Student notes in ppt
advertisement

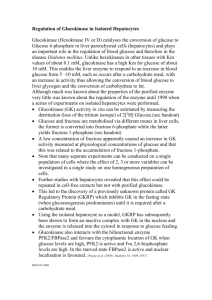
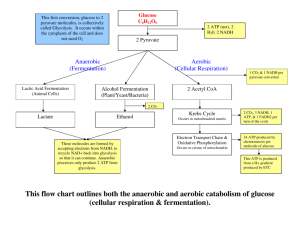
Glycolysis 2: Regulation of glycolytic flux, entry and exit of glycolytic metabolites, and pyruvate metabolism Bioc 460 Spring 2008 - Lecture 26 (Miesfeld) Glycolytic flux is regulated in part by PFK-1 activity; a metabolic “valve” in the pathway Lactose intolerance is due to insufficient lactase enzyme This is the chemical structure of which glycolytic metabolite? Key Concepts in Glycolysis • Glucokinase (hexokinase IV) catalyzes reaction 1 in the glycolytic pathway in liver and pancreas cells when blood glucose levels are high. Unlike hexokinase I, glucokinase as a very low affinity for glucose and is not inhibited by glucose6P. Therefore after a meal, the liver accumulates glucose for glycogen synthesis, and the insulin secretion pathway is activated in pancreatic cells. • Phosphofructokinase 1 (PFK-1) is one of three metabolic “valves” in the glycolytic pathway. PFK-1 is allosterically activated by fructose-2,6-BP, AMP, and ADP (low energy charge), whereas, it is allosterically inhibited by ATP and citrate (high energy charge). AMP stabilizes the R form of the enzyme (active), and ATP stabilizes the T form (inactive). The activity of pyruvate kinase is controlled by both phosphorylation and allosteric regulation. • Disaccharide sugars (maltose, sucrose, lactose) are cleaved by specific enzymes to produce glucose and other monosaccharide sugars that enter the glycolytic pathway. Glycolytic intermediates are metabolites in amino acid biosynthesis, pentose phosphate pathway, and triacylglyceride biosynthesis. • Regeneration of NAD+ in the cytosol is critical to maintaining glycolytic flux through the glyceraldehyde-3-P dehydrogenase reaction (reaction 6). Glucokinase is a sensor of high glucose levels Hexokinase I – high affinity for substrate (Km for glucose is ~0.1mM) – expressed in all tissues – phosphorylates a variety of hexose sugars – inhibited by the product of the reaction, glucose-6-P Glucokinase (Hexokinase IV) – low affinity for substrate (Km for glucose is ~10mM) – highly specific for glucose – expressed primarily in liver and pancreatic cells – not inhibited by glucose-6-P Two Major Roles of Glucokinase Role in liver cells When blood glucose levels are high, both hexokinase I and glucokinase are active in liver cells, whereas, other tissues only have hexokinase 1 and their ability to take up glucose after a meal is unchanged. Since phosphorylation traps glucose inside cells, and reaction 1 of glycolysis (same reaction catalyzed by both hexokinase 1 and glucokinase) is highly favorable, liver cells take up a disproportionate amount of the elevated blood glucose. Role in pancreatic β cells Glucokinase also sequesters glucose inside the pancreatic cells which initiates a complex signaling pathway leading to the release of insulin into the blood. Since insulin signaling results in lowered blood glucose levels by activating glucose uptake in the muscle and fat cells (adipose), glucokinase is vital to glucose control. Homeostatic blood glucose levels are ~5mM which saturates hexokinase I activity in all tissues. However, after a carbohydrate-rich meal (glucose is plentiful), blood glucose levels increase dramatically and the glucokinase reaction in liver and pancreas cells becomes a major contributor to the formation of glucose-6-P. Since glucose-6-P is trapped in the cell because of the negative charge, the liver and pancreas accumulate a large share of the blood glucose. Glucokinase is a Sensor of Glucose Levels GLUT protein is a glucose transporter. Glucose activation of glucokinase activity is at the level of protein synthesis, i.e., elevated glucose in the cell leads to increased synthesis of glucokinase enzyme. What happens to flux through the glycolytic pathway when glucokinase is activated by glucose? Increased ATP levels stimulate membrane depolarization and subsequent calcuim uptake. Making a glucokinase knock-out mouse The importance of glucokinase in insulin secretion was confirmed using transgenic mice that lacked the glucokinase gene in pancreatic cells. Since these mice cannot secrete insulin when blood glucose levels were high, they developed insulindependent diabetes. Human metabolic diseases are often caused by non-lethal recessive gene mutations in enzymes Over 150 mutations in the glucokinase gene have been found in humans with a form of diabetes called mature-onset diabetes of the young (MODY2). Allsoteric regulators control the activity of phosphofructokinase 1 and modulate glycolytic flux Phosophofructokinase-1 (PFK-1) • catalyzes reaction 3 in glycolysis to generate fructose-1,6- BP PFK-1 Phosphofructokinase-2 (PFK-2) • bifunctional enzyme that catalyzes the synthesis of fructose-2,6-BP (F-2,6-BP), a potent allosteric regulator of PFK-1 activity. We will talk more about the synthesis of F-2,6-BP later in the course. Allosteric regulation of PFK-1 • PFK-1 exists as a homotetramer (a dimer of dimers). • It is stable in two conformations; the inactive T state or active R state (similar to to the T and R conformations of hemoglobin). • The activity of PFK-1 is allosterically