Regulation of FGF-Mediated Control of Cartilage Maturation at
advertisement

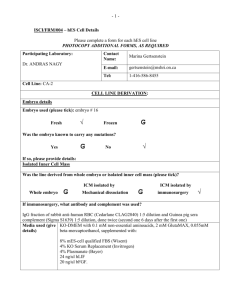
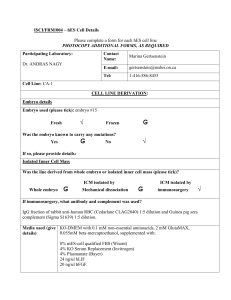
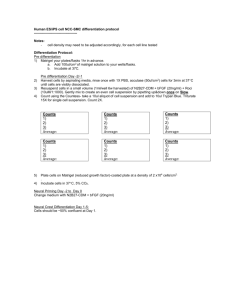
Extracellular Matrix Based Regulation of a Cytokine Gradient at the Growth Plate Jonathan Behr David Berry BEH.400J Project Presentation Diastrophic Dysplasia Hereditary Multiple Exostoses Outline Goals Introduction Methods GAG interaction with cytokines Model system: Long bone growth Model formulation Model implementation Results Proposed experiments to test model Conclusions Project Goals Quantitate how the physiochemical nature of the extracellular matrix modulates FGF2 signaling FGF2 must be localized to differentially signal for angiogenesis, chondrogenesis and osteogenesis Heparan sulfate glycosaminoglycans (HSGAGs) bind FGF2 This process is important in development, and errors therein can lead to a wide range of abnormalities An understanding of this system has applications in treating these pathologies and in tissue engineering GAG Interaction with cytokines HSGAG are one of several components of the ECM. HSGAG consist of a proteoglycan core and a sugar chain with repeating units of a uronic acid (glucuronic or iduronic with possible 2-O sulfation) linked 1→4 to a glucosamine (with possible 3,6, and N sulfation). Variety in sequence and composition allows for many potential interactions. Roles of HSGAG in the ECM Reservoir for proteins, preventing degradation. Impediment to diffusion. Non-specific binding from high charge density Co-factor for growth factor signaling by facilitating ligand dimerization and/or presentation to receptors. Maeder, Scientific American Model System: The Growth Plate In endochondral ossification, the formation of calcified bone is separated from mesenchymal condensation by the development of a Resting Chondrocytes cartilage anlage that regulates bone growth Proliferating Chondrocytes Prehypertrophic Chondrocytes Hypertrophic Chondrocytes Trabecular Bone Human Humancartilage cartilageduring duringendochondrial endochondrialossification ossification stained stained with H&E with H&E and alcian and alcian blue at blue 40x atmagnification. 120x magnification. (Wheater’s (Wheater’s Functional Functional Histology) Histology) Model System: The Growth Plate FGF2 is secreted by the terminal hypertrophic chondrocytes and acts on the proliferating chondrocytes, inhibiting their proliferation and inducing their differentiation (Ornitz and Marie) Assumptions: Geometry Cylindrical geometry, radial symmetry radial dimension >> z direction Model as 1-D problem in z Isotropic environment in hypertrophic zone Assumptions: Equations Boundary conditions Angiogenic side boundary: Constant influx of bFGF Match so with base parameters, 5ng/ml [bFGF] at source at steady state Proliferating cartilage side: [bFGF] x(∞) = 0 Total receptor number at the cell surface is constant Rate constant for internalization of complexes is constant Model Cartoon H H H H H H H H H H H H H 5ng/ml base H H H H H H H bFGF Modified from Lander et al. (2002) Model Equations L [bFGF] LR [bFGF FGFR] LH [bFGF HSGAG] R tot [FGFR] [bFGF FGFR] H tot [HSGAG] [bFGF HSGAG] dL d 2L r r h h D 2 kon L( Rtot LR) koff LR kdeg L kon L( H tot LH ) koff LH dt dx dLR r r kon L( Rtot LR) koff LR kint LR dt dLH h h kon L( H tot LH ) koff LH dt A [bFGF]/R tot B [bFGF FGFR]/R tot H [bFGF HSGAG] / H tot Implementation 1. 2. 