The Organic Chemistry of Drug Design and Drug

The Organic Chemistry of
Drug Design and Drug
Action
Chapter 8
Drug Metabolism
Drug Metabolism
Foreign organism – elicits antibody response
Low molecular weight xenobiotics – nonspecific enzymes convert them into polar molecules for excretion
Enzymatic biotransformations of drugs – drug metabolism
Principal site of drug metabolism is the liver; also kidneys, lungs, GI tract take via mouth
Pathway of Oral Drugs absorbed through small intestine or stomach bloodstream liver
(first metabolized)
Drug metabolism by liver enzymes – first-pass effect
Avoid first-pass effect by changing the route of administration
• sublingual route (under the tongue) bypasses liver
- angina (sublingual)
• rectal route (suppository or enema)
- migraine headaches (rectal)
• intravenous (i.v.) injection – rapid response, circulation time of 15 seconds
Avoid first-pass effect by changing the route of administration (cont’d)
• intramuscular (i.m.) injection – for large volumes or slow absorption
• subcutaneous (s.c.) injection – through loose connective tissue of s.c. layer of skin
• pulmonary absorption – gaseous or highly volatile drugs
- asthma (aerosol)
• topical application
Prodrug approaches are discussed in Chapter 9
Drug metabolism is desirable once drug has reached site of action – may produce its effect longer than desired or become toxic.
Drug metabolism studies are essential for the safety of drugs. Metabolites must be isolated and shown to be nontoxic.
An active metabolite that is less toxic
• Terfenadine is cardiotoxic, since it binds to the hERG channel
• Fexofenadine has similar antihistamine activity, but no hERG activity
Synthesis of Radioactive Compounds
To increase sensitivity for detection of metabolites, radioactivity is incorporated into the drug candidate.
Incorporate a commercial radioactive compound near the end of the synthesis, if possible.
Usually the radioactive synthesis is different from that of the unlabeled compound.
[ 14 C] preferable to [ 3 H] – 3 H has shorter t
1/2 cleavage; loss of 3 H as 3 H
2
; isotope effect on C-H
O if C-H cleavage occurs
Only a trace amount of radioactivity is used (maybe 1 in 10 6 molecules); the remainder of the molecules is nonradiolabeled.
Metabolism of erythromycin
If the NMe
2 group is labeled with the [ 14 C]-CO
2 can be measured.
14 C,
If the drug is a natural product, a biosynthetic approach to radioactive incorporation is best
SCHEME 8.1
Biosynthesis of penicillins
If the drug is not a natural product, a chemical synthesis is needed.
[ 14 C] acetic anhydride could be used here
SCHEME 8.2
Chemical synthesis of linezolid
The radioactive drug is used in metabolism and bioavailability studies in rats, mice, or guinea pigs, then in dogs and/or monkeys.
If >95% of the radioactivity is found in urine and feces, and is nontoxic, it can be administered to humans.
Phase I clinical trials on healthy volunteers – radiolabeled drug administered to humans for human metabolism studies.
Advances that Made
Metabolism Studies Less
Difficult
More commercially-available radioactive compounds
High performance liquid chromatography (HPLC); new column packings; capillary GC; capillary electrophoresis
New mass spectrometric methods – tandem mass spectrometry/mass spectrometry; GC/mass spectrometry;
*HPLC/electrospray mass spectrometry
New nuclear magnetic resonance (NMR) techniques
*HPLC/NMR
*HPLC/NMR/MS
Principal Steps in Drug Metabolism
Studies
1.Isolation (often, this step can be omitted) – extractions, ion exchange
2.Separations – HPLC, GC
3.Identification – mass spectrometry (MS), NMR
4.Quantification – radioactive labeling, GC, HPLC
LC/MS/MS is a rapid method in which a sample is injected into the HPLC, then each peak is run into an electrospray ionization MS for parent ion data, then the parent ion is run into a second MS for fragmentation data.
Pathways for Drug Deactivation and
Elimination
• Rate and pathway of drug metabolism are affected by species, strain, sex, age, hormones, pregnancy, and liver diseases.
