Neonatal Emergencies - Greg Gordon's Place
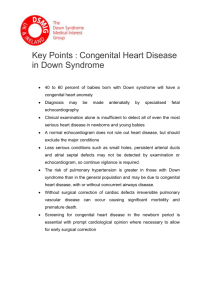
advertisement

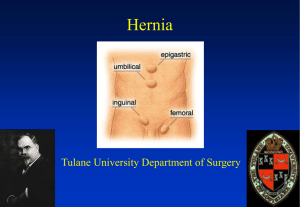
Neonatal Emergencies Joy Loy MD March 2009 Objectives Participants will be able to 1. discuss the underlying pathophysiology of selected neonatal emergencies, 2. explain the anesthetic implications and 3. describe safe anesthetic plans for each. Preoperative Evaluation • Maternal and perinatal history • Recreational drug use • Birth history • Minimum labs: glucose and CBC • Look for associated anomalies • Cardiac and respiratory status • Metabolic and electrolyte imbalance • Hydration status • Coagulation profile • IV access Pyloric Stenosis Pyloric Stenosis Most common GI obstructive anomaly in neonates Hypertrophy of the muscular layer of the pylorus A medical emergency but not a true surgical emergency Incidence: 1 – 3 :1,000 live births 2 - 5x more common in first born, M > F (4:1) Pyloric Stenosis Etiology : unknown ? acquired condition with hereditary predisposition Symptoms are apparent between 2nd-6th wk of life Presents with nonbilious projectile vomiting, signs of dehydration, jaundice (2%) Pyloric Stenosis Physical Exam visible gastric peristalsis palpable “olive-shaped” mass to the right of the epigastric area signs of dehydration Labs: CBC ABG serum electrolytes BUN EKG Pyloric Stenosis Diagnosis history and physical exam abdominal ultrasound upper GI series with barium contrast not recommended pathological pyloric wall thickness ≥ 4 mm pyloric length of > 16 cm Pyloric Stenosis Metabolic Abnormalities • hyponatremia • hypochloremia • hypokalemia • 1° metabolic alkalosis • compensatory respiratory acidosis • paradoxical acidic urine Pyloric Stenosis Preoperative Preparation supportive treatment surgical management check lab indices for safe anesthesia Pyloric Stenosis Preoperative Preparation Supportive therapy • Correction of fluid deficits maintenance: D5 0.2% NaCl + KCl 20 - 40 mEq/L replacement: LR, albumin, normal saline • Correction of electrolyte imbalance • Prevention of aspiration : NGT Pyloric Stenosis Surgical Management Pyloromyotomy definitive treatment open or laparoscopic Lab indices for safe anesthesia serum Cl >100 mEq/L HCO3 < 28 mEq/L Pyloric Stenosis Anesthetic Concerns • pulmonary aspiration • severe dehydration • metabolic alkalosis Pyloric Stenosis Intraoperative Management Monitors : ASA standard Decompress the stomach GA: Induction: controversial awake intubation rapid sequence IV induction and intubation with cricoid pressure inhalation induction with cricoid pressure ± muscle relaxant Pyloric Stenosis Intraoperative Management Cook-Sather, 1998 (CHOP) • prospective, nonrandomized study • awake vs paralyzed intubation (RSI and MRSI) • faster and more successful tracheal intubation with muscle paralysis • awake intubation does not protect from bradycardia and desaturation Pyloric Stenosis Intraoperative Management Maintenance IV narcotics: rarely needed inhalational agents Postop pain relief acetaminophen 30-40 mg/kg PR caudal epidural LA infiltration of surgical incision Pyloric Stenosis Extubate awake Postoperative concerns respiratory depression and apnea hypoglycemia Congenital Diaphragmatic Hernia a problem unresolved Congenital Diaphragmatic Hernia Herniation of abdominal viscera into the thorax Result from failure of the pleuroperitoneal canal to close at ~ 8th wk of gestation or early return of midgut to the peritoneal cavity Most challenging and frustrating of all neonatal surgical emergencies Congenital Diaphragmatic Hernia 50% mortality regardless of the method of treatment Incidence: 1:2,000-5,000 live births M<F 1:1.8, frequently full term Etiology: unknown no genetic factors have been implicated Antenatal history: polyhydramnios Congenital Diaphragmatic Hernia Classification • Absent diaphragm : rare • Diaphragmatic hernia 80% posterolateral L >R (Bochdalek) 2% anterior (Morgagni) 15 - 20% paraesophageal • Eventration (15 - 20%) Congenital Diaphragmatic Hernia Associated anomalies (20-50%) cardiovascular 13 - 23% CNS 28% gastrointestinal 20% genitourinary 15% • increase the mortality rate Congenital