O 2
advertisement
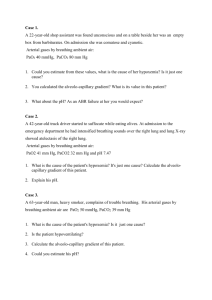
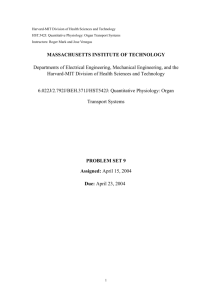
Unit I Oxygen Delivery: Heart, Lungs and RBCs Michel Désilets Objectives Trace the oxygen delivery system from ambient air to the cellular level. Define oxygen content, oxygen saturation and partial pressure of oxygen. Describe the mechanisms of hypoxemia and relate them to their position in the alveolar O2 equation. Compare the effects of methemoglobin and sulfhemoglobin on oxygen delivery and content as a method to understand oxygen delivery. Outline the methods of clinical and laboratory assessment of cyanosis, hypoxemia and tissue hypoxia. Oxygen delivery system Inspired tracheal air (humidified) PEO2 = 116 PECO2 = 32 PO2 = 160 PCO2 = 0.3 PIO2 = 150 PICO2 = 0.3 PAO2 = 102 PACO2 = 40 PvO2 = 40 PvCO2 = 45 PaO2 = 95 PaCO2 = 40 Rhoades & Bell. Medical Physiology. Principles for Clinical Medicine, 3rd Ed. , 2009 Symbols P = partial pressure (mm Hg) I = in inspired air (humidified) E = in expired air A = in alveolar air a = in arterial blood v = in venous blood Oxygen delivery system The oxygen cascade Symbols P = partial pressure (mm Hg) atm = in atmospheric air I = in inspired air (humidified) E = in expired air A = in alveolar air c = in end pulmonary capillary a = in arterial blood v = in venous blood PatmO2 http://www.prognosis.org/physiology/index.php (Also, for more details: http://www.altitude.org/oxygen_delivery_model.php) Oxygen delivery system 1. Pulmonary ventilation: from atmosphere to alveoli • Dry air in atmosphere (barometric pressure) = 760 mm Hg PO2 + PN2 PatmO2 = FIO2 x 760 = 0.21 x 760 = 160 mm Hg (FIO2 = Fraction of O2 in inspired dry air) • In trachea: air saturated with water vapour: PIO2 = FIO2 x (760 – PH2O) = 0.21 x (760 – 47) = 150 mm Hg Oxygen delivery system 1. Pulmonary ventilation: from atmosphere to alveoli • In alveoli: O2 partly absorbed by capillary blood and replaced with CO2 Alveolar gas equation: PAO2 PIO2 − [PACO2 / RQ] 100 mm Hg RQ • • = Respiratory quotient = rate of CO2 production (VCO2) / rate of O2 consumption (VO2) • • = VCO2 / VO2 0.8 Symbols P = partial pressure (mm Hg) atm = in atmospheric air I = in inspired air (humidified) E = in expired air A = in alveolar air c = in end pulmonary capillary a = in arterial blood v = in venous blood Oxygen delivery system 2. From alveoli to blood • In a perfect lung: PaO2 = PAO2 i. Ventilation-perfusion mismatch (50%): • • Low VA / Q ratio at the base of the lungs ii. Anatomic shunts (50%): Bronchial arteries to pulmonary veins (1% of cardiac output) Coronary venous blood (Thebesian veins) to left ventricle (<1% of cardiac output) iii. Diffusion block (normally small): Incomplete equilibrium through the respiratory membrane Definitions: • Physiological shunt: Ventilation-perfusion mismatch + anatomic shunts • Venous admixture: Mixing of oxygenated blood with unoxygenated blood Partial pressure (mm Hg) • In practice: PaO2 < PAO2 3 causes: Oxygen delivery system 2. From alveoli to blood Alveolar-arterial oxygen gradient (AaDO2): 5% shunt AaDO2 ≈ 10 mm Hg AaDO2 PaO2 PatmO2 Oxygen delivery system Alveolar-arterial oxygen gradient (AaDO2): • Difference between alveolar (PAO2) and arterial (PaO2) partial pressures of O2 AaDO2 = PAO2 – PaO2 • Normal A-a O2 gradient: 5-15 mm Hg • A-a O2 gradient increases with age Quick estimate: AaDO2 (age + 10) / 4 E.g.: AaDO2 10 mm Hg at