• Drug metabolism is stereoselective, if not stereospecific.
• Generally, enantiomers act as two different xenobiotics – different metabolites and pharmacokinetics.
• Sometimes the inactive enantiomer produces toxic metabolites or may inhibit metabolism of active isomer.
• Metabolism of enantiomers may depend on the route of administration.
• For example, the antiarrhythmia drug verapamil is 16 times more potent when administered i.v. than orally.
As the lipophilicity increases, metabolism increases; increased lipophilicity leads to better substrate activity with metabolizing enzymes.
FIGURE 8.1
Effects of lipophilicity on direct renal clearance and on metabolism
Verapamil is 16 times more active IV than orally
The more active (-) isomer is metabolized faster than the (+) isomer by the liver
(Advil)
Inactive ( R )-isomer is metabolized to active ( S )-isomer
No need to use a single enantiomer
One enantiomer can be metabolized to the other.
Drug metabolism reactions – two categories
Phase I transformations – introduce or unmask a functional group, e.g., by oxygenation or hydrolysis
Phase II transformations – generate highly polar derivatives (called conjugates) for excretion
Phase I Transformations
Oxidative Reactions
Late 1940s, early 1950s
Metabolism of 4-dimethylaminoazobenzene shown to require O
2 and a reducing system (NADPH).
Called a mixed function oxidase.
One atom of O from O
2 is incorporated into product; a heme protein is involved.
Cytochrome P450 – family of heme enzymes that catalyzes the same reaction on different substrates
(isozymes)
Drug-Drug Interactions
Changes in the pharmacokinetics and metabolism of drugs when multiple drugs are taken together.
One drug may inhibit a cytochrome P450, blocking metabolism of another drug.
One drug may induce a cytochrome P450, which increases metabolism of other drugs.
Hyperforin is found in St.
John’s Wort
Active constituent of St. John’s wort (hyperforin, 8.11
) activates the pregnane X receptor, which regulates P450 3A4 transcription, resulting in more active drug metabolism
Heme-dependent Mixed Function Oxidase
Scheme 4.35
Oxidizing agent
Reducing agent
Activated coenzyme
Reactions Catalyzed by Cytochrome P450
Site of Reactions Catalyzed by P450
Part of molecule undergoing reaction is determined by:
1. topography of the active site of the isozyme
2. degree of steric hindrance of the heme iron-oxo species to the site of reaction
3. ease of H atom abstraction or electron transfer from the compound
CYP450 activity is variable in the population
•
•
•
•
•
•
•
CYP450 is found in liver, kidney and lungs.
There are a number of different P450 families, which differ in their substrate and reaction specificity.
57 human genes for P450 have been indentified.
Individuals also vary in the properties of their P450s.
CYP450 2C9 and 2D6 are responsible for metabolism of about half of all drugs.
Variations in P450s are racially and ethnically distributed.
Pharmacogenomics—how the genetic characteristics of a person influences their response to drugs.
Individual variation in CYP450 2C9
•
•
•
CYP450 2C9 metabolizes phenytoin, S-warfarin, tolbutamide, losartan, and many nonsteroidal antiinflammatory agents
(NSAIDs).
At least 33 alleles of CYP450 2C9 have been discovered.
Most of the mutant alleles of CYP450 2C9 have low or no enzymatic activity.
CYP450 2C9 and tolbutamide metabolism
•
•
• Tolbutamide is a sulfonylurea antidiabetes drug.
CYP450 2D9 hydroxylates the aromatic methyl to give a much lower activity metabolite.
Individuals with mutant CYP450 2C9 alleles have higher concentrations of tolbutamide in the blood, longer duration of action, and lower blood glucose, so they are more likely to get hypoglycemia.
CYP450 2C9 and warfarin metabolism
•
•
•
•
Warfarin is an anticoagulant drug which inhibits vitamin K 2,3-epoxide reductase.
(S)-Warfarin is hydroxylated at C-6 and C-7 by
CYP450 2C9 to give inactive metabolites.