Diaphragmatic Hernia Classic Triad Dyspnea Cyanosis Apparent dextrocardia Congenital Diaphragmatic Hernia Physical Exam scaphoid abdomen and barrel chest bowel sounds in the chest displaced heart sounds Laboratory Studies CBC ABG electrolytes calcium glucose Congenital Diaphragmatic Hernia Diagnosis: chest x-ray • loops of bowel in the chest • mediastinal shift • absent lung markings Congenital Diaphragmatic Hernia IMMEDIATE Intubation + Stomach Decompression Congenital Diaphragmatic Hernia Determinants of Survival • degree of pulmonary hypoplasia ipsilateral lung > contralateral lung • development pulmonary vasculature Congenital Diaphragmatic Hernia Goals of Management • maximize arterial oxygenation mechanical ventilation: use low inflating pressures increases pulmonary blood flow • prevention of pain fentanyl infusion 3-10 mcg/kg/hr • correction of acidosis Congenital Diaphragmatic Hernia Standard Management Strategy Reduce pulmonary HTN Moderate alkalosis pCO2 < 40 mmHg PaO2 >100 mmHg Congenital Diaphragmatic Hernia Recent Strategy • Permissive hypercapnia and hypoxemia • Pressure-limited ventilation (<25 cmH2O) • Postductal pCO2 40-65 mmHg • Preductal SpO2 85-90% • Postductal SpO2 ignored unless pH is < 7.20 or pCO2 > 65 Congenital Diaphragmatic Hernia Bohn (1986) reevaluation of the traditional “mad dash” surgical strategy recommended 24 – 48 hrs medical stabilization assessment of efficacy of delayed approach infants unresponsive to initial therapy will fail to survive with surgery or any other treatment including ECMO Congenital Diaphragmatic Hernia The Relationship Between PaCO2 and Ventilation Parameters in Predicting Survival in CHD • Arterial CO2 accurately reflects the degree of lung development • Poor survival in the presence of severe pulmonary hypoplasia • CO2 retention and severe preductal shunting have 90% mortality Bohn, DJ, et al J of Pedia Surg 19: 666-671, 1884 Congenital Diaphragmatic Hernia nomogram: to predict the degree of pulmonary hypoplasia in the infants and chance of survival used the preop PaCO2 and an index of ventilation (Vi) If PaCO2 < 40 and Vi < 1000: survival almost universal If PaCO2 > 40 and Vi > 1000: death virtually inevitable ٭Vi = mean airway pressure x respiratory rate Congenital Diaphragmatic Hernia Relationship of Alveolar-arterial Oxygen Tension Difference in Diaphragmatic Hernia in the Newborn A-aDO2 on 100% O2 < 400 mmHg: usually survive 400 - 500 mmHg: intermediate chance > 500 mmHg: unlikely to survive Harrington J, et al Anesthesiology 56: 473-476, 1982 Congenital Diaphragmatic Hernia Acid Base Balance and Blood Gases in Prognosis and Therapy of CHD High Mortality pH < 7.0 pCO2 >60 mmHg pO2 < 50 mmHg Boix-Ochoa J, et al J Pediatric Surg 9:49-57, 1974 Congenital Diaphragmatic Hernia Indications of Surgical Repair • Reversal of ductal shunting • O2 index of < 40 • Arterial pCO2 maintainable under 40 mmHg • Hemodynamic stability Congenital Diaphragmatic Hernia Preoperative Preparation • Look for associated anomalies • Labs: CBC, electrolytes, ABG, glucose, blood type and crossmatch • Ancillary procedures: CXR, Echo • Venous access: upper extremities preferred • Prevention of hypothermia Congenital Diaphragmatic Hernia Intraoperative Management Monitors: ASA standard invasive : arterial line ± CVP foley catheter * 2 pulse oximeters: preductal and postductal * precordial stethoscope on the right axilla NGT to decompress the stomach Adequate IV access Congenital Diaphragmatic Hernia Intraoperative Management Induction awake intubation rapid sequence IV induction and intubation with assisted or controlled ventilation * avoid mask ventilation or PPV before intubation Supine position, left subcostal incision Congenital Diaphragmatic Hernia Intraoperative Maintenance of anesthesia volatile agents + IV narcotics + muscle relaxants TIVA avoid nitrous oxide avoid increase in PVR leading to R→L shunting: hypoxia, acidosis, hypothermia, pain treat metabolic acidosis replace significant blood loss Congenital Diaphragmatic Hernia Intraoperative Mechanical Ventilation adjust FiO2 to achieve PaO2 80 -100 mmHg SpO2 95 - 98% small tidal volume to