Cost Analysis - Introduction
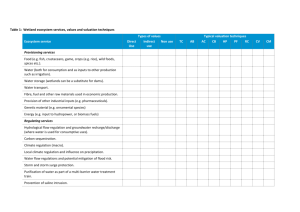
advertisement

Cost Analysis Dr Rakesh Kumar Moderator- Dr PR Deshmukh Framework Introduction What is cost analysis and economics analysis Uses of Cost- Analysis Steps in Cost- Analysis ◦ Planning a cost analysis study ◦ Calculating costs ◦ Measuring outcomes ◦ Applying cost analysis methods ◦ Analysis, interpretation & presentation Strengths and limitations of cost- analysis References Some Questions ??? 1. What has been expenditure and revenues on a project ? What is the averageDistribution cost of providing a service? 2. What are the trend? of costs 3. Does expenditure compares with the budget? Input category Facility or location Service type or activity What is Cost Analysis Definition:• It is the element-by-element examination of the expenditure to determine how resources have been spent. A critical process needed to solve management problems Helps to understand how funds have been used Guides in optimal utilization of scarce resources Uses of Cost Analysis 1. Accountability- Keeping track 2. Assessing Efficiency 3. Assessing Equity 4. Assessing Priorities 5. Making cost projections 6. Considering cost recovery Economical And Financial Cost Analysis Variable Costs Financial analysis Monetary cost. Economic analysis Economic (“opportunity”) cost. e.g, actual monetary payments e.g, volunteer workers and donated for human resources, materials, goods or infrastructure Outcomes Valuation using market interest rates. Valuation using a discount rate Income; expenditure; cash flow; profit; end-of-period balance; internal financial rate of return; net present financial value. Benefit–cost ratio; internal economic rate of return; net present value. Financial consequences Resource consequences Steps for Cost-Analysis Research Question Plan Cost- Analysis study •Setting scope of study •Deciding on time trend •Selecting sample •Drawing iternary & checklist Cost estimation Identification and choice of costs Quantification of costs Valuation of costs Adjustment for differential timing Impact estimation Identification and choice of impacts Quantification of impacts Valuation of impacts Adjustment for differential timing Appropriate cost analysis methods Assessment of Impact of uncertainty Analysis, Interpretation and Presentation Planning Cost- Analysis Study Setting scope of study Deciding on time trend Selecting sample Drawing iternary & checklist Cost- Estimation Identification of main costs and their sources Quantification of costs Valuation of costs and discounting. Identification of costs and their sources Intervention Direct Cost Health services resource use. Eg. Inpatient, outpatient, tests, drugs Non-health services Eg. Patient transportation, Administration Research & Development Indirect Costs Wider cost implications to society eg. lost production. Time receiving medical care ◦ Perspective is important ◦ Range of costs justified by perspective Costs to family and friends. Sources of cost data Routine Information Survey : ◦ Market prices & Labor statistics Periodic information sources◦ contracted company, ◦ government ministry or ◦ NGO Specialist surveys or studies ◦ Household surveys ◦ scientific studies Expert opinion Quantification of cost data Need to quantify resource use in appropriate physical and natural units ◦ hours, days, miles etc Direct costs are mostly assessed, and categorised as: ◦ Capital costs (buildings, equipment) ◦ Overheads (jointly used resources, such as heating and lighting, administration and catering) ◦ Labour (medical and non-medical staff) ◦ Consumables (disposable items, such as drugs, bandages etc) Need to distinguish between fixed, variable and total cost, and average, marginal costs and incremental cost Fixed, variable and total cost Cost Total cost: all costs incurred while producing a service Variable cost : vary with level of service. E.g. consumables Fixed cost - do not vary with quantity in short run e.g. Capital costs Quantity Average and marginal cost curves Cost Marginal cost TC Q cost of producing an extra unit Average cost TC Q cost per unit of output Quantity Marginal versus incremental cost Cost TC of Prog A ICA-B, Q MCA, Q TC of Prog B MCB, Q Q Quantity Discounting To allow for differential timing of costs (and benefits) between programmes all future costs (and benefits) should be stated in terms of their present value using discount rate Prefer to have benefits now and bear costs in the future – ‘time preference’ ‘Rate’ of time preference is termed ‘discount rate’ Discounting example Valuation Resources should be valued according to their opportunity cost Method of valuation needs justification (Market prices or ‘Shadow’ price ) Health care provision is rarely subject to market valuations Alternative ‘shadow’ prices may need to be used Unit cost data may need to be adjusted for Price inflation (costs from different years) ◦ weighted average of Pay Cost Index (PCI) and Health Service Cost Index (HSCI) 1. 