Mutant alleles of CYP450 2C9 have less activity for hydroxylation of warfarin, so patients with mutant alleles need to have lower doses.
The therapeutic index for warfarin is small even for wild-type patients.
Individual variation in CYP450 2D6
•
•
•
•
•
•
P450 2D6 metabolizes opiates, antiarrhytmics, tamoxifen and b
-blockers, among others.
More than 60 alleles of 2D6 have been discovered.
Some of the alleles of 2D6 have low or no enzymatic activity (PM).
Some of the alleles of 2D6 have intermediate activity
(IM).
Some of the alleles of 2D6 have somewhat higher activity (EM).
Some of the alleles of 2D6 have much higher activity than wild-type (UM).
CYP450 2D6 and opiate metabolism
•
•
•
•
Codeine is O-demethylated to morphine, the active metabolite in analgesia.
PMs can’t convert codeine to morphine, so don’t get analgesia.
UMs convert codeine to morphine very rapidly, so may experience toxicity .
Infants have been poisoned by breast milk from UM mothers taking codeine
.
CYP450 2D6 and tamoxifen metabolism
•
•
• Tamixofen is an antiestrogen used to treat breast cancer.
The metabolite, 4-hydroxytamoxifen, binds about 100-fold more strongly to estrogen receptors.
2D6 PMs respond poorly to tamoxifen treatment.
Reactions of Flavin
Monooxygenase
Table 8.2
Flavin monooxygenase is often more stereoselective than CyP450
CyP450 CyP450
FMO
Flavin Monooxygenase
(another mixed function oxidase)
Scheme 4.34
Nucleophiles with anionic groups are not substrates
X is N or S
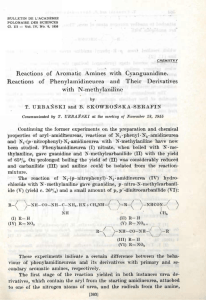
Aromatic Hydroxylation
Intermediate in aromatic hydroxylation
Jerina, Daly and Witkop
1968 National Institutes of Health (NIH) arene oxide isolated
SCHEME 8.3
Cytochrome P450 oxidation of naphthalene
Mechanism for Arene Oxide Formation and
Aromatic Hydroxylation
(favored over a)
SCHEME 8.4
Addition
–rearrangement mechanism for arene oxide formation
Reactions of
Arene Oxides
SCHEME 8.5
Possible fates of arene oxides toxic effects
Rearrangement of Arene Oxide to Arenol
Called the
NIH shift
SCHEME 8.6
Rearrangement of arene oxides to arenols (NIH shift)
Competing with the NIH Shift
deprotonation
The more stabilized the carbocation intermediate, the less favored for hydride shift - more deprotonation.
SCHEME 8.7
Competing pathway for NIH shift
Deuteration can reduce metabolism
Deuterated linezolid has t
1/2
6.3 h, compared to 4.5 h
=
NIH Shift with Groups Other than H
p -chloroamphetamine
Oxidation of a halogen-substituted aromatic ring is quite rare.
SCHEME 8.8
NIH shift of chloride ion
A common approach to slow down or block aromatic hydroxylation is to substitute the phenyl ring with a para -fluorine or para -chlorine
(deactivates the ring).
The half-life for the anti-inflammatory drug diclofenac ( 8.22
) is 1 h; for fenclofenac ( 8.23
) is
>20 h.
