Pediatric Anesthesia and the URI
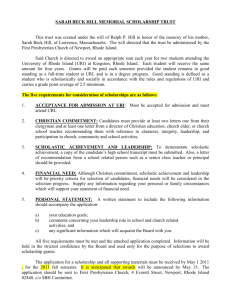
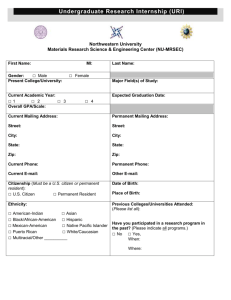
advertisement

Pediatric Anesthesia and the Child with URI Words of Wisdom Greg & Joy Loy Gordon MD et al Nov 2006 The Old School: Elective surgery + URI = Cancel (Postpone) case Newer school? URI increases risk but Complications can be anticipated recognized treated So perhaps we ought to proceed Anesth Analg 2005;100:59-65 Problems interpreting data • What exactly is a URI? • Type/duration of surgery • Airway instrumentation • Anesthetic agent/technic Evidence from observational studies Not random double-blinded controlled Alan R. Tait, PhD Director of Clinical Research Professor of Anesthesiology University of Michigan Ann Arbor, MI atait@umich.edu Shobha Malviya, MD Director, Pediatric Research Associate Professor of Anesthesiology smalviya@umich.edu Frederic A. Berry, MD Professor of Anesthesiology and Pediatrics University of Virginia fab@virginia.edu Charles J. Cote, MD Vice Chairman Director of Research Department of Pediatric Anesthesiology Children's Memorial Hospital Chicago, IL ccote@anesthesiaweb.com Anesthesia for the Child with an Upper Respiratory Tract Infection: Still a Dilemma? Alan R. Tait, PhD, and Shobha Malviya, MD Anesth Analg 2005;100:59-65 Reported events – what will happen to the kid with URI? DeSoto et al. Anesthesiology 1988;68:276 Bronchospasm Faster drop in SpO2 Postop lower SpO2 Laryngospasm Tait et al. Anesthesiology 1987;67:930 Breath-holding SpO2 < 90 % Severe coughing Specific predictors – which kids will it happen to? Parnis et al. Paediatr Anaesth 2001;11:29 ETT > LMA > FM Parents say child had “cold” Snoring history Passive smoking Thiopental > halothane > sevo > propofol Sputum Nasal congestion Muscle relaxant not reversed Specific predictors – which kids will have more problems? Tait et al. Anesthesiology 1987;67:930 Independent risk factors: ETT in child < 5 yrs old Premie (< 37 wks EGA) Reactive airway disease Parental smoking Surgery involving airway Copious secretions Nasal congestion Let’s do some math 9 URIs per year (day care) Conservatively wait 6 wks for airway hyperreactivity 9 x 6 = 54 wks to postpone surgery How many weeks in a year ? Severe symptoms postpone 4 weeks Mucopurulent secretions Productive cough Fever Lethargy Signs of pulmonary involvement A one to two week delay may be all that is needed for children with uncomplicated nasopharyngitis. Berry FA. Semin Anesth 1984;3:24 “children with a mild URI may be safely anesthetized, since the problems encountered are generally easily treated and without long-term sequelae.” J Clin Anesth 1992;4:200 “children with a recent URI fared as well a those with an acute URI. Delaying a procedure will not significantly change the incidence of adverse respiratory events. Little is gained except to create inconvenience for the family, the surgeon, and the surgery schedule.” Anesthesiology 2001;95:383 “Nearly 2,000 procedures would have to be canceled to prevent 15 cases of laryngospasm.” Anesthesiology 2001;95:383 “Despite the increased risk of respiratory events in children with URIs, there appears to be very little residual morbidity.” No cases in ‘closed claim literature’ implicating URI Only 3 of 742 current or recent URIs: 2 admitted for pneumonia after surgery 1 admitted for stridor (uneventful recoveries) What about child with “intermediate” symptoms? Tait-Malviya URI Algorithm No severe symptoms or Recent URI General anesthesia needed Estimating risk/benefit ratio Risk factors Hx of asthma Use of an ETT Copious secretions Nasal congestion Parental smoking Surgery of airway Hx of prematurity Other factors? Need for experience Parents traveled far Surgery canceled before Comfort caring for child with URI Tait-Malviya URI Algorithm Anesthetic management of URI child Avoid ETT Consider LMA Pulse oximetry Hydration Humidification? Anticholinergics? Dilemma remains for child with intermediate symptoms Recommend: Decide on case-by-case basis Considering: Identified risk factors Need for expedient surgery Your experience and Your comfort level Using: “Tincture of common sense” Good judgment Anesthesia for the Child with an Upper Respiratory Tract Infection: Still a Dilemma? Alan R. Tait, PhD, and Shobha Malviya, MD Anesth Analg 2005;100:59-65