age 30 • A-a O2 gradient increases with increasing FIO2 Quick estimate: about 5 to 7 mm Hg per 10% increase ( 6 mm Hg / 10%) Oxygen delivery system A-a O2 gradient increases with shunt AaDO2 Oxygen delivery system A-a O2 gradient increases with diffusion block 90% block Oxygen delivery system A-a O2 gradient increases with increasing FIO2 (FIO2 = Fraction of O2 in inspired dry air) FIO2 = 0.5 Oxygen delivery system 3. From blood to cells PatmO2 Oxygen delivery system CaO2 % Hb saturation (SO2) O2 content (mL/ dL blood) PvO2 PaO2 CvO2 Oxygen delivery system 3. From blood to cells O2 content (mL O2 / dL blood) C(a-v)O2 PatmO2 CaO2 CvO2 Oxygen delivery system 3. From blood to cells: Transport of oxygen O2 content (mL O2 /dL blood) = O2 bound to Hb + O2 dissolved O2 bound to Hb = O2 capacity of Hb x Hb content x % Hb saturation (mL O2 /g Hb) x (g Hb/dL blood) x % • In arterial blood: 1.34 x 15 x 97.5% = 19.6 mL O2 /dL blood • In mixed venous blood: 1.34 x 15 x 75% = 15.1 mL O2/dL blood O2 dissolved = Solubility of O2 x PO2 (mL O2 / dL blood • mm Hg) x (mm Hg) • In arterial blood: 0.003 x 100 = 0.3 mL O2 /dL blood • In mixed venous blood: 0.003 x 40 = 0.1 mL O2 /dL blood CaO2 = Arterial blood oxygen content = 19.6 + 0.3 20 mL O2 /dL blood CvO2 = Venous blood oxygen content = 15.1 + 0.1 15 mL O2 /dL blood O2 delivery (mL O2 / min): amount of oxygen delivered to the tissues per minute • DO2 = Cardiac Output x CaO2 = 5 L/min x 20 mL O2/dL x 10 dL/L = 1000 mL O2 / min A decrease of O2 delivery could be caused by a decrease in: 1) cardiac output, 2) Hb content, 3) % Hb saturation Oxygen delivery system 3. From blood to cells: Oxygen extraction C(a-v)O2 = (CaO2 – CvO2) = (20 – 15) = 5 mL O2/dL O2 extraction: fraction of O2 removed from the blood O2 extraction = (CaO2 – CvO2) / CaO2 = 5 / 20 = 0.25 O2 consumption (mL O2 / min): amount of oxygen consumed by the tissues per minute • VO2 = Cardiac Output x (CaO2 – CvO2) = 5 L/min x (5 mL O2/dL) x 10 dL/L = 250 mL O2 / min An increase in O2 consumption would lead to one or more of the following : 1) A decrease in CvO2 (i.e. an increase in O2 extraction) 2) An increase in cardiac output 3) An increase in CaO2 (long term adaptation) Oxygen delivery system Example 1. Cardiogenic shock A decrease in cardiac output increases C(a-v)O2 gradient, with little effect on CaO2 Cardiac Output O2 content (mL/dL blood) Oxygen delivery system Example 2. Anemia A decrease in Hb reduces CaO2 with little effect on C(a-v)O2 gradient O2 content (mL/dL blood) CaO2 CvO2 Mechanisms of hypoxia and hypoxemia • Hypoxia: Inadequate oxygen delivery to the tissues • Hypoxemia: Reduced PaO2 Mechanisms of hypoxia and hypoxemia • Hypoxemic hypoxia I. Oxygen deficit in inspired air (e.g. high altitude) II. Alveolar hypoventilation (e.g. neuromuscular disease) III. Ventilation/perfusion mismatch (e.g. severe asthma, COPD) IV. Problems with diffusion (e.g. interstitial lung disease) V. Right to left shunt (e.g. cyanotic congenital heart defects) Mechanisms of hypoxia and hypoxemia • Hypoxia without hypoxemia VI. Hypoxia of transport (anemia) (e.g. anemia, CO poisoning, MetHb) VII. Ischemic hypoxia (stagnant) circulatory shock (e.g. CV Collapse) VIII. Troubles with diffusion at the interstitial level (e.g. interstitial oedema) IX. Histotoxic hypoxia (e.g. cyanide poisoning) X. Cellular overuse of oxygen (e.g. muscular rigidity, fever, chills, intense