NIH Shift of a Nitro Group
Scheme 8.9
antiprotozoal
This reaction is electrophilic aromatic substitution
Favors electron-donating substituents
No aromatic hydroxylation if strongly electron-withdrawing substituents e withdrawing uricosuric agent
For drugs with 2 aromatic rings, the more e -rich one usually is hydroxylated.
hydroxylation here e withdrawing
- antipsychotic
Species Specificity
Major hydroxylation metabolites in dogs pro-R
Maybe a different isozyme pro-S in humans
- antiepilepsy
Mechanism of Epoxide Hydrolase
Hydration of Arene Oxide trans -diol anti attack
SCHEME 8.10
Metabolic formation and oxidation of catechols
Glutathione S-transferase Reaction with Arene Oxide
SCHEME 8.11
Formation of glutathione adducts from naphthalene oxides
Toxicity from Arene Oxides
SCHEME 8.12
Deoxyribonucleic acid adduct with benzo[a]pyrene metabolite benzo[a]pyrene alkylation of
DNA and RNA
Relationship between soot and cancer noted in 1775 chimney sweeps frequently developed skin cancer
Alkene Epoxidation
Also an anticonvulsant anticonvulsant
SCHEME 8.13
Metabolism of carbamazepine
Toxic Product of Alkene Oxygenation aflatoxin B
1
DNA adduct
SCHEME 8.14
Metabolic reactions of aflatoxin B
1
Oxidation of Carbons Adjacent to sp 2
Centers
Oxygenation next to aromatic sp 2 carbon antidepressant
Hydroxylation stereochemistry at C -1 depends on stereochemistry at C -2 in metoprolol.
antihypertensive
Stereochemistry at C -2 will affect how the molecule binds in P450, which determines which H is closest to the heme iron-oxo species.
Allylic Hydroxylation antiarrhythmic
Oxidation gives 7.38
(R = OH)
Allylic hydroxylation of THC
Oxidation Next to a Carbonyl Group
Enantiomer difference in metabolism hydroxylation here for (+)-isomer hydroxylation here for (-)-isomer sedative/hypnotic
Oxidation at Aliphatic and Alicyclic
Carbons
Both positions are hydroxylated anticonvulsant
Perhexiline is hydroxylated
Hydroxylation beta to a Carbonyl Group
SCHEME 8.15
C -demethylation of a flutamide metabolite
Oxidations of Carbon-Nitrogen Systems
Oxidative Deamination
Cleavage of NH
3 from 1° amines
SCHEME 8.16
Oxidative deamination of primary amines
Oxidative Deamination of amphetamine
N-Oxidation-Hydroxylation of Nitrogen
SCHEME 8.17
N -Oxidation pathways of amphetamine
Basic amines (p K a
8-11) are oxidized by flavoenzymes. Nonbasic compounds, such as amides, are oxidized by P450. Compounds of intermediate basicity, such as aromatic amides, are oxidized by both.
Alternative Pathway to Ketone
SCHEME 8.18
Amphetamine imine formation via the carbinolamine
Metabolism of 2° Amines and Amides
Oxidative N-Dealkylation
SCHEME 8.19
Oxidative N -dealkylation of secondary amines
Oxidation here a b
Oxidation here
SCHEME 8.20
Oxidative metabolism of propranolol
N-Oxidation of 2
Amines
anorectic
SCHEME 8.21
N -Oxidation of fenfluramine
Further oxidation occurs
Oxidation of 3° Amines and Amides
No oxidative deamination
Oxidative N-Dealkylation
Rate of oxidative N -dealkylation of 3 amines > oxidative N -dealkylation of 2 amines > oxidative deamination of 1 amines antihypertensive drug antidepressant drug
Rate of metabolism
R = NMe
2
> NHMe > NH
2
Enantioselective Oxidative N-Dealkylation
N -Demethylation of (+)-isomer is slower than that of (-)-isomer narcotic analgesic
SCHEME 8.22
Metabolism of selegiline (deprenyl)
( S )-(+)-deprenyl ( S )-(+)-methamphetamine ( S )-(+)-amphetamine weak MAO B inhibitor undesirable CNS stimulant
( R )-(-)-deprenyl ( R )-(-)-methamphetamine ( R )-(-)-amphetamine potent MAO B inhibitor weak CNS stimulant
Therefore only the ( R )-(-)-isomer is used
Rasagiline avoids the stimulation problem with Seligiline
Alicyclic 3°
Amine Oxidation
SCHEME 8.23
Oxidative metabolism of nicotine leading to C –N bond cleavage
.
