Respiratory Infections including Tuberculosis
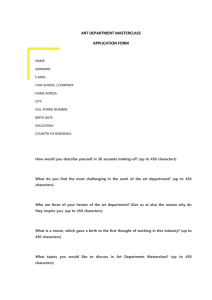
advertisement

Respiratory Infections including Tuberculosis Dr Terry O’Connor Mercy University Hospital Cork Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient 62-yr male smoker Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient 29-yr homeless male Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient 34-yr HIV+ South African male • Pulmonary Tuberculosis • Sputum cultures – Resistant • • • • • Rifampicin Isoniazid Pyrazinamide Ethambutol Streptomycin – Sensitive • Amikacin • Capreomycin • Ciprofloxacin • Clarithromycin • Cycloserine • Ethionamide Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Multiple Choice Questions • The commonest cause of respiratory death in Ireland is: – – – – a) b) c) d) Lung Cancer Pneumonia COPD Hermansky-Pudlak syndrome Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Multiple Choice Questions • The incidence of tuberculosis in Ireland is: – – – – a) b) c) d) Increasing Remaining constant Decreasing Fluctuating Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Multiple Choice Questions • Tuberculous pleural effusions are characterised by: – – – – a) b) c) d) Negative Mantoux tests in > 70% Pleural fluid neutrophil predominance High pleural fluid adenosine deaminase activity Low pleural fluid protein content Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pneumonia Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Respiratory Deaths by Cause, 2004 Total Deaths 6007 Pneumonia Respiratory Cancers COPD 1973 (33%) 1692 (28%) 1417 (24%) Brennan N, McCormack S, O’Connor T. INHALE. 2008. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pneumonia • Definition by Microbes – – – – Bacterial – Pneumococcal, Streptococcal Atypical pathogens Fungal Viral • Definition by Location – – Lobar pneumonia Bronchopneumonia • Definition by Acquisition – – – Community acquired pneumonia Hospital acquired pneumonia Ventilator-associated pneumonia Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Bronchopneumonia vs Lobar Pneumonia Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pneumonia RUL RML RLL LUL LLL Aspiration Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pathogens in CAP • Bacteria – – – – – Streptococcus pneumoniae Haemophilus influenzae Staphylococcus aureus Gram negative bacilli Miscellaneous • Atypical Agents – Legionella – Mycoplasma pneumoniae – Chlamydia pneumoniae • Viruses • Aspiration 50-60% 5-10% 2-5% 2% 3-5% 10-20% 2-5% 5-10% 5% 2-15% 5-10% Streptococcus pneumoniae Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Typical Atypical • • • • • • • • • • • • • Sudden onset Toxic patient appearance Productive cough High fever (>39 C) Elevated WBC with left shift Sputum - bugs Defined consolidation Slow onset Patient appears relatively well Non-productive or dry cough No left shift in WBC Sputum - no bugs Interstitial or patchy infiltrate Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Streptococcus pneumonia • Most common cause of CAP • Gram positive diplococci • “Typical” symptoms (e.g. malaise, shaking chills, fever, rusty sputum, pleuritic hest pain, cough) • Lobar infiltrate on CXR • 25% bacteremic Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Atypical Pneumonia • Second commonest cause (especially in younger population) • Commonly associated with milder symptoms: subacute onset, nonproductive cough, absence of focal infiltrate on CXR • Mycoplasma: younger patients, extra-pulmonary symptoms (anemia, rashes), headache, sore throat • Chlamydia: year round, upper respiratory symptoms, sore throat • Legionella: higher mortality rate, water-borne outbreaks, hyponatremia, diarrhoea Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pathogens in HAP • Bacteria – – – – – – Pseudomonas aeruginosa Staphylococcus aureus (MRSA) Gram negative bacilli Streptococcus pneumoniae Haemophilus influenzae Polymicrobial 25-30% 25% 25% 3-5% 3-5% 10-20% • Atypical Agents – Legionella 2-5% • Fungi (Aspergillus / Candida) 5-10% • Aspiration 5-10% Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pneumonia patient characteristics • Alcoholism: S. pneumoniae, oral anaerobes, Klebsiella, Acinetobacter species, MTB • Smoker/COPD: S. pneumoniae, H. influenzae, Moraxella catarrhalis, Pseudomonas, Legionella • Aspiration: Gram-negative enteric pathogens, oral anaerobes • Lung Abscess: MRSA, oral anaerobes, endemic fungal pneumonia, MTB, atypical mycobacteria • Exposure to birds: Chlamydophilia psittaci (if poultry, avian influenza) • Exposure to farm animals or parturient cats: Coxiella burnetti (Q fever) • Hotel or cruise ship in previous 2 weeks: Legionella species Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pneumonia patient characteristics • HIV infection: Early - S. pneumoniae, H. influenzae, MTB Late – Pneumocystis, Cryptococcus, Histoplasma, Aspergillus, Atypical mycobacteria • Post viral bronchitis: S. pneumoniae, Staphylococcus aureus, H. influenzae • IV drug user: S. aureus, anaerobes, M. tuberculosis, S. pneumoniae • Structural lung disease (eg. Bronchiectasis): Pseudomonas aeruginosa, Burkholderia cepacia, S. aureus • Endobronchial obstruction: Anaerobes, S. pneumoniae, H. influenzae, S.aureus Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Antimicrobial Therapy for Specific Pathogens Organism Preferred antimicrobial(s) Alternative antimicrobial(s) Streptococcus pneumoniae Penicillin nonresistant; MIC !2 mg/mL Penicillin G, amoxicillin Macrolide, cephalosporins, clindamycin, doxycyline, respiratory fluoroquinolone Vancomycin, linezolid, high-dose amoxicillin Penicillin resistant; MIC 2 mg/mL Agents chosen on the basis of susceptibility, including cefotaxime, ceftriaxone, fluoroquinolone Haemophilus influenzae Non–β-lactamase producing β-Lactamase producing Amoxicillin Fluoroquinolone, doxycycline, azithromycin, clarithromycin Second- or third-generation cephalosporin, amoxycillinclavulanate Fluoroquinolone, doxycycline, azithromycin, clarithromycin Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases 2007; 44:S27–72. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Antimicrobial Therapy for Specific Pathogens Organism Preferred antimicrobial(s) Alternative antimicrobial(s) Mycoplasma pneumoniae Macrolide, a tetracycline Fluoroquinolone Legionella species Fluoroquinolone, azithromycin Doxycyline Chlamydophila psittaci A tetracycline Macrolide Coxiella burnetii A tetracycline Macrolide Yersinisa pestis Streptomycin, gentamicin Doxycyline, fluoroquinolone Bacillus anthracis (inhalation) Ciprofloxacin, levofloxacin, doxycycline Other fluoroquinolones; β-lactam, if susceptible; rifampin; clindamycin; chloramphenicol Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases 2007; 44:S27–72. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Antimicrobial Therapy for Specific Pathogens Organism Preferred antimicrobial(s) Alternative antimicrobial(s) Pseudomonas aeruginosa Antipseudomonal β-lactam plus (ciprofloxacin or levofloxacin or aminoglycoside) Aminoglycoside plus (ciprofloxacin or levofloxacin) Methicillin susceptible Antistaphylococcal penicillin Cefazolin, clindamycin Methicillin resistant Vancomycin or linezolid TMP-SMX β-Lactam/ β-lactamase inhibitor, clindamycin Oseltamivir or zanamivir Carbapenem Staphylococcus aureus Anaerobe (aspiration) Influenza virus Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases 2007; 44:S27–72. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Tests for Pneumonia • • • • • • • • • • Chest Radiograph Arterial Blood Gas Complete Blood Count Chemistry – Electrolytes, Renal function, Liver function Serologic Testing (Atypical pneumonia screen) Blood Culture Sputum Gram stain and culture, AFB Pneumococcal Urinary Antigen Legionella Urinary Antigen Pleural fluid analysis Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Poor prognostic features • Age > 65 years • Coexisting disease Diabetes, renal / heart failure, neoplasia, others • Clinical findings RR > 30/min, SBP < 90mmHg, T > 38.3oC Altered mental status • Lab tests WCC low or very high, Haematocrit < 30% Low pO2 Renal failure Multilobar involvement on CXR, pleural effusion • Microbial pathogens Streptococcus pneumoniae Legionella pneumophilia Staphylococcus aureus Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient CURB-65 • • • • • C = Confusion U = Urea > 7mmol/L R = Respiratory rate >/= 30/min B = BP systolic < 90mmHg or diastolic </=60mmHg 65 = Age >/= 65 years Score one point for each feature present • 0 or 1- low risk of death, non-severe pneumonia, home treatment • 2 – increased risk of death, consider short inpatient stay or hospital supervised outpatient treatment • 3 or more – high risk of death and should be managed as having severe pneumonia Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Non-invasive ventilation • CPAP may be of value in selected patients with hypoxic respiratory failure but good evidence lacking • BiPAP of more established benefit in patients with hypercapnic respiratory failure, particularly those with COPD Delclaux et al. JAMA 2000;284:2352-2360. Cochrane Database Syst Rev. 2004;CD004104. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Aspiration Pneumonia Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Lung Abscess Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Lung Abscess Pathophysiology • Localized necrotic lesion of the lung parenchyma containing purulent material • Lesion collapses and forms a cavity Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Lung Abscess • Aetiology – Aspiration – Staphylococcal aureus – Klebsiella – Anaerobic organisms • Antimicrobial Therapy – 4-6 weeks Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Tuberculosis Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient The White Plague Much Ado About Nothing (1600), Macbeth (1606) Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient ‘Patricia’ Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient TB incidence in Ireland Tuberculosis in Ireland Incidence / 100,000 population 250 200 150 Ireland 100 50 2001 2000 1999 1998 1997 1996 1995 1994 1993 1992 1990 1982 1972 1962 1952 0 Year Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Incidence / 100,000 population 30 TB incidence in Ireland 25 20 Ireland Irish 15 10 5 0 1991 1993 1995 1997 1999 2001 2003 2005 Year Health Protection Surveillance Centre Ireland 2008 Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Transmission of M. tuberculosis Risk factors for progression – HIV infection – Diabetes mellitus – Acquisition of LTBI in infancy or early childhood – Apical fibronodular changes on chest radiograph – Use of agents that antagonize the effect of tumor necrosis factor- Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Transmission of M. tuberculosis Musher DM. N Engl J Med 2003;348:1256-66. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Transmission of M. tuberculosis • Characteristics of the source-case – Concentration of organisms in sputum – Presence of cavitary disease on chest radiograph – Frequency and strength of cough • Characteristics of the exposed person – Previous M. tuberculosis infection – Innate / genetic susceptibility to M. tuberculosis infection • Characteristics of the exposure – Frequency and duration of exposure – Dilution effect (i.e., the volume of air containing infectious droplet nuclei) – Ventilation (i.e., the turnover of air in a space) – Exposure to ultraviolet light, including sunlight • Virulence of the infecting strain of M. tuberculosis Controlling tuberculosis in the United States. Am J Respir Crit Care Med. 2005 Nov 1;172:1169-227 Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Susceptibility to tuberculosis • Polymorphism within the interferon gamma/receptor complex is associated with pulmonary tuberculosis. • Recurrent tuberculosis in the United States and Canada is rarely due to reinfection with a new strain of M. tuberculosis. • Incidence rate of tuberculosis attributable to reinfection after successful treatment could be four times that of new tuberculosis in an area with high prevalence of disease, such as South Africa. Cooke GS, et al. Am J Respir Crit Care Med. 2006 EPub May 11. Jasmer RM et al. Am J Respir Crit Care Med. 2004;170:1360-6. Verver S, et al. Am J Respir Crit Care Med 2005;171:1430–1435. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Symptoms of TB infection – Cough – Sputum – Haemoptysis – Weight loss – Night sweats Key issues in the diagnosis and management of tuberculosis Milburn J R Soc Med.2007; 100: 134-141 Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Asymptomatic 100 Symptomatic Patients 50 0 Pleural TB Pulmonary TB LTBI Jahangir A, et al. Ir J Med Sci (Suppl) 2008 Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Diagnosis of tuberculosis • Mycobacterium tuberculosis is discovered in the laboratory by one of two methods: – Acid and alcohol fast bacilli stain (also called AFB or smear). TB specimens which contain a lot of TB organisms are often AFB positive. – Tuberculosis culture – TB is very slow growing so, unlike bacterial infections, it may be 1012 weeks before the results are reported. TB specimens which contain very few TB organisms are often AFB negative but culture positive. Ziehl-Nielsen Staining Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient False TST Reactions Positive • Nontuberculous mycobacteria • BCG vaccination Negative • • • • • • • Anergy Poor nutrition Immunosuppressive drugs Recent TB infection (2-10 wks) Very young / old age Malignancy Live virus vaccination (measles, smallpox) • Overwhelming TB disease • Poor TST administration Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Interferon Gamma Release Assays • Rapidly replacing the Mantoux test in developed economies • More specific than Mantoux for