Leadership Strategy Analysis: Improving Patient
advertisement

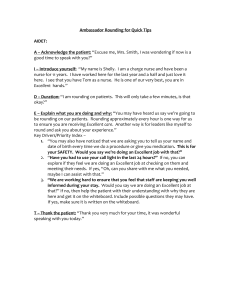
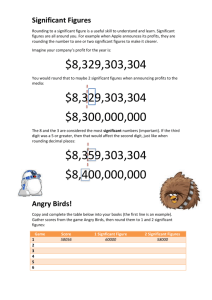
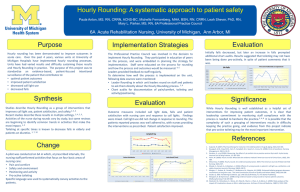
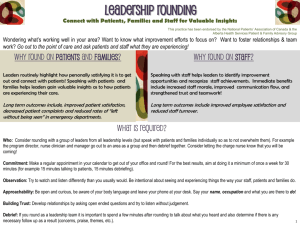
Running head: LEADERSHIP STRATEGY ANALYSIS Leadership Strategy Analysis: Improving Patient Outcomes One Hour at a Time Amanda Chappel, Trisha Mast, and Jennifer Stankevich Ferris State University 1 LEADERSHIP STRATEGY ANALYSIS 2 Abstract The Internet, technology, enhanced mobility, changes in insurance reimbursement criteria, and improved consumer knowledge have placed renewed emphasis on patient satisfaction in the health care industry. Hourly rounding has been one proposed method of improving patient satisfaction scores. Hourly rounding is associated with reduced patient falls and development of pressure ulcers, improved patient satisfaction and enhanced nurse satisfaction. LEADERSHIP STRATEGY ANALYSIS 3 Leadership Strategy Analysis: Improving Patient Outcomes One Hour at a Time Throughout history customer satisfaction has been at the forefront of quality improvement initiatives in the United States. This is because, according to Yoder-Wise (2015), “Customers define quality” (p. 366). Patients have started to see themselves as consumers who can take their business elsewhere (Yoder-Wise, 2015). The Internet, sophisticated technology, healthcare transparency, and consumer mobility have enhanced healthcare options. If consumers are not happy with the quality of their healthcare, they can simply take their business elsewhere. This coupled with recent changes in the health care system and insurance reimbursement criteria have lead healthcare leaders to further research and trial methods of improving patient outcomes, safety, and satisfaction. The quality improvement process involves, continual analysis and evaluation of products and services utilized to reduce errors and improve patient outcomes to achieve improved patient satisfaction (Yoder-Wise, 2015). Hourly rounding has been one proposed method of improving patient satisfaction scores. It is hypothesized that hourly bedside rounding is a proactive method of anticipating and meeting patient needs regularly and ensuring their safety (Ford, 2010). Hourly rounding is a structured, and intentional method of gathering information and addressing problems before they occur or worsen (Ford, 2010). Clinical Need The Internet, technology, enhanced mobility, and improved consumer knowledge have placed renewed emphasis on patient satisfaction in the health care industry. Health care organizations are continually seeking and researching new approaches to improve patient satisfaction scores (Ford, 2010). According to Ford (2010), “Patients value the nurse-patient relationship, as well as time spent with them, continuity of care, trust, compassion, respect, LEADERSHIP STRATEGY ANALYSIS 4 safety, understandable instructions, and service quality. They also appreciate reliability, responsiveness, and effective communication” (p. 188). Patient satisfaction scores are also a key component in healthcare facility ratings, percentage of reimbursement, and community reputation (Mitchell, Lavenberg, Trotta, & Umscheid, 2014). Bedside rounding is one quality improvement initiative that has been suggested to improve patient satisfaction, safety, and outcomes. Uniquely, bedside rounding is a component of every nurse’s practice. However, policies and procedures surrounding bedside rounding requirements vary between healthcare facilities. It is proposed that implementation of hourly bedside rounding reduces patient falls, reduces adverse patient outcomes, increases patient satisfaction, and decreases the number of times a patient pushes their call bell each shift (Blakley, Kroth, & Gregson, 2011). In addition to positive patient outcomes, hourly rounding can potentially leave nurses with more time to chart without interruption, which reduces errors and improves clinical documentation (Blakley, Kroth, & Gregson, 2011). Multidisciplinary Team To achieve success in the quality improvement process, input is needed from all members of the healthcare team. For this reason, hourly bedside rounding is best achieved through a multidisciplinary approach. Gonzalo, Wolpaw, Lehman, & Chuang (2014) states, “Team-based care delivery with providers of different professions functioning as one unit enhances communication, coordination, and patient-centered shared-decision making, potentially improving process measures and patient-level outcomes” (p. 1040). Physicians Many times, the physician is in and out of the room, and the patient feels uninvolved in their care. Physicians and residents can do their part in enhancing the patient experience by doing LEADERSHIP STRATEGY ANALYSIS 5 their clinical rounds in the patient’s room at the bedside instead of using a conference room. Physicians and patients reported a better understanding of education provided when done during bedside rounds (Gonzalo, Wolpaw, Lehman, & Chuang, 2014). Conducting provider rounds at the bedside also allows the nurse to be