Evidence for Iminium Ion Intermediates local anesthetic
SCHEME 8.24
Metabolism of lidocaine isolated
N-Oxidation of 3° Amines
N -Oxidation antihypertensive
Cyproheptadine forms the Noxide in dogs
N
-Oxidation of 3° Aromatic Amines
Two enzymes systems: P450 and flavin monooxygenase
P450 catalyzed N -oxidation
SCHEME 8.25
Mechanism of cytochrome P450-catalyzed N -oxidation of tertiary aromatic amines
N -Oxidation by P450 occurs only if there are no -hydrogens available or if the iminium radical is stabilized by electron donation.
Flavin Monooxygenase-Catalyzed
N-Oxidation of Aromatic Amines
SCHEME 8.26
Possible mechanism for N -oxidation of primary arylamines
Primary aromatic amines are generally not substrates for flavin monooxygenase; 2 and 3 aromatic amines are good substrates.
Two Pathways for N-Demethylation of
3 Aromatic Amines
SCHEME 8.27
Two pathways to N -demethylation of tertiary aromatic amines
Evidence to Support Carbinolamine
Formation
R = OH isolated
Mechanism of Carbinolamine
Formation
Based on low intrinsic isotope effects by P450, direct
H abstraction mechanism was excluded.
SCHEME 8.28
Mechanism of carbinolamine formation during oxidation of tertiary aromatic amines
N-Oxidation of Aromatic Amines (1 and 2 )
Generation of reactive electrophiles acetylation or sulfation
SCHEME 8.29
Metabolic activation of primary and secondary aromatic amines
Cytotoxicity of N-Hydroxylated Amides
Mechanism-based inactivator if 8.78
does not escape the enzyme prior to nucleophilic attack
SCHEME 8.30
Arylhydroxamic acid
N,O -acyltransferase-catalyzed activation of N -hydroxy-2-acetylaminoarenes
Amide N-Demethylation sedative
N-Oxidation of 1 and 2 Aromatic Amides
Generation of electrophiles
2-acetylaminofluorene
(R = H) carcinogenic agent
Toxicity of Acetaminophen
Two possible mechanisms for generation of reactive electrophile 8.80
SCHEME 8.31
Initial proposals for bioactivation of acetaminophen
Another possible mechanism for
Acetaminophen Hepatotoxicity
SCHEME 8.32
Bioactivation of acetaminophen via a radical intermediate
Ethanol induces a P450 isozyme that generates the radical; alcoholics have a higher incidence of acetaminophen hepatotoxicity.
Acetaminophen also causes renal damage, but little P450 is in the kidneys.
Prostaglandin H synthase is in high concentrations in kidneys.
Prostaglandin H synthase contains heme just like
P450 and catalyzes similar reactions
SCHEME 8.33
Proposed bioactivation of acetaminophen by prostaglandin H synthase
Oxidations of Carbon-Oxygen Systems
Oxidative O-Dealkylation
Same mechanism as oxidative N -dealkylation
O -Demethylation is rapid; as increase alkyl chain length, O -dealkylation gets faster up to propoxyl, then rate decreases.
Cyclopropyl gives ethers with longer plasma half lives.
Indomethacin is demethylated
Oxidative O-Dealkylation of codeine analgesic
O -Demethylation by Cyp450 2D6 is rapid
Regioselective O-Demethylation
In dogs O -demethylation only here blood pressure maintenance
Oxidation on the Carbon Next to a
Lactone Oxygen
SCHEME 8.34
Metabolic hydroxylation of rofecoxib
Oxidations of Carbon-Sulfur Systems
Three principal biotransformations: Oxidative
S -dealkylation, desulfuration, and S -oxidation
Oxidative S -dealkylation
Dealkylation occurs here sedative
Desulfuration (C=S C=O) anesthetic sedative
S-Oxidation
SCHEME 8.35
Cytochrome P450-catalyzed oxidation of sulfides
Occurs with P450 and flavin monooxygenase
Flavin monooxygenase gives sulfoxides only
P450 gives both S -dealkylation and sulfoxides
antihelmintic agent
Gives both S -dealkylation and S -oxidation metabolites
Thioridazine is oxidized on both sulfurs
Thiophenes are converted to thiophene S -oxides, which are electrophilic and can bind to liver proteins.
