Hypoxia and Equipment Failure
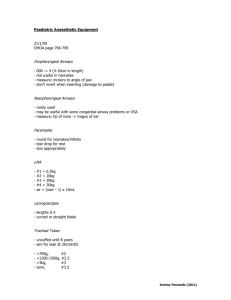
advertisement
April 25, 2011 Case Stem: A 70 year old man is to undergo cystoscopy and transurethral resection of a bladder tumor under general anesthesia through an LMA. He gave a history of mild asthma and used an albuterol inhaler when necessary. Breathing room air (FiO2 = 0.21), his pulse oximeter saturation reading (SpO2) was 94%. Hypoxia Reduction of oxygen supply to tissue below physiologic levels. Decreased oxygen tension (PO2) inside the body at tissue level or outside the body (hypoxic gas mixture) Hypoxemia Deficient oxygenation of blood. Decreased oxygen tension in the arterial blood (PaO2) Yes. Age-dependent decrease in PaO2. Marshall and Whyche equation Mean PaO2 (mmHg) = 102-0.33(age in years) Sorbini et al. found PaO2 decreased from about 95 mmHg at 20 years of age to 73 at 75 years (about 4-5 mmHg per decade) No. Hypoxemia is considered to exist when the PaO2 is less than 60 mmHg which is equivalent to a hemoglobin O2 saturation of 90% Using the Marshall Whyche equation 102-0.33(70) = 79 mmHg Pulse Oximeter Noninvasive device that provides an estimate (SpO2) of the arterial hemoglobin saturation with oxygen. Uses patient body part as in vivo cuvette through which 2 different wavelengths of light are transmitted. Hemoximeter Used to analyze an arterial blood sample. Laboratory cooximeter that uses six or more different wavelengths of light to measure total hemoglobin, oxygenated hemoglobin, deoxygenated hemoglobin, methemoglobin, carboxyhemoglobin and other aberrations. Pulse oximeter Light-emitting diodes transmit red light at wavelengths 660 nm and infrared light at 960 nm through the probe site. Light is sensed by a single photodetector Ratio of absorbances (660/990 nm) is related to hemoglobin O2 saturation (Spectophotometry) Plethysmography – detection of pulsatile flow (as blood pulses, absorbance increases) Pulse oximeter Patient movement (shivering, peripheral nerve stimulation, “twitching”) Presence of intense ambient light Electrocautery use Administration of IV dyes with absorbance peaks at 66o nm (methylene blue) Dyshemoglobinemias Nail polish Poor pulsatile flow at probe site (hypotension, Raynaud’s) Venous pulsations (tricuspid regurg) Methemoglobin Iron in heme moiety is oxidized (dapsone, benzocaine, nitric oxide, prilocaine) to Fe3+ state rather than Fe2+ state. Cannot carry O2 Shows similar absorbances at 660 and 940 nm (SpO2 tends toward 85%) Overestimates the fractional saturation and underestimates the functional saturation Carboxyhemoglobin CO + Hb has similar absorbance to HbO2 at 660 nm, but very low absorbance at 94o nm. SpO2 overestimates fractional saturation and underestimates functional saturation. SpO2 will appear in the 90s Hemoximeter required to determine true O2 sat Capnography Most use infrared spectroscopy to measure PCO2 A built in barometer measures barometric pressure so that CO2 can be displayed as a percentage. “Gold standard” for establishing presence of ventilation. End-tidal CO2 Tension of CO2 in the exhaled gas at end of exhalation. Represents the CO2 tension in the alveolar gas (PACO2) Does not account for dead space ventilation Presence of CO2 depends on Production of CO2 by the tissues CO and pulmonary blood flow to carry CO2 Ventilation Capnogram Phase I – Expiratory baseline Phase II – Expiratory upstroke Phase III – Expiratory plateau Horizontal in healthy lungs Upward Slope with obstructive airway disease Maximum expired CO2 is considered the end-tidal α angle – slope between II and III (increase in acute bronchospasm) Phase IV – Inspiratory downstroke Elevated baseline CO2 Capnometer not properly calibrated to zero Delivery of CO2 to breathing system through fresh gas inflow Incompetent unidirectional valves Failure of CO2 absorber (channeling, exhaustion, bypass) Prolonged expiratory plauteau and expiratory upstroke Mechanical obstruction to exhalation COPD Bronchospasm Dips in expiratory plateau Spontaneous ventilation efforts Cardiogenic oscillations Ventilator pressure relief valve pertubations Elevated expiratory plateau Incorrect calibration Increased CO2 production / delivery Laparoscopic CO2 gas insufflation Decreased CO2 removal Hypoventilation Leak Decreased expiratory plateau Incorrect calibration Air leak into gas sampling system Hyperventilation Decreased CO2 production (hypothermia) Increased arterial-alveolar CO2 gradient (VQ mismatch / pulmonary embolus) Prolonged inspiratory downstroke and raised baseline Incompetent or missing inspiratory unidirectional valve Inspiratory obstruction to gas flow (kinked tube) A-a gradient Measure of alveolar dead space ventilation 2.5cc / Kg = volume of anatomic dead space (PaCO2 – PETCO2) / PaCO2 = Ratio of dead space to tidal volum Alveolar dead space