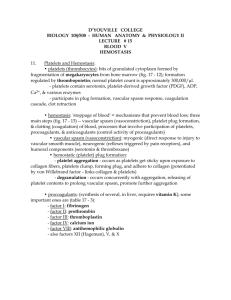
Platelet mediators
advertisement

Nerves Smooth muscle Red cells Platelets White cells eg neutrophils Endothelium Thrombosis and haemostasis Platelet adhesion, aggregation, release Coagulation thrombin Local vasoconstriction Balance of stimulatory/inhibitory mediators Haemostasis trigger = tissue damage Thrombosis trigger = plaque rupture? Interactions between : •platelets •coagulation cascade •endothelial cells •vascular smooth muscle (neuronal control too) Resting platelet Activated platelet What do platelets do when they are activated? Adhere to eg vessel wall Change shape – from disc to spiny sphere Expose fibrinogen receptors at their surface Expose PF3 at their surface Synthesise lipid-derived mediators (TXA2, PGD2, PAF) Synthesise nitric oxide (NO) Release the contents of their dense granules (5-HT, ADP, ATP) Release the contents of their alpha granules (proteins – including PF4, fibrinogen, vWF, PDGF) Starts within seconds, finished within a couple of minutes PLATELET RESPONSES: Shape change, aggregation, release ADP or other aggregating agents Fibrinogen + Ca2+ Exposure of PF3 (procoagulant phospholipids) Thrombin Blood clotting Release of soluble mediators Release of α granule contents Intrinsic pathway (in vitro contact) Extrinsic pathway (tissue damage) Ca2+, PF3 Ca2+, PF3 X Xa Ca2+, PF3 II Prothrombin IIa Thrombin XIII Ca2+ Fibrinogen Fibrin Ca2+ XIIIa Stabilised fibrin Binds to activated platelets Blood clot Platelet activation Platelet activation involves an increase in cytoplasmic Ca2+ Platelets are stimulated by proteins: •collagen - subendothelial surface •thrombin – coagulation cascade And by small molecules: •ADP/ATP – from damaged cells and platelets •PGH2/TXA2 – from platelets •PAF – from platelets •5-HT – from platelets •adrenaline/NA - circulating hormones Platelet inhibition Platelet inhibition involves an increase in cytoplasmic cyclic nucleotides (cAMP or cGMP) Platelets are inhibited by : •PGI2 – from endothelium •PGD2 – from platelets •adenosine – released by hypoxic cells, formed during ADP/ATP degradation •NO – from platelets and endothelium Platelet mediators Platelets release soluble compounds that affect nearby cells Stimulatory mediators: •ADP/ATP – stored in vesicles •5-HT – stored in vesicles •PGH2/TXA2 - synthesised •PAF - synthesised Inhibitory mediators: •NO - synthesised •PGD2 - synthesised As a general rule: • things that activate platelets also constrict blood vessels • things that inhibit platelets also relax blood vessels Platelet-vessel wall interactions Interactions between platelets and the vessel wall determine the final outcome of an initial small aggregation The endothelium is important in determining whether or not platelet aggregation will spread or be reversed Healthy intact endothelium will respond by releasing factors that inhibit aggregation and cause vasodilation – PGI2 and NO If the endothelium is damaged aggregation and vasoconstriction will dominate - THROMBOSIS Thrombin Healthy endothelium: platelets will not aggregate, blood vessel will relax Platelet factor 3 Collagen ADP PGI2 5-HT AGGREGATION PAF Adenosine PGH2/TXA2 PGH2/TXA2 Thrombin NO PAF ADP 5-HT PGI2 + NO VASODILATION Endothelium Vascular smooth muscle Thrombin Damaged endothelium: platelets will aggregate, blood vessel will contract Platelet factor 3 Collagen ADP 5-HT AGGREGATION PAF PGH2/TXA2 PGH2/TXA2 Thrombin NO PAF CONTRACTION ADP 5-HT Vascular smooth muscle