added in vitro to mimic a liver protein cysteine residue
SCHEME 8.36
S -Oxidation of tienilic acid
Oxidation of Sulfoxide to Sulfone
Oxisuran, an immunosupressive drug, is oxidized to the sulfone
Other Oxidative Reactions
Oxidative Dehalogenation volatile anesthetic
SCHEME 8.37
Oxidative dehalogenation of halothane
Oxidative Aromatization
Oxidation products of morphine
Oxidation of Alcohols to Aldehydes and
Aldehydes to Carboxylic Acids
Scheme 8.38
al coh ol d ehydr ogen ase
RCH
2
OH + NAD + RCHO + NADH + H + al dehyde dehydr oge nas e RCHO + NAD + + H
2
O RCOOH + NADH + H +
Oxidation of an aldehyde to a carboxylic acid is generally faster than reduction of an aldehyde to an alcohol.
Cytochrome P450 also oxidizes alcohols to aldehydes and aldehydes to carboxylic acids.
Oxidation of an Alcohol to a Carboxylic
Acid by NAD + Enzymes anti-AIDS drug
Oxidation of an Alcohol to a Carboxylic
Acid by a P450 Isozyme antihypertensive drug
The metabolite is 10 times more potent an antagonist of the angiotensin II receptor than losartan.
Reductive Reactions
Carbonyl Reduction
Typically aldo-keto reductases that require NADPH or NADH
Reduced here
Hydroxylated here
(R)-isomer:
(R,S) alcohol
(S)-isomer:
R=OH +
4:1 (S,S) : (S,R) alcohols
When the racemic mixture was administered, the R -isomer gave aromatic hydroxylation (both 6and 7-hydroxyl) as the major metabolites. Administration of racemates can affect the metabolism of each enantiomer.
Species Variation in Stereochemistry opioid antagonist used for addiction rehabilitation
6 -alcohol ( 7.102
, R 1 = OH, R 2 =
H) in chickens
6 b -alcohol ( 7.102
, R 1 = H, R 2 =
OH) in rabbits and humans
, b -Unsaturated Ketone Double Bonds
Reduced
7.94
, R 3 = Et) and norethindrone ( 7.94
, R 3 = Me) is reduced; norgestrel gives 3 -alcohol (R 1 = H, R 2 = OH) but norethindrone gives 3 b -alcohol (R 1 = OH,
R 2 = H).
Double bond reduced
Nitro Reduction
SCHEME 8.39
Nitro group reduction
Nitro Reduction
Often the amine metabolite is not observed because it is easily air oxidized back to the nitro compound, for example, the anti-parasitic agent niridazole is reduced to the hydroxylamine, but is reoxidized to niridazole, and clonazepam is reduced to the unstable amine.
Nitro reduction with ring opening
SCHEME 8.40
Reductive metabolism of nitrofurazone
Azo Reduction
SCHEME 8.41
Azo group reduction
Azo Reduction
SCHEME 8.42
Reductive metabolism of sulfasalazine
Reduction carried out by intestinal bacteria.
Reduction of Azido to Amino
Anti-AIDS
3
Amine Oxide Reduction
imipramine N -oxide
Reduced in the presence of O
2 to the amine
Reductive Dehalogenation
SCHEME 8.43
Reductive dehalogenation of halothane
Cytochrome P450 in the absence of O
2
May be the cause for
Halothane hepatitis
Carboxylation Reactions
Metabolized to 8.124
, R = COOH
Hydrolytic Reactions
(nonspecific esterases and amidases in plasma, liver, kidney, and intestines)
Electron-withdrawing groups accelerate hydrolysis.
Conjugation with carbonyls decelerates hydrolysis.
Steric hindrance decelerates hydrolysis.