present, which enhances continuity of care (Ford, 2010). Registered nurses Registered nurses have the biggest and most important role in bedside rounding. Patients are unaware of the demands of their nurse throughout the shift; this creates a level of anxiety for patients when they don’t know how long the nurse will take to respond to their needs (Mitchell, Lavenberg, Trotta, & Umscheid, 2014). Nurses can alleviate some of this fear by making predictable rounds and addressing basic needs. The four “Ps” of basic patient needs are: position, pain control, proximity to personal items, and bathroom needs [“potty”] (Mitchell, Lavenberg, Trotta, & Umscheid, 2014). Patients are less likely to push their call button, and more likely to be satisfied with their overall experience when they feel that their personal needs are attended to. In addition to feeling taken care of, patients who anticipate hourly rounding are less likely to fall, because they know that the nurse, or another member of the health care team, will be in to check on them in the next hour (Mitchell, Lavenberg, Trotta, & Umscheid, 2014). Certified nursing assistants Certified nursing assistants (CNAs) are responsible for many patient care tasks. They assist in passing and picking up meal trays, performing vitals, repositioning patients, encouraging and assisting in ambulation, helping patients with activities of daily living, and function as a liaison between the patient and the nurse. The CNA is a key player in effective hourly patient rounding. Risk manager LEADERSHIP STRATEGY ANALYSIS 6 The risk manager’s function is to identify risks and provide opportunities to improve care (Yoder-Wise, 2015). The risk manager’s role will be to obtain historical data, provide evidencebased practice (EBP) for staff, measure employee compliance, and measure the effectiveness of bedside rounding. Effectiveness can be measured in terms of patient safety data such as reduced falls, reduced adverse patient outcomes, and improved patient satisfaction scores. The risk manager will implement surveys to nursing staff to measure nurse satisfaction and potential process improvements before and after implementation of hourly rounding. The risk manager will also be in charge of working with the unit manager and reviewing patient satisfaction surveys. Specifically it is the risk managers role to take patient satisfaction survey results and transpose the data onto a comparative risk analysis graph that identifies patient satisfaction scores, number of patient falls and adverse patient outcomes before and after implementation of hourly bedside rounding. Charge nurse The charge nurse will monitor hourly rounding and compliance according to policy, provide support to the staff during the change, and assist in rounding during the transition. The charge nurse will work with the risk manager in communicating concerns of employees, convey patient feedback, and assist in identification of actual and potential barriers to action. Assessing barriers on the floor will increase compliance while alleviating the barriers will aid in success of implementing hourly bedside rounding (Shepard, 2013). Unit manager The unit manager and risk manager will work together to develop a script and tactics for hourly bedside rounding. Better patient outcomes are achieved through provision of a script and tactics for employees to utilize during the initial implementation phase of the bedside rounding LEADERSHIP STRATEGY ANALYSIS 7 quality improvement initiative (Ford, 2010). Patient satisfaction surveys will be distributed to patients within two weeks discharge. Evaluation of patient satisfaction surveys will be handled by the unit manager and reviewed with the risk manager. Data Collection Method Data will be collected from all nursing departments within the hospital. To focus on quality improvement, information will be collected specifically on the number of falls, level of patient satisfaction, adverse patient outcomes (specifically development of pressure ulcers and medication errors), as well as nurse and staff satisfaction. Fall data will be obtained through chart audits, while patient and nurse satisfaction reports will be collected via surveys. Comparison/relationship charts will be utilized to evaluate multiple variables: falls, medication errors and pressure ulcers over a quarterly and yearly time period; specifically line charts. Bar graphs will be used to display compliance data among the interdisciplinary team. Composition charts such as pie charts and line charts can be used to measure compliance rates for bedside rounding. According to Yoder-Wise (2015), “The use of statistical tools enables nurse managers to make objective decisions about quality improvement activities” (p. 367). Composition charts, bar graphs, and comparison charts are uncomplicated, clear, decisive, and easy to read. They are great at displaying comparative data and trends over a period of time such as months or years (Yoder-Wise, 2015). Each unit will display their data in staff break rooms or lounge area for employees to see as well as reviewed