3. Built-in MATLAB BVP and PDE solvers failed Created system of ODEs by discretizing space, using central finite difference method on PDE Solved system dynamically by using MATLAB implicit variable order ODE solver ode15s Base Parameters from Literature Parameter Value Description Deff 0.5e-8 m2/s Effective diffusivity in the ECM F0 5 ng/ml (0.278 nM) S.S. concentration of bFGF at “source” Htot 13 uM Number density of HS binding sites (ECM and cell surface) Rcell 1480 Number of FGFR per cell rcell 10 um Cell radius L 7 cell diameters Distance between bFGF source and proliferating chondrocytes kdeg 3.5e-5 /s Rate constant for degradation of free bFGF kint 2e-4 /s Rate constant for consumption of bFGF due to receptor complex mediated internalization konh 4.2e5 /(M*s) On rate for bFGF·HS complex formation koffh 0.01 /s Off rate for bFGF·HS complex formation konr 1.36e10 /(M*s) On rate for bFGF·FGFR complex formation koffr 0.18 /s Off rate for bFGF·FGFR complex formation ε 0.2 Volume fraction ECM v 4.8e-013 M/s In-flux of bFGF at angiogenic boundary Presentation of Results Distance where concentration threshold (1 ng/ml) is crossed Distance where receptor occupancy is less than 10% (B<0.1) Time to 80% of steady state [bFGF] at x=0 Phase plots relating results to “normal” physiology Base Case Results, 3D Base Case: Ass0 = 2.9635e-010 M Threshold A at x = 51.4286 m 80% S.S. at t = 43 days -10 x 10 [bFGF] 2 1 [bFGF*FGFR]/rtot 0 0 50 100 150 200 m 250 300 7 6 5 4 2 1 0 3 2 1 0 3 2 1 0 3 Threshold B at x = 108.5714 mtime (days) 1 0.5 0 0 50 100 150 -3 250 300 7 6 5 4 time (days) m x 10 [bFGF*HS]/htot 200 6 4 2 0 0 50 100 150 200 250 300 7 6 5 4 time (days) Base Case Results, 2D Base Case: Ass0 = 2.9635e-010 M Threshold A at x = 51.4286 m 80% S.S. at t = 43 days -10 x 10 2 1.5 1 0.5 0 0 50 100 150 200 250 150 200 250 150 200 250 [bFGF*FGFR]/rtot Threshold B at x = 108.5714 m 0.8 0.6 Increasing Time 0.4 0.2 0 0 50 100 0 50 100 0.012 [bFGF*HS]/htot Concentrations [bFGF] 2.5 0.01 0.008 0.006 0.004 0.002 0 m Distance Example of Faster Kinetics [bFGF] Profiles For 10*base kdeg: Threshold A at x = 5.7143 m 80% S.S. at t = 5 days -11 x 10 7 [bFGF] 6 5 4 3 2 1 0 0 50 100 150 200 250 150 200 250 150 200 250 [bFGF*FGFR]/rtot Threshold B at x = 62.8571 m 0.8 0.6 0.4 0.2 0 0 50 100 50 100 -3 x 10 [bFGF*HS]/htot 3 2.5 2 1.5 1 0.5 0 0 m Example of Longer Gradient [bFGF] Profiles For 10% base kdeg: Threshold A at x = 148.5714 m 80% S.S. at t = 554 days x 10 -10 12 [bFGF] 10 8 6 4 2 0 0 50 100 150 200 250 150 200 250 150 200 250 [bFGF*FGFR]/rtot Threshold B at x = 205.7143 m 0.8 0.6 0.4 0.2 0 0 50 100 0 50 100 [bFGF*HS]/htot 0.05 0.04 0.03 0.02 0.01 0 m Example of Unstable Gradient -8 x 10 [bFGF] Profiles For 10*v/rtot: Threshold Met At x = 280 m 80% S.S. at t = 34 days [bFGF] 4 3 2 1 0 0 50 100 150 200 250 150 200 250 150 200 250 [bFGF*FGFR]/rtot Threshold B at x = 280 m 0.8 0.6 0.4 0.2 0 0 50 100 0 50 100 [bFGF*HS]/htot 0.6 0.5 0.4 0.3 0.2 0.1 0 m Steady State Dependence on “External” Parameters 2 Phase Plane of Threshold Acceptability At the End of the Growth Plate Fold Change From Base v 10 1 10 Pathological 0 10 Unnacceptable B -1 10 Acceptable -2 10 -2 10 -1 10 0 10 Fold Change From Base kdeg 1 10 2 10 Steady State Dependence on “Cellular” Parameters 2 Phase Plane of Threshold Acceptability At the End of the Growth Plate 10 Fold Change From Base kint Acceptable 1 10 Unacceptable B 0 10 -1 10 •Chondrodysplasia punctata •Acrocephalosyndactyly syndrome •Achondroplasia Pathological -2 10 -2 10 -1 10 0 10 Fold Change From Base Rtot 1 10 2 10 Steady State Dependence on “ECM” Parameters 2 Phase Plane of Threshold Acceptability At the End of the Growth Plate Fold Change From Base D 10 Pathological 1 10 Unacceptable B 0 10 Acceptable -1 10 -2 10 -2 10 -1 10 0 10 Fold Change From Base Htot 1 10 Most Important Results! 