keep airway pressure < 20-30 cm H2O high respiratory rate 60-120 /min to PaCO2 25-30 mm Hg Congenital Diaphragmatic Hernia Intraoperative Surgical repair primary closure staged procedure Transabdominal subcostal incision Thoracoscopic repair has been reported Congenital Diaphragmatic Hernia Intraoperative Potential Problems • Hypoxemia distension of stomach 1° pulmonary hypoplasia / pulmonary HTN • Contralateral pneumothorax • Hypotension or IVC compression • Cardiac arrest Congenital Diaphragmatic Hernia Postoperative Care Ventilatory support Close fluid management Hemodynamic monitoring “Honeymoon Period” followed by deterioration increase abdominal pressure impaired peripheral and visceral perfusion limited diaphragmatic excursion worsening of pulmonary compliance Congenital Diaphragmatic Hernia Management of PPHN • Minimize ETT suctioning • Vasodilators : rarely effective tolazoline isoproterenol nitroglycerin SNP PGE1 • Inhaled nitric oxide endothelium - derived relaxing factor (EDRF) selective pulmonary vasodilation rapidly metabolized has not been shown to improve survival Congenital Diaphragmatic Hernia Extracorporeal Membrane Oxygenation (ECMO) • Use: controversial • Allows the lungs to develop & restructure • Expensive • improved survival in neonates with > 80% mortality Congenital Diaphragmatic Hernia Criteria for ECMO • Gestational age ≥ 34 wks • Reversible disease process present • Weight ≥ 2000 grams • Predicted mortality ≥ 80% estimated by oxygenation index of > 40 FiO2 x mean airway pressure x 100 PaO2 Congenital Diaphragmatic Hernia Contraindications Gestational age < 34 wks Weight < 2000 grams Preexisting intracranial hemorrhage (≥ grade II) Aggressive respiratory treatment > 1 wk Congenital heart disease Congenital or neurological abnormality incompatible with good outcome TracheoEsophageal Fistula (TEF) Tracheoesophageal Fistula Incidence: 1:4000 live births M > F (25:3) 10-40% are preterm Antenatal history: polyhydramnios (60%) Etiology: failure in mesenchymal separation of upper foregut Tracheoesophageal Fistula Clinical Presentation choking on 1st feed coughing cyanosis excessive salivation aspiration pneumonia Tracheoesophageal Fistula Diagnosis • inability to pass a suction catheter into the stomach • CXR: coiled orogastric tube in the cervical pouch; air in the stomach and intestine Tracheoesophageal Fistula Esophageal Atresia Tracheoesophageal Fistula Turnage RH, et al, Sabiston Textbook of Surgery,17th Ed. 2004 TracheoEsophageal Fistula 5 Types (Gross and Vogt) 7.7% 0.8% 86% 0.7% 4.2% Gregory GA, ed, Pediatric Anesthesia, 3rd edition, 1996 Tracheoesophageal Fistula 35-65% have associated anomalies VATER and VACTERL V vertebral anomalies or VSD A anorectal malformation C cardiac anomalies (common) T TEF E esophageal atresia R renal abnormalities L limb/radial malformation Tracheoesophageal Fistula Preoperative Preparation Minimize pulmonary complication npo head-up position sump tube (repogle) on low continuous suction ± gastrostomy under local anesthesia CXR, abdominal x-ray, renal ultrasound 12-L EKG and Echocardiogram : mandatory IV access ± arterial line Tracheoesophageal Fistula Preoperative Preparation Laboratory studies CBC Electrolytes Glucose Calcium ABGs Tracheoesophageal Fistula Preoperative Preparation 24-48 hr medical stabilization Antibiotics: ampicillin and gentamicin Ensure availability of blood in the OR Optimize volume status and metabolic state Intubation preferably in the operating room under controlled situation Tracheoesophageal Fistula Intraoperative Management Main Concern oxygenation and ventilation securing the airway Monitors ASA standard ± invasive : arterial line * precordial stethoscope in the L axillary area Tracheoesophageal Fistula Intraoperative Management Anesthetic Technique • “classic approach” GA without muscle paralysis • combined light GA + epidural (Bosenberg) • GA with muscle paralysis Tracheoesophageal Fistula Intraoperative Management Induction • awake intubation • rapid sequence IV induction • inhalation induction spontaneous ventilation without muscle relaxant Tracheoesophageal Fistula Intraoperative Management