increased by ventilation in excess of perfusion or decrease in perfusion (shunt has minimal effect) PaCO2-PACO2 – nl 3-5 mmHg Safety Features Pin index (cylinder) and diameter index (pipeline) safety systems “Fail-safe” valve – pressure sensitive device that interrupts flow of all hypoxic gases on the machine to their flow control valves if the supply pressure of O2 in the high pressure system falls below a threshold (between 12-20 psig) O2 supply failure alarm – pressure below 30 psig O2 flow control knob – fluted and on the right Key-fill systems for vaporizers Pop-off (pressure relief) valve Safety Features Gas flow proportioning – ensure minimum O2 of 25% when N2O is used Vaporizer interlock system Gas Leakage Breathing system Partially deflated tracheal tube cuff Disconnection of sidestream gas analyzer Humidifiers Bag Low-pressure machine components Cracked rotameter flow tubes Incorrectly mounted vaporizers Vaporizer leak around agent filling device Fracture in gas piping Machine Check for Leaks Drager Circle breathing system tubing removed Insp and exp limb connected by tubing Resevoir bag removed and replaced with test terminal with sphygmomanometer bulb Pressurize with bulb to 50 cm H2O – pressure should not decrease by 20 in 30 sec Test with vaporizers on Datex-Ohmeda One-way outlet check valve at the common gas outlet Connect bulb and squeeze, should not refill in 30 sec Step 1 – Emergency Ventilation Equipment Step 2 – Check O2 Cylinder supply Step 3 – Central pipeline supply Step 4 – Low-pressure system check (flow control valves and vaporizer status) Step 5 – Leak check of low-pressure system Step 6 – Turn on machine master switch and other electrical equipment Step 7 – Test flowmeters Step 8 – Adjust / Check scavenging system (test pop off) Step 9 – Calibrate O2 monitor Step 10 – Check initial status of breathing system (circuit, CO2 absorbent) Step 11 – Leak check of breathing system Step 12 – Test ventilation system (connect resevoir bag to Y-piece) Step 13 – Check, calibrate, and set alarm limits Step 14 – Check final status of machine Emergency Equipment Back-up ventilation equipment Emergency airway equipment Cricothyroid kit / Difficult airway cart Working flashlight Backup battery O2 tank and regulator Malignant hyperthermia cart “Code” cart Fire extinguisher Premedication Anxiolysis Minimization of gastric volume and acidity Antibiotic prophylaxis Antisialagogue effect Standard ASA Monitors Standard I – Qualified anesthesia personnel shall be present in the room throughout the conduct of all general, regional, and monitored anesthetic care. Standard II – During all anesthetics, the patient’s oxygenation, ventilation, circulation, and temperature shall be continually evaluated. Standard ASA Monitors Oxygen analyzer with low O2 alarm Quantitative method of blood oxygenation (pulse ox) Ventilation evaluation (chest rise, auscultation) Correct positioning of airway devices End-tidal CO2 with airway devices Ventilator disconnection alarm ECG, BP, HR (every 5 min for the latter 2) Body temperature (if perturbations are expected) Interventions Assess for airway obstruction, bilateral breath sounds, quality of breath sounds Check FiO2, ETCO2, HR, BP, SpO2 Bladder intake and output IV fluid intake Increase FiO2 to 100% Consider assisted ventilation If no improvement, tracheal intubation and PPV Common Leak Sites Incomplete tracheal cuff seal Elbow End-tidal monitoring connections Inspiratory and expiratory hoses Unidirectional valves, Pop-off valve, resevoir bag, bellows, absorber, vaporizers, flowmeters, scavenging system Extubation Criteria Global criteria Return of consciousness Demonstration of ability to protect airway Adequate reversal of NM blockade Absence of hypothermia Presence of nl metabolic milieu Respiratory criteria Vital capacity > 15ml per kg NIF < -20 cm H2O SpO2 > 90% on FiO2 <0.4 Rapid Shallow Breathing Index Patient observed breathing a T-bar or low Pressure support RSBI = RR (bpm) / tidal volume (L) RSBI > 100 – Patient will probably fail extubation If develops diaphoresis, agitation, tachycardia, bradycardia, HTN, hypotension – failed trial Postop Hypoxemia Physiologically Low FiO2 Hypoventilation VQ mismatch Shunt Pathologically Airway obstruction Atelectasis R Mainstem intubation Aspiration Pulmonary edema Pulmonary embolus Shunt Perfused but not ventilated PaO2 will not rise with increased FiO2 once shunt fraction approaches 30% Dead Space Ventilated but not perfused Failure to maintain normal PaCO2 despite increased MV (tv x rr) Pulmonary Edema Condition Pathophysiology Congestive Heart Failure filling pressure, CO Negative Pressure Pulmonary outside-inside pressure Edema Acute Lung Injury and ARDS gradient Permeability ARDS Mechanical Ventilation TV < 6ml / kg PIP < 35 cm H2O Consider PEEP of 10 cm H2O