2 10 Kinetic Dependence on “ECM” Parameters Plot of Time to 80% Steady State This point takes >10 Years!!! 4000 3500 3000 2500 2000 1500 1000 •Hereditary multiple exostoses (HME) •Simpson-Golabi-Behmel syndrome (SGBS) •Diastrophic dysplasia 500 0 2 10 2 1 10 10 1 10 0 10 0 10 -1 10 -1 10 -2 Fold Change From Base D 10 -2 10 Fold Change From Base htot Most Important Results! Results: Sensitivity to parameters Parameter Gradient Time to S.S. v + + kdeg + + kint + + Rtot + + Htot - + D + + Experiments: in vitro Investigate and characterize base state/ parameters Use chondrocyte cultures to better characterize cellsurface and ECM HSGAG using capillary electrophoresis Identify ranges of binding sites using surface noncovalent affinity mass spectrometry. Attempt organ culture to measure in vivo parameters (Keiser, 2001, Nature Medicine) Experiments: in vivo Validate model and model predictions Test with exogenous delivery of saccharides and proteins. Heparin-alginate spheres could be used for FGF2 or recombinant FGF2 mutant delivery Sodium chlorate to inhibit sulfation of HSGAG Knock-out mice/RNAi Targeted delivery of GAG modifying enzymes to subsets of chondrocytes Heparin release over time using alginate (Edelman, 2000, Biomaterials) Proposed future model directions Expand to other relevant FGF family members: FGF7, FGF8 FGF17, FGF18. Complicate model by simulating growth (moving source, semi-infinite domain) Make predictions about sources of pathologies with known phenotypes but unknown causes Use in silico testing to gauge potential efficacy of treatments for growth plate related pathologies Conclusions Our model is predictive of qualitative physiological and pathological conditions at the growth plate Our model suggests that a previous assumption that ECM binding could be lumped into an “effective” diffusivity may be incorrect Experimental testing and validation of the model is required to determine quantitative accuracy The model can suggest treatments for pathologies The model can be expanded to other systems References 1 Ornitz, D.M.a.M., P.J., FGF signaling pathways in endochondral and intramembranous bone development and human genetic disease. Genes and Development, 2002. 16: p. 1446-1465. 2. Erlebacher, A., Filvaroff, E.H., Gitelman, S.E., and Derynck, R., Toward a molecular understanding of skeletal development. Cell, 1995. 80: p. 371-378. 3. Floyd, W.E., 3rd, Zaleske, D.J., Schiller, A.L., Trahan, C., and Mankin, H.J., Vascular events associated with the appearance of the secondary center of ossification in the murine distal femoral epiphysis. Journal of Bone and Joint Surgery of America, 1987. 69: p. 185-190. 4. Kosher, R.A., Kulyk, W.M., and Gay, S.W., Collagen gene expression during limb cartilage differentiation. Journal of Cell Biology, 1986. 102: p. 1151-1156. 5. Schmid, T.M.a.L., T.F., Immunohistochemical localization of short chain cartilage colalge (type X) in avian tissues. Journal of Cell Biology, 1985. 100: p. 598-605. 6. Mundlos, S.a.O., B.R., Heritable diseases of the skeleton. Part I: Molecular insights into skeletal development transcription factors and signaling pathways. FASEB Journal, 1997. 11: p. 125-132. 