Hydrolyzed by all human tissues
Selectivity for Aliphatic vs.
Aromatic Esters
Some esterases catalyze the hydrolysis of aliphatic esters and others aromatic esters.
In vivo hydrolysis
Hydrolysis by liver enzymes in vitro
Amide vs. Ester Hydrolysis
Generally amides are more slowly hydrolyzed than esters.
Hydrolysis of procaine >> procainamide
Amide vs. Ester Hydrolysis
No amide hydrolysis
Ester hydrolysis only
Some amides are hydrolyzed at rates comparable to that of esters (maybe because of electronwithdrawing groups).
Hydrolysis of phenacetin produces a toxic amine
Amide Hydrolysis - Enantiomer Toxicity
(
Both enantiomers are anesthetics
NH
2
R )-isomer
CH
3 causes methemoglobinemia
( S )-isomer not hydrolyzed
Stereospecific metabolism of phensuximide, an anticonvulsant
Enantiomer-Selective Hydrolysis
The ( R )-(-)-ester is hydrolyzed in the liver, but the ( S )-(+)-ester is hydrolyzed in the brain.
Differential Enantiomeric Metabolism
(S)-enantiomer
(R)-enantiomer
SCHEME 8.44
Competitive metabolism of R - and S -etomidate
Phase II Transformations
Conjugation Reactions
Attachment of small polar endogenous molecules to drugs or (more often) to metabolites of phase I enzymes
Further deactivates drugs and produces watersoluble metabolites readily excreted
Conjugation reactions take place with hydroxyl, carboxyl, amino, heterocyclic N , and thiol groups; if not present, a phase I reaction introduces it
Many drugs are excreted without any modification at all.
Mammalian Phase II
Transformations
Table 8.7
Glucuronidation
Biosynthesis and Reactions of UDP-glucuronic Acid
SCHEME 8.45
Biosynthesis and reactions of UDP glucuronic acid
Classes of Compounds Forming Glucuronides
Diseases (inborn errors of metabolism) associated with defective glucuronidation
Crigler-Najjar syndrome and Gilbert’s disease
• deficiency of UDP-glucuronosyltransferase
• adverse effects caused by accumulation of drugs
• inability of neonates to conjugate the antibacterial chloramphenicol ( 8.142
) - “gray baby syndrome”)
Species Specificity, Regioselectivity, and Stereoselectivity
Antibacterial drug sulfadimethoxine is glucuronidated in humans (at arrow) but not in rats, guinea pigs, or rabbits.
OMe
N
H
2
N SO
2
NH N
OMe
Sulfadimethoxine
Two different glucuronides are formed here here
The R,R -(-)-isomer is conjugated with higher affinity, but lower velocity than is the S,S -(+)isomer.
The two hydroxylated isomers of nortriptyline metabolite
8.144
(R = OH) are glucuronidated stereospecifically. Liver and kidney glucuronosyltransferases convert only the E -(+)isomer and the intestinal enzyme converts only the ( E )-(-)isomer.
Human UGTs
•
• 40-70% of drugs are glucuronidated in humans.
Twenty-two UGTs have been identified.
Polymorphisms of UGT1A1
Polymorphisms of UGT1A3
UGT alleles can lead to severe side effects
Sulfate Conjugation
Occurs less often than glucuronidation (limited availability of SO
4
= ). Main substrates are phenols, but also aliphatic
OH, amines, and thiols (much less).
Glucuronidation and sulfation can occur on the same substrates, but the K m for sulfation is usually lower, so it predominates.
sulfation here
(phenolic OH instead of aliphatic OH) bronchodilator
Hepatotoxicity and Carcinogenicity by Sulfation
SCHEME 8.47
Bioactivation of phenacetin
Amino Acid Conjugation
SCHEME 8.48
Amino acid conjugation
Glycine conjugates are most common in animals.
L -Glutamine conjugates are most common in primates
(insignificant in nonprimates).