activated by binding of F-2,6-BP, AMP, and ADP, and it is allosterically inhibited by citrate and ATP. Allosteric regulators alter the activity of PFK-1 by binding to a region outside of the active site ATP and AMP binding to PFK-1 shifts the equilibrium between the T and R conformations What are the two roles of ATP in the PFK-1 catalyzed reaction? The activity of liver pyruvate kinase is controlled by both phosphorylation and allosteric regulation When blood glucose levels are high, glycolytic flux is stimulated in part by dephosphorylation of liver pyruvate kinase. Conversely, low blood glucose levels leads to phosphorylation and partial inactivation of pyruvate kinase. Feed forward allosteric regulation by fructose1,6-BP, and allosteric inhibition by ATP and alanine, also control pyruvate kinase activity. Based on what you know about the structure of pyruvate and alanine, why do you think alanine is a negative regulator of pyruvate kinase activity? Supply of Glycolytic Intermediates Disaccharide sugars are common nutrients in our diet and provide much of the carbohydrate used for energy conversion. - Maltose is from starch - Sucrose is table sugar - Lactose is from milk Glycerol is a glycolytic intermediate derived from the degradation of triacylglycerides. Lactose intolerance occurs in most adults as a result of decreased lactase enzyme production Lactose is present at high levels in milk products and can cause considerable intestinal discomfort in people with reduce lactase gene expression. This is most common in people of Asian decent and is rarely found in people from a Scandinavian background. High levels of intestinal lactose causes osmosis of water into the intestine leading to diarrhea, and moreover, anaerobic intestinal bacteria metabolize the extra lactose to produce H2 and CH4 gas. Two ways for adults to still enjoy dairy products are to predigest the lactose sugar by adding lactase to yogurt or milk before consuming, or to take a lactase supplement pill before eating dairy foods. Fructose, galactose and glycerol enter the glycolytic pathway through a variety of routes, many of which require additional enzymatic reactions. For example, fructose is first converted to fructose-1-P which is then cleaved by fructose -1-P aldolase to generate DHAP and glyceraldehyde which is then phosphorylated to produce GAP. Does the number of ATP required to convert 1 mole of fructose into 2 moles of pyruvate differ in liver and muscle cells? The metabolic disease fructose intolerance is due to a deficiency in the enzyme fructose-1-P aldolase • High fructose corn syrup is the most common added sweetener to processed foods, however, for individuals with fructose intolerance, fructose in the diet can be extremely toxic. • Prolonged ingestion of fructose, primarily from fruit juice, leads to the build-up of fructose-1-P which results in loss of Pi in the liver and decreased ATP synthesis (ADP + Pi --> ATP) causing liver damage. What do you think the treatment is for people with fructose intolerance? Demand for Glycolytic Intermediates In addition to functioning as intermediates in the gluconeogenic pathway (production of glucose from non-carbohydrate sources), many of the glycolytic metabolites provide carbon skeletons for amino acid synthesis, the pentose phosphate pathway (ribose-5-P), and triacylglyceride synthesis (glycerol). Metabolic Fate of Pyruvate 1. Under aerobic conditions, the majority of pyruvate is metabolized in the mitochondria to acetyl CoA, and ultimately to CO2 and H2O which are the products of the citrate cycle and electron transport chain. 2. Under anaerobic conditions, such as occurs in muscle cells during strenuous exercise, or in erythrocytes which lack mitochondria, pyruvate is converted to lactate (the ionized form of lactic acid) by the enzyme lactate dehydrogenase. 3. Under anaerobic conditions in microorganisms such as yeast, pyruvate can also be utilized for alcoholic fermentation to convert pyruvate to CO2 and ethanol using the enzymes pyruvate decarboxylase and alcohol dehydrogenase, respectively. NAD+ must be regenerated to maintain glycolytic flux The glyceraldehyde-3-P dehydrogenase reaction requires a steady supply of NAD+ which functions as a coenzyme in this oxidation reaction. Anaerobic respiration replenishes the NAD+ through a reduction reaction leading to lactate or ethanol production. Aerobic respiration replaces the NAD+ through a metabolite shuttle system since NAD/H cannot cross the mitochondrial membrane. Glyceraldehyde-3-P Anaerobic Regeneration of NAD+ NAD+ + Pi NADH + H+ Glyceraldehyde-3-P dehydrogenase 3-Pglycerate 1,3-BisPglycerate ADP Pglycerate ATP kinase Phosphoglycerol mutase Enolase Phosphoenolpyruvate 2-Pglycerate ADP Pyruvate kinase NAD+ Lactate NADH + H+ ATP Pyruvate Lactate dehydrogenase Lactate Dehydrogenase Deficiency (LDHA) These patients cannot maintain moderate levels of exercise due to an inability to utilize glycolysis to produce ATP needed for muscle contraction under anaerobic conditions. When lactate dehydrogenase levels are insufficient, the level of NAD+ becomes limiting during exercise and flux through the glyceraldehyde-3-P dehydrogenase reaction is inhibited.