Carotid Pulse, Apex Impulse, Jugular Venous Pulse
advertisement

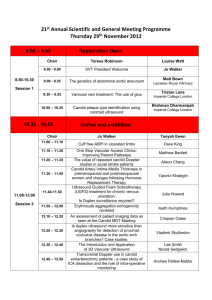
Diagnostic Utility of Examination of the Carotid Pulse Apex Impulse Jugular Venous Pulse Mary Beth Fontana M.D. Cardiovascular Medicine Block Learning Objectives Evaluate carotid pulse and auscultate for bruits Localize and characterize the apex impulse Identify jugular venous pulse components and assess jugular venous pressure Describe the abnormalities of the carotid pulse, apex impulse, and jugular venous pulse in cardiac and pericardial disease Resources Lilly doesn’t have specific sections on carotid pulse or apex impulse, instead describing them with some specific diagnoses. Jugular venous pulse; Chapter 2, pp.29-30 This module summarizes the abnormalities of all 3 that are pertinent to diagnosis Learning Objectives For the carotid pulse, apex impulse, jugular venous pulse be able to: Describe the normal characteristics Describe the method of examination Explain the pathophysiology causing abnormalities of the components of each The abnormalities described are mentioned in the clinical examination of the individual diagnoses Carotid Pulse Palpate between larynx and sternocleidomastoid muscle Marker of ventricular systole Rapid upstroke and slower decline Normal Carotid Pulse Rapid upstroke Dicrotic notch Abnormal Carotid Pulse Increased volume, rapid upstrokes Sympathetic stimulation increases stroke volume and upstroke velocity Bradycardia-larger stroke volume per beat Aortic valvular regurgitation Aging stiffens walls – flow is transmitted more rapidly which raises systolic blood pressure and maintains the rapid upstroke Pulsus Parvus Reduced stroke volume Left ventricular failure Severe fixed LV outflow obstruction Blood volume depletion Pulsus Tardus Slow upstrokes Obstruction to flow between heart and carotid Most common is valvular aortic stenosis Turbulent flow in carotid is audible—called a BRUIT and can cause a palpable vibration of the arterial wall – called a THRILL Pulsus Parvus &Tardus Valvular Aortic Stenosis carotid ECG Slow upstroke Small volume Bisferiens or Bifid Carotid Two systolic peaks Rapid ejection of a large stroke volume as in severe aortic valvular regurgitation. The elastic artery reverberates Initial rapid ejection followed by slow ejection in the same systole. Seen in dynamic muscular subvalvular aortic obstruction, called hypertrophic obstructive cardiomyopathy. Only the initial spike is palpable Bisferiens Carotid Pulse Aortic Regurgitation 2 systolic peaks Bisferiens Carotid Pulse Hypertrophic Obstructive Cardiomyopathy spike dome Dicrotic notch Pulsus Alternans Sign of severe left ventricular failure Aortic pressure Strong beat from larger LV diastolic volume Weak beat from smaller LV diastolic volume Paradoxical Pulse Sign of fluid under pressure in the pericardial space-- tamponade expiration Aortic pressure inspiration 15mmHg drop Greater than 10 mmHg fall in systolic pressure with inspiration LV Apex Impulse Recording of the apex impulse- usually only the E is palpable A wave may be palpable at time of S4 Systolic contraction of LV contacting the chest wall is palpable– the E point Rapid filling wave may be palpable at time of an S3 LV Apex Impulse Midclavicular line 5th intercostal space in the supine and upright position Palpable in 50% Quarter size or smaller Marker of ventricular systole Size of impulse, duration, and magnitude can be assessed in left lateral position Abnormal Apex Enlarged LV - displaced toward left axilla Prominent heave- ejection of large stroke volume Sustained- Poor LV systolic function, prolongation of ejection time from obstruction to LV outflow Double or triple apex impulses - palpable gallop(s) Normal JVP - RA a = atrial contraction C=upward thrust of T valve v = atrial filling with T valve closed during ventricular systole x =atrial relaxation, emptying y descent = atrial emptying in early diastole Carotid artery and internal jugular vein anatomy JVP Examination Elevate head 10-15 degrees to see waves and estimate pressure. If JVP visible at 45 degrees, RA pressure is abnormally high Measure vertical distance above manubrial-sternal junction and add 5 to get RA pressure. Time events by feeling carotid pulse on opposite side of neck; a is before carotid, v peak is after. The c is not seen Descents are more rapid than ascents of waves JVP normally goes down with inspiration Elevated Jugular Venous Pressure Increased blood volume- pregnancy, heart failure Obstruction to atrial emptying- pericardial disease, tricuspid valve obstruction, noncompliant RV Absent wave forms- SVC obstruction Further elevation with inspiration- Kussmaul’s signconstrictive pericarditis Abnormal A Wave, Attenuated Y Descent Large a wave due to stenosis of tricuspid valve Attenuated y descent Also seen when the RV muscle has reduced compliance Large V wave-tricuspid valve regurgitation No a wave – loss of atrial contraction, atrial fibrillation V Y The RA is filling from the vena cavae and from the RV during ventricular systole when the T valve should be closed. The Y descent is rapid from emptying a large volume into the RV AV Dissociation – Cannon A waves P waves and QRS’s occur independently due to complete block of conduction at the AV node A Atrial contraction when tricuspid valve is closed A P P RA – JVP Tamponade 20mm. Hg Good X descent Attenuated Y descent Fluid under pressure in the pericardial space prevents passive ventricular filling in early diastole JVP – RA Accentuated Y Descent Constrictive Pericarditis y Constriction raises RA pressure, early diastolic filling is rapid until constricting pericardium limits filling Summary & Advice Thank you for completing this module • • I hope that I was able to teach the subject clearly. If you have any questions, write to me: MaryBeth.Fontana@osumc.edu