Metabolism of Brompheniramine
(antihistamine)
SCHEME 8.49
Metabolism of brompheniramine
Metabolism of diphenhydramine (Benadryl)
The pathway is the same as bromopheniramine, except that it is conjugated with glutamine
Glutathione Conjugation
Glutathione
GSH
Found in all mammalian tissues (5-10 mM in liver and kidneys)
Scavenger of harmful electrophiles
Glutathione
Conjugation
SCHEME 8.50
Examples of glutathione conjugation
Further Metabolism of GSH Conjugates
Metabolism of glutathione conjugates to N -acetyl-
L -cysteine conjugates
Referred to as phase III metabolism
SCHEME 8.51
Metabolism of glutathione conjugates to mercapturic acid conjugates
Water Conjugation
Epoxide hydrolase reactions; such as hydrolysis of arene oxides, as discussed earlier.
Acetyl Conjugation
Important for xenobiotics with primary NH
2
+
Converts ionized amine (RNH
3
) to uncharged amide
O
(RNHCCH
3
)
Metabolites are less water soluble; possibly serves the function of deactivating the drug.
Occurs widely in animals
Extent of N -acetylation in humans is a genetically determined characteristic - called acetylation polymorphism.
• Egyptians are slow acetylators - toxic buildup of drugs but longer drug effectiveness.
• East Asians and Canadian Eskimos are fast acetylators inadequate response.
Acetylation of Amines
SCHEME 8.52
N -Acetylation of amines
Makes less polar:
RNH
3
+
Examples of Drugs Exhibiting
Acetylation Polymorphism
Antibacterial
Treatment of leprosy
Antituberculosis
Cilastatin is acetylated. It is administered with Imipenem
Fatty Acid and Cholesterol Conjugation
Fatty acid metabolites of 8.177 and 8.178
deposit in liver, spleen, adipose tissue, and bone marrow.
Cholesterol esters can be formed
Development of the hypolipidemic drug 8.180
had to be stopped because cholesterol esters deposited in the liver.
Methylation - relatively minor in drug metabolism
Generally occurs when the compound has a structural similarity to normal endogenous substrates of the methyltransferase.
SCHEME 8.53
Methylation of xenobiotics
Methylated here regiospecifically bronchodilator
Methylation by catechol O methyltransferase requires a catechol (an aromatic 1,2dihydroxy) substrate. An aromatic
1,3-dihydroxy compound ( 8.185
) does not get methylated.
Phenolic hydroxyls also can get methylated
Methylation here
(minor)
N -Methylation also occurs to a minor extent.
Oxyprenolol is N -dealkylated to 8.187
, R = H, which is methylated to 8.187
, R = CH
3
.
antihypertensive
S -Methylation
Captopril and propylthiouracil are S -methylated.
Reactive metabolites
Atorvastatin and lumiracoxib can form an electrophilic quinone imine.
Hard and Soft Drugs
Sometimes a drug is not metabolized rapidly enough
(long plasma half life). The plasma half life for an analog ( 8.196
) of the antiarthritis drug celecoxib ( 8.195
) in dogs is about a month! To shorten the plasma half life the para -chloro was changed to para -methyl because a carbon next to an aromatic group is known to undergo
P450 oxygenation.
plasma t
1/2
9 h plasma t
1/2
680 h
Compounds (like 8.196
) that are difficult to metabolize are termed hard drugs. Those that are easily metabolized (like 8.195
) are soft drugs
(also called antedrugs).
Soft drugs are designed to have a predictable and controllable metabolism to nontoxic and inactive products after they have achieved their pharmacological effect.
8.197 is a soft analogue of
8.198, an antifungal
Retro Approach Related to Soft Drugs
Identify a biologically inactive metabolite, then modify to an active drug in such a way that this modification is known to be reversed to the inactive metabolite.
The anti-inflammatory agent loteprednol etabonate ( 8.199
) was designed based on the known inactive steroid 8.201
[an analog of the antiinflammatory drug prednisolone ( 8.200
)].
Compound 8.199
is metabolized by esterases to
8.201
after it elicits its antiinflammatory effect.