2. International currencies (costs from different countries)◦ Purchasing Power Parities (PPPs) and exchange rates ◦ PPPs are more appropriate Measuring Outcome/ consequences Identification ◦ ◦ Depends upon viewpoint (govt., societal ) Depends on the objective of the evaluation Measurement- Valuation- in terms of: ◦ Measure outcome in natural physical units ◦ Utility (eg QALY) ◦ Money (eg WTP) Cost Analysis Methods 1. 2. 3. 4. 5. 6. Cost-effectiveness analysis (CEA): Cost-utility analysis (CUA) Cost-benefit analysis (CBA): Cost-of-illness analysis: Cost-minimization analysis: Cost-consequence analysis: Cost-Effectiveness Analysis A comparison of costs in monetary units with outcomes in quantitative non-monetary units, e.g., reduced mortality or morbidity Target and output indicators pre-decided Most appropriate if the important outcome is uni- dimensional Compare costs of at least two alternatives Cost- Effectiveness Ratio: CE Ratio = ($ Cost Int - $ Cost Comp) / ($ Effect Int - $ Effect Comp) For example: “$45,000 per life- year saved” or $10,000 per lung cancer case averted” Cost-Effectiveness Analysis cont… Advantages 1. Useful to know the cause of failure to attend the objective and the unmet demand. 2. Adequacy of corrective action taken, can be reviewed Disadvantage 1. Only compare programs with similar outcomes 2. There is not enough information to assign a value to the outcome 3. Methodological inconsistency 4. Ambiguity in assessing overall improvement or decrement in health 5. Cannot address the issue of allocative efficiency Cost-Utility Analysis A type of cost-effectiveness analysis It compares costs in monetary units with outcomes in terms of their utility, usually to the patient, measured, e.g., in QALYs Measures of different effects are consolidated into a common abstract scale Example; Quality adjusted life year (QALY), Disablity adjusted life years (DALYs) Most appropriate if the important outcome is multidimensional Disadvantage Difficult to assign utility weights Cost- Utilty Ratio: CU Ratio = ($ Cost Int - $ Cost Comp) / ($ Utile Int - $ Utile Comp) For example: “$10,000 per QALY gained” Quality-adjusted life years (QALYs) Adjust quantity of life years saved to reflect a valuation of the quality of life ◦ If healthy QALY = 1 ◦ If unhealthy QALY < 1 ◦ QALY can be <0 Procedure ◦ Identify possible health states - cover all important/relevant dimensions of QoL ◦ Derive utility ‘weights’ for each state ◦ Multiply life years (spent in each state) by ‘weight’ for that state. Quality adjustment utility “weights” should (1) be preference-based (2) be interval-scaled (3) contain both perfect health and death on the same scale Techniques to ‘weight’ utility Direct methods ◦ Measure the preferences of individuals directly using general instruments like the visual analogue scale, the time trade-off method, and the standard gamble technique ◦ Widely applied ◦ Costly & time consuming Indirect methods ◦ Simpler to use (though difficult to develop) ◦ Based on multi-attribute health status classification systems.(consist of a set of attributes of health status (e.g., pain and discomfort, visual acuity, ambulation, cognitive function, etc.), and levels of function associated with each attribute from full function to impaired function (e.g. perfect vision — totally blind) Cost-Benefit Analysis It compares costs and benefits, both of which are quantified in common monetary units Unique feature that can indicate explicitly whether benefits outweigh costs Advantage: ◦ Can address allocative efficiency ◦ Can compare disaperate technologies Disadvantage: ◦ Difficult to assign monetary value to outcomes Cost-Benefit Analysis cont… Two approaches: Cost- Benefit Ratio: (Ratio Approach) CB Ratio = ($ Cost Int - $ Cost Comp) / ($ Benefit Int - $ Benefit Comp) For example: “Cost Benefit ratio of 1.5” Cost- Benefit Ratio: (Net Benefit Approach) CB Ratio = ($ Cost Int - $ Cost Comp) - ($ Effect Int - $ Effect Comp) For example: “Net cost of $15,00” Monetary Valuation Earlier “Human Capital’ method were used Willingness To Pay Method Done by Contingency valuation method Assess individual ‘willingness-to-pay’ for (the benefits of) a good through either: 1. Observed wealth-risk trade-off (revealed preference) ◦ Advantage – ‘real’ preferences/values ◦ Disadvantage – difficult control for confounders 2. Direct survey (stated preference) ◦ Advantage – direct valuation of good ◦ Disadvantage – hypothetical/survey problems Vast majority of CBA use direct survey Cost of Illness Analysis A determination of the economic impact of an illness or condition . Cost of Illness includes: Medical care for prevention, treatment & Social services for rehabilitation Productivity loss Examples o What does cancer cost the India? o What does blindness cost the world? Just because something has the highest cost of illness does not imply that it necessarily should have the most resources directed toward research or cure Depends on how much it will cost to do something about it Cost - Minimization Analysis A determination of the least costly among alternative interventions Calculate the cost of the different methods of achieving the objective Needs at least two ways of achieving the objective Example Rabies vaccination: Intramuscular or Intradermal schedule? Which is least costly? If so, should we continue Intramuscular schedule or use intradermal schedule? These studies are difficult because they don’t focus on partial outcomes Need a high degree of certainty that outcome can be obtained or else these studies are not particularly helpful Summary of Cost- Analysis Methods Valuation of costs (in Monetary units) Cost Effectiveness $ Cost Benefit $ Cost Utility $ Cost of Illness $ Cost Minimization $ Valuation of outcomes Comments It can only compare technologies ÷ Natural units whose outcomes are measured in the same units ÷ or – •It enables comparison of disparate i.e, Ratio technologies Approach $ or Net •Difficult to assign monetary Benefit values to all pertinent outcomes Approach Utilities (e.g., It enables comparisons of disparate ÷ QALYs) technologies A determination of the economic vs. None impact of an illness or condition . Assume same A determination of the least costly vs. outcome among alternative interventions Dealing with uncertainty 1. Sensitivity analysis ◦ Systematically examining the influence of uncertainties in the variables and assumptions employed on the estimated results Steps: Identifying the (uncertain) variables ◦ All variables in the analysis are potential candidates ◦ Give reasons for exclusion rather than inclusion 2. Specifying the plausible range over which they should vary ◦ Reviewing the literature ◦ Consulting expert opinion 3. Recalculating results based on combinations of the best guesses, most and least conservative, usually based on… ◦ One-way analysis (each variable separately) ◦ Multi-way analysis (number of variables together) ◦ Threshold analysis (amount of variance needed to achieve specified result) Analysis, interpretation & presentation Set up "dummy tables" and graphs at initial phase Analysis should include interpretationi.e. What do the data mean? Finally, Report the result ◦ Stick to objective ◦ Keep presentation simple and use tables & graphs ◦ Write an executive summary Strengths & Limitations Strengths o a very useful tool for the manager and policy maker o In the absence of certainty, even approximations can help improve decision-making Limitations o It's difficult to estimate "true costs" or opportunity cost o Allocation of costs; often very difficult References Creese A, Parker D. Cost Analysis in Primary Health Care. A training manual for programme managers. Geneva: World Health Organization; 1994. Torres T, Baltussen R, Adam T, Hutubessy R, Acharya A, EvansD, Murray C. WHO Guide to cost effectiveness analysis. Geneva: World Health Organization; 2003. Hutton G, Rehfuess E. Guidelines for conducting cost–benefit analysis of household energy and health interventions. Geneva: World Health Organization; 2006. Module E Cost and Sustainability analysis. Aga Khan Foundation Cost Analysis Methods. Available from URL: www.nlm.nih.gov/nichsr/ Thanks