephalopathy Intracranial bleeding Meningitis/encephalitis Poisoning An Option for Outpatient Psychosocial Planning of Substance Dependence • Call AA/NA and have sponsor visit patient in ER • Prescribe daily or bidaily NA/AA Group meetings for first 2 weeks post discharge. • Follow-up with addiction disorder clinic. • Register for Rehab Program. Psychotic Disorders • • • • • Clear sensorium Delusions Hallucinations Disorganized speech and behavior Flat or inappropriate affect Psychosis Differential • • • • • Substance – induced Due to medical condition Schizophrenia Mood Disorder (BMD/MDE) Dementia with delusions Psychosis Differential (cont.) • Brief Psychotic Episode • Schizophreniform • Delusional Disorder Mood Disorders – BMD and MDE +/Psychotic Features, Severe Agitation • Mania - - Decreased need for sleep, increased energy, agitation, irritability, liability, projects, missions, hypertalkative, pressured, racing. • R/o organic etiology, especially if acute. Treatment of Acute Psychotic/Severe Agitation • Haldol 5 mg, Benadryl 50 mg, Ativan 2 mg IM. (B52) • Repeat Haldol 5mg IM +/- Ativan 1-2 mg q1-2h IM as needed until calm. Other Guidelines • Use 25-50% for elderly • Monitor ECG when possible • Most calm after 1-2 injections Treatment of Acute Agitation Other Options • Zyprexa 10 mg q 2 h X 1, then q 4 h not to exceed 30 mg/24 h. Do not give concomitant Benzos. • Geodon 10 mg q 2 h or 20 mg q 4 h, not to exceed 40 mg/24 h. • Use 25-50% for elderly/medically compromised. • Not indicated for dementia-related psychosis. Switching to Oral Antipsychotics for Schizophrenia, BMD, MDE with Psychoses While Awaiting Admission. • Haldol 2-5 mg po q daily --BID • Zydis (melts in mouth): 10-15 mg po q daily initially. • Seroquel 50 po BID. Increase by 100 mg/day to 600 mg/day in divided doses - - more at night. Switching to Oral Antipsychotics for Schizophrenia, BMD, MDE with Psychoses While Awaiting Admission. (Cont.) • Risperidol 1 mg po BID. 1st day, 2 mg BID 2nd day, 3 mg 3rd day. • Geodon 40 mg po BID (usually 2nd line) • Abilify 10-15mg • Use 25-50% for elderly/medically compromised. Second Generation Antipsychotics: Long term Side Effects • Zyprexa, -- most weight gain, metabolic syndrome (Relative cotraindication in D.M. Obesity, Cholesterol) • Risperidol, Seroquel – Second-most metabolic syndrome issues. • Geodon, Abilify – least weight gain and metabolic syndrome. Second Generation Antipsychotics: Side Effects • Risperidol – hyperprolactenemia • Geodon – Relative QTC prolongation Relative contraindication in patients with CVS history. If CVS history, perform EKG. • Seroquel – most antihistaminic, sedating Anxiety • • • • • Adjustment d/o with anxious mood GAD Panic OCD Social Phobia ER Treatment of Anxiety • Ativan 1-2 mg po q 4-6 h • Klonipin 0.5 – 1 mg po BID – TID • Use SSRI long term. Borderline P.D. • • • • Impulsivity Parasuicidal behavior Abandonment anxiety Labile affect Agitation in Borderline P.D. • Benzodiazepines may disinhibit • Seroquel 50 po nightly/BID Suicide • • • • • • Level of intent Level of lethality Prior attempts Late life white divorced male Living alone Lack of sleep/agitation Major Depressive Episode (MDE) • Depressed mood or loss of interest/pleasure x 2 weeks. • Five/nine symptoms – depressed mood, interest/pleasure, or weight, insomnia/hypersomnia, psychomotor agitation/retardation, fatigue/ energy, selfworth, concentration, SI Choice of Antidepressant – General Issues • Needs weekly f/u x 4 weeks with new antidepressant • Start low, go slow, especially in anxious, somatisizing patients. • Early side effects usually diminish in 10-14 days. If tolerable, hang in there. Choice of Antidepressant – General Issues • Activating agent may need sleeping agent – Trazodone (Priapism), Ambien, Lunesta • Don’t give if mania hx Antidepressant Choices– Selective Variables • Wellbutrin (150 mg) norepinephrine/dopamine – activating, energy, concentration, no sexual SE’s. • Effexor (75 mg) - combination serotonin, norepinephine – monitor BP, especially at higher dose – good for GAD also. Antidepressant Choices– Selective Variables • Cymbalta (30 mg) – combination norepinephrine/ serotonin – pain syndromes, start 30 mg for 7-14 days to mitigate nausea. • Remeron (15 mg) – po q nightly – combination serotonin, norephinephrine, sedating Antidepressant Choices – Selective Variables • Prozac (10-20 mg) – in some, more activating, give in am, start 10 mg in panic/anxiety. • Paxil (10-20 mg) – in some more sedating, more wt gain. Antidepressant Choices – Selective Variables • Zoloft (25-50 mg) – activating or sedating, can be nicely calming • Celexa/Lexapro (10-20 mg) – most serotonin - receptor selective. ER Physician • R/O underlying medical causes for presenting delirium, psychosis, or mood disorder. • PEC if S/H or G.D. Mental Status Exam: ARTT SMAJIC • Appearance – well dressed/disheveled • Rapport – good/eye contact • Thought Process – linear, goal directed, looseness of associations (LOA), tangential, disorganized • Thought Content – S/HI, A/VH • Speech – N/R/R/V/T Mental Status Exam: ARTT SMAJIC (Cont.) • • • • • Mood – upset, angry, sad Affect – blunted, full range, depressed Judgment – good, poor Insight – good, poor Cognition – see MMSE “MINI-MENTAL STATE EXAM” Maximum Score 5 5 Score Orientation ( ) What is the (year) (season) (date) (day) (month)? ( ) Where are we? (state) (country) (town) (hospital) (floor). MMSE (Cont.) Maximum Score Score Registration 3 ( ) Name 3 objects: 1 second to say each. Then ask the patient all after you have said them. Give 1 point for each correct answer. Then repeat them until he learns all 3. Count trials and record. Trials_________ MMSE (Cont.) Maximum Score Score Attention and Calculation 5 ( ) Serial 7’s 1 point for each correct. Stop after 5 answers. Alternatively spell “world” backwards. Recall 3 ( ) Ask for the 3 objects repeated above. Give 1 point for each correct. MMSE (Cont.) Maximum Score Score Language 9 ( ) Name a pencil, and watch (2 pts) Repeat the following “No ifs, ands or buts.” (1 point) Follow a 3-stage command: “Take a paper in your right hand, fold it in half, and put it on the floor” (3 points) Read and obey the following: MMSE (Cont.) Maximum Score Score Close your eyes ( 1point) 5 ( ) Write a sentence ( 1 point) Copy design (1 point) Total Score________________ FIG 6-1. From Folstein MF, Folstein SE, McHugh PR: J. Psychiatr Res 1975, 12:189-198 Structured Diagnostic Interview with Psychosocial Assessment • S.W./Psychiatric Nurse Practitioner/Psychiatric Resident - HPI, DSM IV symptoms - Past psychiatric history - Family psychiatric history - Past medical history - Social history with current social supports and resources. - MSE Psychiatrist Consultant • Confirm diagnosis • Medication recommendations Disposition and Treatment Recommendations • Inpatient • Outpatient • ER medications Withdrawal Delirium (alcohol, benzodiazepine, barbiturates) • Fixed with symptom triggered schedule. Ativan 1-2 mg PO, IM or IV, Q 4-6 h; Ativan 1-2 mg PO, IM, IV; Q 1-2 h prn P>100, BP> 150/100; hold for sedation • Or, give symptom – triggered alone, if more appropriate. Alcoholism • Thiamine 100 mg po q daily • Folate 1 mg po q daily • MVI 1 taken po q daily Opiate Withdrawal Evaluation • Positive Opiate UDS • Positive history • Dilated pupils, piloerection, muscle cramps Opiate Withdrawal Treatment • Clonidine 1 mg po TID – QID with 1 mg po q 2 h for BP > 150/100, p > 100 • Bentyl 20 mg po QID prn abdominal cramps. • Pepto-Bismol, Imodium, Maalox, Mylanta • Robaxin - muscle spasm. Substance Dependence Disposition • Medical admission for detoxification if unstable. • Psychiatric admission if suicidal. • Outpatient addiction follow-up and rehab. Outpatient Detoxification Option • Patients w/o history of prior seizures or withdrawal delirium. • Valium 10 mg po TID-QID with 2-3 prn for agitation/tremulousness • Taper over 5-7 days • MVI Ativan Outpatient Detoxification Option • If patient has increased LFT’s • Ativan 1-2 mg po q 4-6 h with 2-3 prn’s • Taper over 10-14 days by dose, while preferentially maintaining frequency. MEDICAL DELIRIUM TREATMENT ISSUES • CBC, electrolytes, BUN, Cr, LFT’s, UDS, possible CT scan. • Admit for medical stabilization of underlying causes. Psychosis Due to Medical Condition • Drugs and Toxins • Intracranial masses (tumor, abscess, subdural) • Anoxia • Normal Pressure Hydrocephalous Psychosis Due to Medical Condition (cont.) • • • • • Neurodegenerative diseases Infection Nutritional (B12 , Folate) Metabolic/Endocrine Inflammatory/autoimmune Mood Disorder Due to a Medical Condition • • • • Carcinoid Pancreatic Cancer Collagen-vascular disease Endocrinopatheses (Cushings, Addison’s hypoglycemia, hyper/hypocalcaemia, hyper/hypothyroid) • Lymphoma • Viral illness (mono, hepatitis, flu) Depressed Mood Due to a Pharmacologic Agent • • • • Clonidine Propanolol Corticosteroids Ibuprofen • • • • Indomethacin Ampicillin Teracycline Cimetidine Mania Due to Pharmacologic Agent • • • • • • Baclofen Cimetidine Corticosteroids Disulfiram Isonazid Levodopa