7. Mundlos, S.a.O., B.R., Heritable diseases of the skeleton. Part II: Molecular insights in skeletal developmentmatrix components and their homeostasis. FASEB Jounral, 1997. 11(227-233). 8. Hall, B.K.a.M., T., The membranous skeletonL The role of cell condensations in certebrate skeletogenesis. Anatomy and Embryology, 1992. 186: p. 107-124. 9. Olsen, B.R., Reginato, A.M., and Wang, W., Bone development. Annual Reviews in Cell Developmental Biology, 2000. 16: p. 191-220. 10. Peters, K., Werner, S., Chen, G., and Williams, L.T., Two FGF receptor gene are differentially expressed in epithelial and mesenchymal tissues during limb formation and organogenesis on the mouse. Development, 1992. 144: p. 233-243. 11. Deng, C., Wynshaw-Boris, A., Zhou, F., Kuo, A. and Leder, P., Fibroblast growth factor receptor 2 is a negative regulator of bone growth. Cell, 1996. 84: p. 911-921. 12. Shiang, R., Thompson, L.M., Zhu, Y.Z., Church, D.M., Fielder, T.J., Bocian, M., Winokur, S.T., and Wasmuth, J.J., 1. Mutations in the transmembrane domain of FGFR3 cause the most common genetic form of dwarfism, achondroplasia. Cell, 1994. 78(2): p. 335-342. 13. Rousseau, F., Bonaventure, J., Legeal-Mallet, L., Pelet, A., Rozet, J.M., Marteaux, P., Merrer, M.L., and Munnich, A., Mutations in the gene encoding fibroblast growth factor receptor-2 in achondroplasia. Nature, 1994. 371: p. 254256. References 2 14. Sullivan, R.a.K., M., Puriifaction of cartilage-derived growth factor by heparin affinity chromatography. Journal of Biological Chemistry, 1985. 260: p. 2399-2403. 15. Xu, J., Lawshe, A., MacArthur, C.A., and Orntiz, D.M., Genomic structure, apping, activity and expression of fibroblast growth factor 17. Mechanisms of Development, 1999. 83: p. 165-178. 16. Liu, Z., Xu, J., Colvin, J,S,m and Ornitz, D.M., Coordination of chrondrogenesis and osteogenesis by fibroblast growth factor 18. Genes and Development, 2002. 16: p. 859-869. 17. Martin, G.R., The roles of FGFs in the early development of vertebrate limbs. Genes and Development, 1998. 12: p. 1571-1586. 18. Jingushi, S., Scully, S.P., Joyce, M.E., Sugioka, Y., and Bolander, M.E., Transforming growth factor-beta 1 and fibroblast growth factors in rat growth plate. Journal of Orthopedic Research, 1995. 13: p. 761-768. 19. Nagai, H., Tsukuda, R., and Mayahara, H., Effects of basic fibroblast growth factor (bFGF) on bone formation in growing rats. Bone, 1995. 16: p. 367-373. 20. Mancilla, E.E., De Luca, F., Uyeda, J.A., Czerwiec, F.S., and Baron, J., Effects of fibroblast growth factor-2 on longitudinal bone growth. Endocrinology, 1998. 139: p. 2900-2904. 21. Wezeman, F.H.a.B., M.R., Immunohistochemical localization of fibroblast growth factor-2 in nomral and brachymorphoc mouse tibial growth plate. Histochemical Journal, 1997. 29(6): p. 505-514. 22. Leach, R.M.J., Sokol, C., and McMurtry, J.P., Immunolocalization of basic fibroblast growth factor in porcine epiphyseal growth plate. Domestic Animal Endocrinology, 1997. 14(2): p. 129-132. 23. Lander, A.D., Nie, Q., and Wan, F.Y.M., Do Morphogen Gradients Arise by Diffusion? Developmental Cell, 2002. 2: p. 785-796. 24. Conrad, H.E., Heparin-Binding Proteins. 1998, San Diego: Academic Press. 25. Binari, R.C., Staveley, B.E., Johnson, W.A., Godavarti, R., Sasisekharan, R., and Manoukian, A.S., Genetic evidence that heparin-like glycosaminoglycans are involved in wingless signaling. Development, 1997. 124: p. 2623-2632. 26. Perrimon, N., and Bernfield, M., Specificities of heparan sulphate proteoglycans in developmental processes. Nature, 2000. 