Facial Pathologies and Related Special Tests
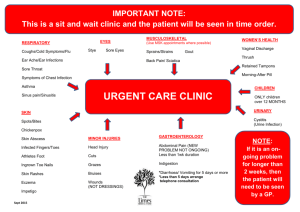
advertisement

Facial Pathologies and Related Special Tests Orthopedic Assessment III – Head, Spine, and Trunk with Lab PET 5609C Ear Pathologies Auricular Hematoma: “Cauliflower Ear” MOI: Repeated blunt trauma or shearing forces to external ear Pooling of blood between the skin and cartilage (cartilage deprived of nutrition) Over time, hematoma can scar deformity Inspection: Red appearance Swelling of auricle Ecchymosis Ear Pathologies Auricular Hematoma: Palpation: Functional/Neurological Tests: Acute Injury: pain, confirm presence of hematoma Chronic Injury: hardened feeling Otoscope → check inner ear Hearing and Balance Note: Rule out brain trauma (blow to head) Ear Pathologies Tympanic Membrane Rupture: History: Onset of Symptoms → Acute Pain → Severe pain in middle ear; radiating inward and outward MOI: Sudden change in air pressure → blunt trauma (slap to ear), blocked sneeze, mechanical intrusion (i.e. cleaning ear with pen) Tympanic membrane bursts Predisposing Conditions → URI, otitis media Ear Pathologies Tympanic Membrane Rupture: Inspection: Blood, fluid leaking from ear (fluid should not be present in canal → immediate referral) Inspection with Otoscope: Can signify skull fracture Cerumen – reddish-brown wax formed in auditory meatus Functional Testing: Hearing Loss Valsalva maneuver may result in audible escape of air from within inner ear Ear Pathologies Tympanic Membrane Rupture: Complications: Permanent hearing loss Ear infection (otitis media) Treatment: Ruptured or perforated eardrum usually heals by itself within 2 months Treatment: relieve pain, prevent infection (Antibiotics) Surgical repair of the ear drum may be needed Prevention: Keep ear dry and clean while it heals Prevent water entering the ear Ear plugs while swimming. Do not insert objects into the ear canal Ear Pathologies Otitis Externa: “Swimmer’s Ear” Infection of external auditory meatus History: Pain: constant, pressure, itching MOI: Inadequate drying of ear canal (water sports) Inspection: Excessive water exposure Water collects in the ear canal (trapped by wax) Resultant bacteria (streptococcus, staphylococcus) /fungus growth Predisposing Conditions: Psoriasis, eczema, oily skin, open wounds within ear; Overcleaning of external auditory canal Redness, possible presence of clear discharge from middle ear Palpation: ↑ pain with tugging on earlobe Treatment: Prescription drops (acid-based) mixed with antibiotics or corticosteroids Ear Pathologies Otitis Externa: Prevention: Decrease exposure to water Ear plugs (if prone to infection) Swimmer's ear drops or alcohol drops (SwimEAR®) used in the ear after water exposure followed by drying the ear with a hair dryer held at arms length Do not insert instruments, scratch, or use cotton swabs in the ears. Ear Pathologies Otitis Media: Infection or inflammation of the middle ear Often begins when infections (viral or bacterial) that causes URI spread to the middle ear History: Pain/pressure within ear Irritability, difficulty sleeping, fever Fluid draining from the ear Loss of balance Hearing difficulty Ear Pathologies Otitis Media: Inspection: Functional Testing: Otoscope → fluid build-up / reddened, bulging tympanic membrane Hearing Weber Test Treatment: Oral antibiotics Decongestants and antihistamine medications Nasal Pathologies Nasal Fractures: History: Onset: Acute (most commonly fractured facial/skull bone) Pain: Bridge of nose and cartilage, frontal and zygomatic bones MOI: Direct blows Inspection: Possible deformity Bleeding Ecchymosis (raccoon eyes) Nasal Pathologies Nasal Fractures: Palpation: Pain Crepitus Note: Any patient suffering a nasal fracture needs to be screened for injury to the eyes/head Nasal Pathologies Repeated Nasal Trauma: Saddle-Nose Deformity: Necrosis of nasal cartilage Collapsed bridge of nose Nasal Pathologies Repeated Nasal Trauma: Deviated Septum: Nasal Septum - thin wall inside your nose that separates right and left nasal cavities Ideally, septum is situated in the center of your nose 80 percent of people have a septum that is displaced to one side (one nasal passage smaller than the other) Septum significantly offcenter (deviated septum) Nasal Pathologies Deviated Septum: Blockage of one side of your nose – reduced air flow Signs and Symptoms: Causes: Difficulty breathing Nasal congestion Nosebleeds Frequent sinus infections Can be present at birth Result of injury Treatment: Medication, Surgery Throat Pathologies Throat Trauma: History: Inspection: Bruising, swelling Mouth/throat – possible bloody septum Patient: coughing (attempting to clear airway) / altered voice Palpation: Onset – acute Pain: Anterior neck, increased during swallowing or taking deep breaths MOI: Blow to anterior neck Point tenderness, crepitus, displacement of cartilage Treatment: Immediate referral / Monitor vital signs Facial Fractures Mandibular Fractures: History: Inspection: Onset: Acute Pain: Ramus or mental protuberance of mandible MOI: Direct blow Swelling, gross deformity Malocclusion of teeth Palpation: Tenderness, crepitus Facial Fractures Mandibular Fractures: Functional Tests: Neurological Tests: Cranial Nerves V, VII Special Tests: Pain with opening/closing mouth Lateral tracking of mandible Tongue Blade test Treatment: Referral Facial Fractures Zygoma