exercise) Mechanisms of hypoxia and hypoxemia Hypoxia PaO2 AaDO2 CaO2 C(a-v)O2 A Low PIO2 (low inspired O2) Low N Low N B Hypoventilation Low N Low N C V/Q mismatch Low High Low N D Decreased diffusion Low High Low N E Cardiovascular (stagnant) N N N High F Anemia N N Low N G Histotoxic N N N Low Symbols PAO2 = partial pressure of O2 in alveolar air PaO2 = partial pressure of O2 in arterial blood AaDO2 = PAO2 – PaO2 CaO2 = total content of O2 in arterial blood CvO2 = total content of O2 in venous blood C(a-v)O2 = CaO2 - CvO2 Mechanisms of hypoxia and hypoxemia Condition PaO2 AaDO2 CaO2 C(a-v)O2 E Cardiogenic shock N N N High PAO2 = partial pressure of O2 in alveolar air C Severe asthma Low High Low N A High altitude Low N Low N PaO2 = partial pressure of O2 in arterial blood B Hypoventilation Low N Low N C Tetralogy of Fallot Low High Low N D Pulmonary fibrosis Low High Low N G CN- toxicity N N N Low F CO poisoning N N Low N Would hypoventilation and tetralogy of Fallot respond the same to O2 therapy? Symbols AaDO2 = PAO2 – PaO2 CaO2 = total content of O2 in arterial blood CvO2 = total content of O2 in venous blood C(a-v)O2 = CaO2 - CvO2 Hypoventilation (50% VT) and O2 therapy (FIO2 = 0.9) O2 O2 content (mL/dL blood) Shunt (50%) and O2 therapy (FIO2 = 0.9) O2 O2 content (mL/dL blood) Effects of methemoglobin and sulfhemoglobin on O2 delivery and content - Methemoglobin (metHb): Oxidation of the iron ions in hemoglobin. Oxidant Hb (Fe2+) metHb (Fe3+) metHb reductase (Treatment: methylene blue, a “redox dye”) - Sulfhemoglobin (sulfHb): addition of a sulfur following oxidation of the porphyrin ring in hemoglobin Hb + -S sulfHb (irreversible) • The affinity of Hb for O2 (left and right shifts) directly affects oxygen extraction by altering CvO2 affinity O2 extraction affinity O2 extraction Effects of methemoglobin and sulfhemoglobin on O2 delivery and content Properties of metHb: • Decreased O2 binding capacity (mimics anemia) • Increased affinity for O2 (left shift) May lead to severe decrease in O2 delivery and extraction Normal blood 60% metHb Anemia (40% of normal) Effects of methemoglobin and sulfhemoglobin on O2 delivery and content Properties of sulfHb: • Decreased O2 binding capacity (mimics anemia) • Decreased affinity for O2 (right shift) Effects much less severe than metHb Normal blood 60% metHb Anemia (40% of normal) 60% sulfHb Clinical and laboratory assessment of cyanosis, hypoxemia and tissue hypoxia. Main laboratory assessments: • Pulse oximetry • Measures Hb saturation (not PaO2) • Inaccurate in the presence of abnormal Hb or dyshemoglobins (carboxyHb, metHb, sulfHb) • Arterial blood gases: • Measures of PaO2, PaCO2, pH • From calculation, allow estimates of AaDO2 , CaO2 (with Hb measurement) CBC News 08/06/2007 [SHb]: 2g/L Drug used: Sumatriptan (a sulfonamide) Clinical and laboratory assessment of cyanosis, hypoxemia and tissue hypoxia. Main clinical assessments of cyanosis: Cyanosis: blue coloration of the skin as a result of poor saturation of hemoglobin (detectable with deoxyhemoglobin > 40 g/L) Assessment: Cyanosis Yes • Respiratory disease • Heart failure Response to O2 No Continued cyanosis • Pulmonary shunt (ARDS) • Cyanotic heart defect (newborn) Low • Exposure to oxidants (drugs, nitrates) • Severe acidosis • Hereditary defects Yes PaO2 High metHb level high, response to methylene blue No • SulfHb • Methylene blue overdose