404(6779): p. 725-728. 27. Tumova, S., Woods, A., and Couchman, J.R., Heparan sulfate proteoglycans on the cell surface: versatile coordinators of cellular functions. International Jounral of Biochemistry and Cellular Biology, 2000. 32(3): p. 269288. References 3 28. Nurcombe, V., Smart, C.E., Chipperfield, H., Cool, S.M., Boilly, B., and Hondermarck, H., The proliferative and migratory activities of breast cancer cells can be differentially regulated by heparan sulfates. Journal of Biological Chemistry, 2000. 275(39): p. 30009-30018. 29. Shriver, Z., Liu, D., and Sasisekharan, R., Emerging views of heparan sulfate glycosaminoglycan structure/activity relationships modulating dynamic biological functions. Trends in Cardiovascular Medicine, 2002. 12(2): p. 71-77. 30. Klagsbrun, M., and Baird, A., A dual receptor system is required for basic fibroblast growth factor activity. Cell, 1991. 67: p. 229-231. 31. Schlessinger, J., Lax, I., and Lemon, M., Regulation of growth factor activation by proteoglycans: what is the role of the low affinity receptors? Cell, 1995. 83: p. 357-360. 32. Venkataraman, G., Sasisekharan, V., Herr, A.B., Ornitz, D.M., Waksman, G., Cooney, C.L., Langer, R., and Sasisekahran R., Preferential self-association of basic fibroblast growth factor is stabliszed by heparin during receptor dimerization and activation. Proceedings of the National Academy of Sciences USA, 1996. 93: p. 845850. 33. Sperinde, G.V.a.N., M.A., Mechanisms of Fibroblast Growth Factor 2 Intracellular Processing: A Kinetic Analysis of the Role of Heparan Sulfate Proteoglycans. Biochemistry, 2000. 39: p. 3788-3796. 34. Brown, M.S., ANderson, G.W., and Goldstein, J.L., Recycling receptors: the round-trip itinerary of migrant membrane proteins. Cell, 1983. 32: p. 663-667. 35. Sperinde, G.V., and Nugent, M.A., Heparan sulfate proteoglycans control intracellular processing of bFGF in vascular smooth muscle cells. Biochemistry, 1998. 37: p. 13153-13164. 36. Hawker, J.R.a.G., H.J., Internalized basic fibroblast growth factor translocates to nuclei of venular endothelial cells. American Journal of Physiology, 1992. 262: p. H1525-H1537. 37. Padera, R., Venkataraman, G., Berry, D., Godvarti, R., and Sasisekharan, R., FGF-2/fibroblast growth factor receptor/heparin-like glycosaminoglycan interactions: a compensation model for FGF-2 signaling. FASEB Journal, 1999. 13(13): p. 1677-1687. 38. Bikfalvi, A., Klein, S., Pintucci, G., and Rifkin, D.B., Biological roles of fibroblast growth factor-2. Endocrinology Reviews, 1997. 18: p. 26-45. 39. Johnson, D.E.a.W., L.T., Structural and functional diversity in the FGF receptor multigene family. Advances in Cancer Research, 1993. 60: p. 1-41. References 4 40. Zandstra, P.W., Lauffenburger, D.A., and Eaves, C.J., A ligand-receptor signaling threshold model of stem cell differentiation control: a biologically conserved mechanism applicable to heamotpoiesis. Blood, 2000. 96(4): p. 1215-1222. 41. Yayon, A., Klagsbrun, M., Esko, J.D., Leder, P., and Ornitz, D.M., Cell surface, heparin-like molecules are required for binding of basic fibroblast growth factor to its high affinity receptor. Cell, 1991. 64(4): p. 841-848. 42. Kan, M., Wang, F., Xu, J., Crabb, J.W., Hou, J., and McKeehan, W.L., An essential heparin-binding domain in the fibroblast growth factor receptor kinase. Science, 1993. 259: p. 1918-1921. 43. Moscatelli, D., Basic fibroblast growth factor dissociates rapidly from heparan sulfates but slowly from receptors. Implications for mechanisms of bFGF release from pericellular matrix. Journal of Biological Chemistry, 1992. 