diagnosis of TB infection • Preventing thousands of treatments for latent TB infection Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Species specificity of ESAT-6 and CFP-10 Tuberculosis complex Antigens ESAT M tuberculosis + M africanum + M bovis + BCG substrain gothenburg - moreau - tice - tokyo - danish - glaxo - montreal - pasteur - Respiratory Medicine Session Environmental strains Antigens ESAT CFP CFP M abcessus M avium + M branderi M celatum + M chelonae + M fortuitum M gordonii M intracellulare M kansasii + + M malmoense M marinum + + M oenavense M scrofulaceum M smegmatis M szulgai + + M terrae M vaccae M xenopi of the RCPI Masterclass on Treating the Acutely Ill Patient Treatment of Tuberculosis Millet Seeds. The term "miliary tuberculosis" derives from the resemblance of the granulomatous nodules to millet seeds Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Current Antituberculous Drugs First-Line Drugs Second-Line Drugs • Isoniazid • Streptomycin • Rifampicin • Cycloserine • Pyrazinamide • p-Aminosalicylic acid • Ethambutol • Ethionamide • Rifabutin • Amikacin • Rifapentine • Kanamycin • Capreomycin • Levofloxacin • Moxifloxacin • Gatifloxacin • Clarithromycin Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Recommended Treatment Regimens Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Combination Agents • • • • • Rifampicin Isoniazid Pyrazinamide Ethambutol Pyridoxine • Rifampicin • Isoniazid • Pyridoxine • Rifater 5 tabs OD • Ethambutol 1.2g OD • Pyridoxine 25 mg OD 2 months • Rifinah ‘300’ 2 tabs OD • Pyridoxine 25 mg OD 4-7 months Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient New Antituberculous Drugs Diarylquinolones R207910 Trans-Cinnamic Acid Quinolones Ofloxacin Levofloxacin Moxifloxacin Pyrroles BM212 Oxazolidinones Linezolid RBx 7644 RBx 8700 Macrolides Clarithromycin Azithromycin Roxithromycin Nitroimidazopyrans PA-824 OPC-67683 Newer Rifamycins Rifabutin Rifapentine Rifalazil Ethambutol Analogues SQ109 Aerosolized interferon gamma Barry PJ, O’Connor TM. Current Medicinal Chemistry 2007;14:2000-8. Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Determining when during therapy a patient is noninfectious • Patient has negligible likelihood of multidrug-resistant TB • Patient has received standard multidrug anti-TB therapy for 2– 3 weeks • Patient has demonstrated complete adherence to treatment and evidence of clinical improvement • All close contacts of patient have been identified, evaluated, advised, and, if indicated, started on treatment for latent TB infection Controlling tuberculosis in the United States. Am J Respir Crit Care Med. 2005 Nov 1;172:1169-227 Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient In the Emergency Department • Active infectious TB should not be managed in the ED • Isolate if active infectious TB suspected, negative pressure room ideally • Staff wear FFP2 masks (N95 equivalent) • Do not start empiric therapy • Sputum x 3, consider bronchoscopy, Mantoux, Quantiferon • If sputum AFB +, initiate therapy, HIV test, visual acuity and baseline LFTs, contact public health to initiate contact tracing Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pulmonary Tuberculosis Sputum ZN positive Rx Rifater Ethambutol Pyridoxine Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pulmonary Tuberculosis Sputum ZN negative Bronchoscopy / Washings RUL Rx Rifater Ethambutol Pyridoxine Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Pulmonary Tuberculosis Miliary Tuberculosis Sputum ZN positive Rx Rifater Ethambutol Pyridoxine Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Tuberculous Pleurisy Mantoux positive Pleural fluid analysis – 90% lymphocytes High adenosine deaminase (ADA) activity Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Multiple Choice Questions • The commonest cause of respiratory death in Ireland is: – – – – a) b) c) d) Lung Cancer Pneumonia COPD Hermansky-Pudlak syndrome Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Multiple Choice Questions • The incidence of tuberculosis in Ireland is: – – – – a) b) c) d) Increasing Remaining constant Decreasing Fluctuating Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Multiple Choice Questions • Tuberculous pleural effusions are characterised by: – – – – a) b) c) d) Negative Mantoux tests in > 70% Pleural fluid neutrophil predominance High pleural fluid adenosine deaminase activity Low pleural fluid protein content Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient Thank you Questions Respiratory Medicine Session of the RCPI Masterclass on Treating the Acutely Ill Patient