Assessment of ETT position Goal: ETT just above the carina and just below the fistula • Right mainstem intubation and withdraw ETT until bilateral breath sounds • Left mainstem intubation: poorly tolerated due to insufficient pulmonary reserve Tracheoesophageal Fistula Intraoperative Management • If g-tube present, place end of g-tube under water seal: ETT above fistula → (+) bubbles • Connect capnograph to g-tube: (+) ETCO2 if ETT above the fistula • ? rigid bronchoscopy - not proven Tracheoesophageal Fistula Intraoperative Management Berry FA, Anesthetic Management of Difficult and Routine Pediatric Patients, 2nd Ed. 1990 Tracheoesophageal Fistula Intraoperative Management Beware of gastric distention gentle positive pressure ventilation gastrostomy: open if present TEF + RDS combination now what???!! gastrostomy under local anesthesia fogarty embolectomy catheter Tracheoesophageal Fistula Intraoperative Management Lateral decubitus position Posterolateral thoracotomy Maintenance of Anesthesia Narcotic technique Inhalation technique + regional anesthesia ? Use of nitrous oxide Tracheoesophageal Fistula Intraoperative Management Surgical repair • ligation of fistula check air leak in suture line • esophageal repair identify the pouch placement of feeding tube • chest tube placement and closure of thoracic cavity Tracheoesophageal Fistula Intraoperative Management Intraoperative problems • Endobronchial intubation • Intubation of fistula • Obstruction of ETT • V/Q mismatch lateral decubitus position nondependent lung retraction • Vagal response to tracheal manipulation • Return to transitional circulation and shunting Tracheoesophageal Fistula Postoperative Management Early extubation desirable caution: disruption of surgical repair with reintubation Postop Pain Management 1. IV narcotics 2. epidural infusion: 0.1% bupivacaine + fentanyl 0.5 mcg/ml at 01.-0.2 ml/kg/hr 3. rectal Tylenol + LA infiltration of incision Tracheoesophageal Fistula Main Cause of Mortality associated anomalies survival rates 85-90% Long Term Complications GE reflux anastomotic stricture tracheomalacia Abdominal Wall Defects Gastroschisis Omphalocoele Gastroschisis Greek word for “belly cleft” Evisceration of gut through a 2-3 cm defect in the anterior abdominal wall lateral to the umbilicus, usually on the right Absence of covering or sac chemical peritonitis infection ECF loss heat loss Incidence: 1:15,000-30,000 live births Gastroschisis Gastroschisis Etiology exact cause unknown Theories • intrauterine occlusion of omphalomesenteric artery → ischemia and atrophy of abdominal muscles • early fetal rupture of an omphalocoele Gastroschisis • rupture of umbilical cord at the site of the resorbed right umbilical vein • ? Maternal: smoking, ETOH, recreational drugs, medications (NSAIDS, pseudoephredrine) • associated anomalies - rare Omphalocoele Omphalocoele External herniation of abdominal viscera into the base of the umbilical cord through a central defect Defect: small or large Umbilical cord is inserted into the apex of the lesion Presence of covering or sac (amnion and peritoneum) Incidence: 1-5,000-10,000 live births Omphalocoele Omphalocoele Etiology • incomplete return of the gut to the abdominal cavity due to an abdominal lateral fold defect • Failure of migration and fusion of cranial, caudal and/or lateral folds of the embryonic disc at ~ 3rd wk of gestation Omphalocoele Cranial Fold : Pentalogy of Cantrell Epigastric omphalocoele Sternum cleft Diaphragmatic defect Ectopia cordis Cardiac anomaly Omphalocoele Lateral Fold omphalocoele with cord coming of the center of the sac Caudal Fold Hypogastric omphalocoele Extrophy of the bladder Imperforate anus Colonic agenesis Vesicointestinal fistula Omphalocoele Associated Congenital Anomalies: 75-80% chromosomal: trisomy 13, 15, 21 cardiac anomalies: 20% craniofacial gastrointestinal Beckwith-Wiedeman Syndrome omphalocoele microcephaly visceromegaly hypoglycemia macroglossia hyperviscosity Pentalogy of Cantrell Omphalocoele Survival: 20% with heart disease 70% without heart disease Major cause of mortality cardiac defects prematurity Definitive Treatment: surgical repair Incidence Peritoneal covering/sac Location of defect Herniated bowel Associated anomalies Gastroschisis Omphalocoele 1:15,000-30,000 1:6,000 absent present periumbilical matted, edematous low (10-15%) intestinal atresia (15%) within the umbilical cord normal high (40-60%) congenital heart dis. Beckwith-Weidman syndrome Gastroschisis Omphalocoele Abdominal Wall Defects Preoperative Management Anesthetic Concerns • Hydration / fluid status warm moist sterile saline-soaked gauze plastic bowel bag initial fluid requirement 10 -15 ml/kg/hr; higher with gastroschisis 100-200 ml/kg/hr • Heat loss : neutral thermal environment • Difficulties of surgical closure • Associated congenital anomalies & prematurity Abdominal Wall Defects Preoperative Management • Infection and postop nutrition • Postoperative ventilation • Airway • Metabolic status • Aspiration precautions • Direct trauma to herniated organ Abdominal Wall Defects Preoperative Management Lab workup CBC Electrolytes and Glucose ABG Ancillary Procedures CXR Echocardiography Abdominal Wall Defects Intraoperative Management Premedication: ± atropine IV access: 2 large bore IVs preferably above the diaphragm Monitors: ASA standard : 2 pulse oximeters invasive: arterial line ± CVP foley catheter intraop airway pressures Abdominal Wall Defects Intraoperative Management Choice of Anesthesia general anesthesia spinal (reported) in selected patients Induction decompress the stomach rapid sequence IV induction with cricoid pressure or inhalation induction and intubation or awake intubation Abdominal Wall Defects Intraoperative Management Maintenance of Anesthesia • Opiate technique or judicious use of inhalational agents • Avoid nitrous oxide • Adjust FiO2: PaO2 50-70 mmHg SpO2 97-98% term 87-92% preterm • Muscle relaxant facilitates abdominal closure Abdominal Wall Defects Intraoperative Management Prevent hypothermia full access body hugger heating blanket increase room temp plastic wrap fluid warmer Fluid requirement maintenance: D5 0.2% NS 3rd space loss replacement isotonic fluid 10 -15 ml/kg/hr blood loss from adhesions Abdominal Wall Defects Intraoperative Management Surgical Closure • optimal method remains controversial 1) primary fascial closure : 80% ± intraop and postop muscle paralysis 2) staged repair silicone elastometer pouch primary skin closure Abdominal Wall Defects Intraoperative Management • Closure dependent on the 1) size of the defect 2) development of abdominal wall 3) presence of associated anomalies Abdominal Wall Defects Intraoperative Management Primary Closure • monitor: airway pressure, O2 saturation and ABG • tight abdominal closure 1) impairs diaphragmatic excursion → ventilatory compromise 2) impedes venous return → profound hypotension 3) aortocaval compression → bowel ischemia, ↓ CO, renal and hepatic dysfunction, wound dehiscence Abdominal Wall Defects Intraoperative Management Unsafe for Primary Abdominal Closure • Intragastric pressure > 20 cmH2O • Intravesical pressure > 20 cmH2O • Change in CVP 4 ≥ mmHg • ETCO2 ≥ 50 mmHg • Peak inspiratory pressure ≥ 35 cmH2O Abdominal Wall Defects Intraoperative Management Staged Reduction • Dacron reinforced silastic silo • Gradual reduction over 1- 2 weeks • Ketamine or opioid ± muscle relaxant in intubated patients or • Titration of ketamine 0.5 -1 mg/kg IV with spontaneous breathing unintubated infants • Final closure in the OR Abdominal Wall Defects Intraoperative Management Silo closure Abdominal Wall Defects Intraoperative Management To extubate or not to extubate? • Size of patient • Intraoperative events • Prematurity • Associated pathology • Hemodynamic status • Magnitude of the abdominal defect • Type of repair Abdominal Wall Defects Postoperative Management NICU Postop ventilation in most neonates for 24-48 hrs Fluid requirements may remain high Prolonged postop ileus: TPN or PPN Prevent infection: higher with silo Watch for circulatory compromise cyanotic lower limbs Postop HTN due to ↓ renal perfusion and activation of renin-angiotensin-aldosterone Abdominal Wall Defects Early Postoperative Complications • Necrotizing enterocolitis • Renal