267(36): p. 25803-25809. 44. Turnbull, J.E., Fernig, D.G., Ke, Y., Wilkinson, M.C., and Gallagher, J.T., Identification of the basic fibroblast growth factor binding sequence in fibroblast heparan sulfate. Journal of Biochemical Chemistry, 1992. 267(15): p. 10337-10341. 45. Maccarana, M., Casu, B., and Lindahl, U., Minimal sequence in heparin/heparan sulfate requried for binding of basic fibroblast growth factor. Journal of Biological Chemistry, 1993. 268(32): p. 23898-23905. 46. Wang, H., Toida, T., Kim, Y.S., Capila, I., Hilemna, R.E., Berfield, M., and Lundhard, R.J., Glycosaminoglycans can induce fibroblast growth factor-2 mitogenicity without significant growth factor binding. Biochemical and Biophysical Research Communcations, 1997. 235: p. 369-373. 47. Ishihara, M., Kariya, Y., Hayashi, K., Hara, S., Kikuchi, H., and Yoshida, K., Importance of 6-O sulfate groups of glucosamine residues in heparin for activation of FGF-1 and FGF-2. Journal of Biochemistry (Tokyo), 1995. 118(1255-1260). 48. Lundin, L., Larsson, H., Kreuger, J., Kanda, Lindahl, U., Salmivirta, M., and Claesson-Welsh, L., Selectively desulfated heparin inhbits fibroblast growth factor-induced mitogenicity and angiogenesis. Journal of Biological Chemistry, 2000. 275(32): p. 24653-24660. 49. Tanihara, M., Suzuki, Y., Yamamoto, E., Noguchi, A., and Mizushima, Y., Sustained relase of basic fibroblast growth factor and angiogenesis in a novel covalently crosslinked gel of heparin and alginate. Journal of Biomedical Materials Research, 2001. 56(2): p. 216-221. 50. Nugent, M.A., Karnovsky, M.J., and Edelman E.R., Vascular cell-derived heparan sulfate shows coupled inhbition of basic fibroblast growth factor binding and mitogenesis in vascular smooth muscle cells. Circulation Research, 1993. 73(6): p. 1051-1060. References 5 51. Forsten, K.E., Courant, N.A., and Nugent, M.A., Endothelial proteoglycans inhibit bFGF binding and mitogenesis. Journal of Cellular Physiology, 1997. 172(2): p. 209-220. 52. Fannon, M., Forsten, K.E., and Nugent, M.A, Potentiation and inhibition of bFGF binding to heparin: a model for regulation of cellular response. Biochemistry, 2000. 39(6): p. 1434-1445. 53. Keller, K.M., Brauer, P.R., and Keller, J.M., Modulation of cell surface heparan sulfate structure by growth of cells in the presence of chlorate. Biochemistry, 1989. 28(20): p. 8100-8107. 54. Coffin, J.D., Florkiewixz, R.Z. Neumann, J., Mort-Hopkins, T., Dornll, G.W., Lightfoot, P., German, R., Howles, P.N., Kier, A., O'Toole, B.A., Sasse, J., Gonzalez, A.M., Baird, A., and Doetschman, T., Abnormal bone growth and selective translational regulation in basic fibroblast growth factor (FGF-2) transgenic mice. Molecular Biology of the Cell, 1995. 6: p. 1861-1873. 55. Ponnazhagan, S., Mehendra, G., Kumar, S., Thompson, J.A., and Castillas, M. Jr., Conjugate-Based Targeting of Recombinant Adeno-Associated Virus Type 2 Vectors by Using Avidin-Linked Ligands. Journal of Virology, 2002. 76(24): p. 12900-12907. 56. Keiser, N., Venkataraman, G., Shriver, Z., and Sasisekharan, R., Direct isolation and sequencing of specific protien-binding glycosaminoglycans. Nature Medicine, 2001. 7(1): p. 123-128. 57. Ornitz, D.M., Xu, J., Colvin, J.S., McEwen, D.G., MacArthur, C.A., Coulier, F., Gao, G., and Goldfarb, M., Receptor specificity of the fibroblast growth factor family. Journal of Biological Chemistry, 1996. 271(25): p. 15292-15297.