Fractures: History: Inspection: Subconjunctival hematoma Periorbital swelling Palpation: MOI: Direct blow to cheek or inferior periorbital area Pain: Injury site, possibly ↑ with eye movement Tenderness at zygomatic arch, lateral eye socket Treatment: Referral Facial Fractures Maxillary Fractures: History: Inspection: Ecchymosis Swelling Palpation: May occur concurrently with nasal fracture Pain: Midpoint of face Pain and crepitus Treatment: Referral Facial Fractures LeFort Fractures: Midface fracture MOI: High-impact forces Inspection: Automobile accident Unusual in athletics Upper teeth/face can be displaced forward Classification: I – maxilla II – maxilla and nasal III – crosses zygomatic and orbital bones Dental Conditions Dental Injuries: Rates Female athletes: 1.5% - softball 7.5% - basketball Male athletes: Basketball (highest) Ice hockey Lacrosse Football Soccer Baseball Volleyball ADA: Universal National System (1-32) Dental Conditions Tooth Fracture: Classifications (Ellis System) Class I – enamel only Class II - enamel and dentin pain to touch and sensitivity to air. Class III – enamel, dentin, pulp Pain with manipulation, air, and temperature. Dental Conditions Tooth Luxation: Extrusive luxation: partially displaced from the socket Greatly increased mobility and radiographs show displacement Lateral luxation: tooth displaced laterally Intrusive luxation: teeth forced into their sockets in an axial direction Can be buried (no visibility) Decreased mobility Dental Conditions Intrusive Luxation Lateral and extrusive luxation Avulsion and luxation Dental Conditions Dental Caries: Cavities Cause: Plaque – food, mucus, and bacteria that collect and harden on the exposed tooth (can harden into tartar) Sugars, starches, acid-rich food, poor oral hygiene Signs/Symptoms: As decay enlarges → heat/cold sensitivity, visible defect Dental Conditions Gingivitis: Inflammation of the gums Cause: Accumulation of plaque → bacteria released into gums Overbrushing can lead to inflammation Increased risk: Signs/Symptoms: Poor oral hygiene Diabetes Pregnancy, Birth control pills Soreness, bleeding gums Red and swollen gums Treatment: Plaque, tartar removal (dental care) TMJ Pathology TMJ Dysfunction: History: Inspection: Onset: Acute, chronic Pain: Area of TMJ; clicking/locking of joint MOI: Blunt trauma to the mandible or progressive joint degeneration (i.e. punch – forces mandible laterally) Swelling, Malocclusion of the jaw Palpation: Point tenderness Clicking when mouth open/closed TMJ Pathology TMJ Dysfunction: Functional Tests: Observation of jaw during opening/closing of mouth Any deviation? Treatment: Referral to physician Instruct athlete not to eat hard foods (↑ pain) Dental Conditions Special Tests Otoscope: Allows health care providers to see the outer and middle ear Steps: Choose a speculum size appropriate for the patient’s canals Hold the otoscope in the hand of the same side as the ear you are examining Special Tests Otoscope Use: (Steps continued) Examine the good ear first: Prevents spread of infection into unaffected ear You can see normal anatomy (for comparison) Inspect the Eardrum: Tympanic membrane should appear shiny, translucent, and smooth (without perforations) Any suspected disruption, fluid, pus, debris seen → Medical referral Special Tests TMJ Palpation Test: (External) Procedure: TMJ is palpated while mouth is opened and closed Positive Sign: Asymmetry of movement Clicking / Locking of joint Special Tests TMJ Palpation Test: (Internal) Positioning: Examiner places his fingers in the outermost portion of auditory canal (with rubber gloves on) Procedure: Subject repeatedly opens/closes the mouth while examiner applies gentle pressure in an anterior direction Positive Findings: Pain, discomfort during opening/closing of mouth Asymmetry of movement Special Tests TMJ Range of Motion: Patient Position: Seated or standing (examiner is positioned in front of subject) Procedure: Patient attempts to place as many flexed knuckles as possible between upper and lower teeth Positive Test: Patient unable to place a minimum of 2 knuckles within the mouth Decreased TMJ ROM Special Tests Weber Test: Tests for hearing loss Otitis Media Procedure: Strike a tuning fork softly and place the vibrating fork on the middle of the patient’s forehead Ask patient if the sound is heard better in one ear or the same in both ears Special Tests Weber Test: (continued) Positive Test: Athlete hears the vibration louder in the affected ear Reasoning: Conduction problem in affected ear masks the ambient noise of the room, while the well-functioning inner ear picks the sound up via the bones of the skull causing it to be perceived as a quieter sound in the unaffected ear Special Tests Tongue Blade Test: Possible mandibular fracture Position: Patient seated with examiner standing in front Procedure: Tongue depressor is placed in patient’s mouth Patient attempts to hold the depressor in place, the examiner twists the tongue depressor Positive Test: Patient unable to maintain a firm bite / Pain Special Tests Chvostek Test: Facial Nerve Pathology Positioning: Patient seated or standing Procedure: Examiner taps over the masseter muscle and parotid gland Positive Finding: Twitching of the facial muscles (masseter) Special Consideration: Twitching of facial muscles may also be result of low calcium levels in the blood