at employee meetings and shared governance. Outcomes, Goals and Implementation Strategies Outcomes The quality improvement process includes planning, implementing, and evaluating changes in order to achieve positive patient outcomes (Yoder-Wise, 2015). By using this process, LEADERSHIP STRATEGY ANALYSIS 8 all members of the team can add to the planning, and be empowered to actively participate in the improvement process. After data is analyzed regarding: adverse patient outcomes, patient falls, patient and nurse satisfaction, and staff compliance, the success and effectiveness of bedside rounding can be measured. Goals Patient falls will decrease by 75% six months after implementation of hourly bedside rounding. Patient satisfaction surveys will conclude increase satisfaction with their hospital stay in six months. Nurse satisfaction will increase and staff turnover reduced in one year. Implementation strategies Hourly bedside rounding will begin with a multidisciplinary team training the floor staff on the objectives of the quality improvement initiative and how to proceed with implementation of the plan. One strategy to improve compliance is to communicate and educate the staff on evidence based practice and the “why” of quality improvement initiatives being sought. An integral component of communication in change initiatives is to not only provide the “what we are doing and why we are doing it”, but also actively listening to the concerns of the staff. While change may provoke resistance, communication will reduce barriers (Yoder-Wise, 2015). Once compliance is obtained, hourly bedside rounding can be implemented. Staff will need to be educated on how to perform hourly rounding. Expectations need to be defined, including the provision of scripts and tactics for staff to use during hourly rounds. Providing education, establishing expectations, and specifying scripts and tactics for use, helps improve consistency and continuity of patient care (Ford, 2010). LEADERSHIP STRATEGY ANALYSIS 9 Evaluation A pre-established team consisting of the unit manager, risk manager, charge nurse, and multiple floor nurses will evaluate hourly bedside rounding. Evaluation will be conducted on a bi-monthly basis. According to Yoder-Wise (2015), “As the plan is implemented, the team continues to gather and evaluate data to document that the new outcomes are being met. If an outcomes is not met, revisions in the implementation plan are needed” (p. 374). Often once a plan is initiated, new problems arise warranting changes to the process or procedures (YoderWise, 2015). It is imperative that floor audits be conducted to establish staff compliance as well as individual performance appraisals be conducted to address barriers to action, and potential areas for process improvement. Conclusion Hourly bedside rounding is a proactive method of anticipating and meeting patient needs regularly and ensuring their safety. It is a structured and intentional method of addressing problems before they occur or worsen (Ford, 2010). Hourly rounding has been shown to significantly reduce patient falls and the use of call lights, as well as improve patient satisfaction (Ford, 2010). The concept of hourly rounding addresses and applies Kolcaba’s comfort theory. With hourly rounding, the patients’ needs will be assessed and addressed hourly, relieving pain, anxiety and increasing comfort, ultimately allowing the patient to transcend to optimal function (Kolcaba, 2010). Consistent hourly rounding is a key quality improvement initiative for improving patient safety, satisfaction, and quality of care. LEADERSHIP STRATEGY ANALYSIS 10 References Blakley, D., Kroth, M., & Gregson, J. (2011). The impact of nurse rounding on patient satisfaction in a medical-surgical hospital unit. Medsurg Nursing, 20(6), 327-332. Fabry, D. (2015). Hourly rounding: perspectives and perceptions of the frontline nursing staff. Journal of Nursing Management, 23, 200-210. Ford, B. M. (2010). Hourly rounding: A strategy to improve patient satisfaction scores. MedSurg Nursing, 19(3), 188-192. Retrieved from: http://0-go.galegroup.com.libcat. ferris.edu/ps/i.do?&id=GALE%7CA230957261&v=2.1&u=lom_ferrissu&it=r&p=ITOF&sw=w &authCount=1 Gonzalo, J. D., Wolpaw, D. R., Lehman, E., & Chuang, C. H. (2014). Patient centered interprofessional collaborative care: Factors associated with bedside interprofessional rounds. Journal of General Internal Medicine, 29(7), 1040-1047. doi: 10.1007/s11606-014-2817-x Kolcaba, K. (2010). Comfort line: Conceptual framework for Comfort Theory. Retrieved from http://www.thecomfortline.com/index.html Mitchell, M. D., Lavenberg, J. G., Trotta, R. L., & Umscheid, C. A. (2014). Hourly rounding to improve nursing responsiveness: A systematic review. The Journal of Nursing Administration, 44(9), 462-472. doi: 10.1097/NNA.0000000000000101 Shepard, L. (2013). Stop going in circles! Break the barriers to hourly rounding. Nursing Management, 13-15. doi:10.1097/01.NUMA.0000426147.98903.ae Yoder-Wise, P. S. (2015). Leading and managing in nursing (6th ed). St. Louis, MO: Elsevier Mosby.