insufficiency • Pneumonia • Abdominal wall breakdown • PDA • GE reflux Necrotizing Enterocolitis (NEC) Necrotizing Enterocolitis (NEC) Life-threatening intestinal inflammation or injury Caused by bacterial invasion of previously injured or ischemic bowel wall Incidence: 5 -10% in infants <1500g birth weight Mortality rate: 10 - 30% Necrotizing Enterocolitis (NEC) Single most important factor PREMATURITY Can occur in: premature infants LBW infants Full term infants fed and unfed infants Necrotizing Enterocolitis (NEC) Other factors ischemia bacterial infection GI endotoxemia enteral feeding use of hyperosmolar formula congenital heart disease hx of umbilical arterial catheterization hx of exchange transfusion Necrotizing Enterocolitis (NEC) Early signs ↑ gastric residuals with feedings temperature instability poor feeding bilious vomiting lethargy mucoid or bloody stool apnea and bradycardia Necrotizing Enterocolitis Late Signs Hemodynamic instability Anemia Thrombocytopenia Coagulopathy, DIC Prerenal azotemia Metabolic acidosis Necrotizing Enterocolitis (NEC) Physical Exam distended and tender abdomen Labs: CBC electrolytes and glucose platelets and coagulation profile DIC profile ABG Necrotizing Enterocolitis (NEC) Abdominal X-ray • signs of bowel obstruction • ileus with edematous bowel • Pneumatosis intestinalis or intramural air (arrow) • portal vein air • pneumoperitoneum Necrotizing Enterocolitis (NEC) Medical Management initial treatment, for 7-10 days 75% successful Surgical Treatment 10 - 50% mortality Necrotizing Enterocolitis (NEC) Medical Management • No enteral feedings for 10-14 days • NGT on intermittent suction • Hydration and correction of electrolytes • Ventilatory support • Antibiotics • Blood and platelet transfusion if needed Necrotizing Enterocolitis (NEC) Surgical Indications • Absolute Indications 1) bowel perforation new mx: peritoneal drains under local anesthesia 2) intestinal gangrene Necrotizing Enterocolitis (NEC) • Relative Indications • clinical condition metabolic acidosis respiratory failure oliguria, hypovolemia thrombocytopenia leucopenia, leukocytosis • air in the portal vein • bowel wall edema • persistent dilated bowel loops Necrotizing Enterocolitis • Non-Surgical Indications severe GI hemorrhage abdominal tenderness intestinal obstruction gasless abdomen with ascites Necrotizing Enterocolitis (NEC) Preoperative Management Anesthetic Concerns • Fluid/volume status • Significant 3rd space loss • Full stomach / pulmonary aspiration • Metabolic abnormalities acidosis, hyperglycemia Necrotizing Enterocolitis (NEC) Preoperative Management • Electrolyte imbalance: hyperkalemia • Coagulopathy: thrombocytopenia • Respiratory failure • Sepsis / hemodynamic instability inotropic support dopamine infusion Necrotizing Enterocolitis (NEC) Intraoperative Management Adequate IV access Monitors: ASA standard invasive: arterial line, ± CVP foley catheter Induction rapid sequence if not intubated Necrotizing Enterocolitis (NEC) Intraoperative Management Maintenance of Anesthesia • Narcotic based technique • Avoid nitrous oxide • Inhalational agents poorly tolerated • Massive fluid requirements • PRBC, FFP and platelets transfusion Necrotizing Enterocolitis (NEC) • Avoid hypothermia • Give blood early when indicated Postop Management • NICU • Postop ventilation required • Continue resuscitation • Parenteral Nutrition Summary • Almost all neonatal surgical “emergencies” are really “urgencies” • Immaturity of organ system in neonates alters pharmacology and physiology • Thorough preop assessment is required in all neonates • One anomaly mandates a search for others • Murmurs necessitate a cardiology consult • Successful perioperative outcome depends on open communication and teamwork between neonatologist, anesthesiologist and surgeon • Initial resuscitation of neonatal surgical candidates includes: airway protection adequate IV access fluid resuscitation temperature stabilization gastric decompression administration of antibiotics identify associated anomalies Omphalocoele Embryology Failure of the midgut to return to the abdominal cavity by the 10th wk of gestation