- Organ Donation Alliance
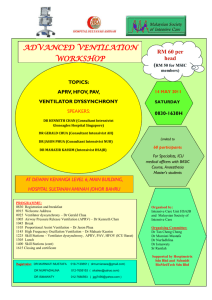
advertisement

Donation Service Area Best Practice Workgroup OPO Toolbox Contents Survey Readiness Survey readiness is very important for OPOs because if observations or citations are found, it can be detrimental to the OPOs operations. Summary of Task Force Recommendations & Findings Preparation is key. In addition to preparing before a survey, an OPO should also prepare yearround. Subjectivity of surveyors is a difficult caveat to resolve. Best Practices Conducting a mock inspection by external peers. Leadership team involvement in their areas of policy review and use of SharePoint for tasks and accountability. Monthly Quality Council Meeting where a report always includes standards and regulatory changes. Scheduled time in weekly leadership meetings to include work sessions related to the audit preparations and to go over each standard by department. Creation of accountability logs and review at each meeting. Audit checklist for our administrative staff to help keep on track with all that needs done in preparation for the site visit, including meals. Safety & environmental rounds conducted prior to the scheduled audit. Preparation of a question/answer key for staff and Medical Director of commonly asked questions by previous auditors. Adding all previous citations to the quality audit schedule to ensure no citation is ever repeated. Caveats & Lessons Learned Using AOPO Prep questions with staff is still not successful. It would be useful to find a better method to prep staff for questions. Surveyors are subjective in that they have subject matter expertise and do not always focus on all subjects uniformly. Not all surveyors are consistent in their strictness of regulations. Regulations allow for interpretation by each surveyor. Donation Service Area Best Practice Workgroup OPO Toolbox Contents Quality Improvement Summary of Task Force Recommendations & Findings It is important to have a detailed Dashboard and hold monthly Quality Council meetings to review the status of goals and objectives within that Dashboard. Maintaining data, reports, summaries, and communicating this data with the hospitals is essential to improving quality in hospital relations. Best Practices (attached) Use of detailed Dashboards that are reviewed on a monthly basis. These Dashboards must include measurable objectives that can be trickled down to each department and employee. Use of Quarterly DSA Action Team Data: This is the PBD and Lost Organ Potential data used for the DSA Action Team to demonstrate opportunities for improvement and leverage change. This is focus data for PDSA activity. Use of Service Area Schema for Hospital Classification: This is our annual hospital classification toll that ranks hospital for service based on potential for donation and services available. Use of Hospital Development Plan: This is a plan that identifies CMS required components to optimize improvement in hospital donation programs. Use of Comprehensive Summary of Opportunities Reports: These are the summary report provided to hospital after completion of the death record review that identifies areas for improvement and impact on year to date data outcomes. Use of Timely Referral Tracking Summaries: For both our DSA and Community of Practice Hospitals these are internal tools of summarization of record review results used to report to quality council as guide for improvement activities. This data is also tracked on dashboards for Board of Directors awareness. Use of Hospital Timely Referral Tools: This is the referral summary tool that is a part of each CRS and can be used where needed in a hospital to evidence current status of referral program. Use of End of Month Letters: This is a copy of the monthly letter we send to all hospital CEO’s and Liaisons with year to date conversion and potential donor data and the number and type of educational activity done in the hospitals. Supporting Materials Attachment A: AOPO Quarterly Data Snapshot – CORE Attachment B: 2009 CORE Dashboard Attachment C: Quality Hospital Development – 4th Quarter DSA Action Team Data Attachment D: Quality Hospital Development – CORE Service Area Scheme for Hospital Classification 2011 Attachment E: Quality Hospital Development – CORE Hospital Development Plan Attachment F: Quality Hospital Development – Comprehensive Summary of Opportunities – Death Record and Referral Review – Memorial Medical Center Attachment G: Quality Hospital Development – Comprehensive Summary of Opportunities – Death Record and Referral Review – Allegheny General Attachment H: Quality Hospital Development – 2011 Timely Referral Tracking Summary Attachment I: Quality Hospital Development – Timely Referral Tool Attachment J: Quality Hospital Development – End of Month Letter Donation Service Area Best Practice Workgroup OPO Toolbox Contents Intensivist The goal of an Intensivist program is to increase organ donors at that particular hospital where an Intensivist is located. The objective is to increase transplants by increasing organ yield (Organs Transplanted per Donor). CORE’s program was implemented in July of 2008 at UPMC Presbyterian with Dr. Joe Darby as the Physician Director. Components of an Intensivist model include: On site CCM evaluation and management of every potential organ donor at UPMC Presbyterian; Consult CCM after consent or authorization from CORE Administrator on Call; Participate in process improvements and physician relations; If successful, evaluate as a spread model to other hospitals; And evaluate data in six months. Summary of Task Force Recommendations & Findings Support from the OPO Leadership, Hospital, and team is key to the success of the program. Implementation If implementing an Intensivist program, please refer to the supporting materials that includes responsibilities, various order set forms, and a feedback form. Briefly, an Intensivist’s responsibilities include: Provide call schedule to our call center Provide 24/7 coverage to the procurement staff regardless of donor hospital location (phone consult) Submit invoice for monthly services Pronounce on DCD cases Best Practices Utilized the program at our largest donor hospital. Need to have a donor hospital physician who believes in the process and takes action/accountability (Can’t initiate without). Need an OPO CEO who understands the donation process and supports the program financially. Need a dedicated group of CCM physicians who are on the team. The team should provide a monthly call schedule to OPO. The ODST should submit an invoice at the end of month. The ODST should submit a form for data collection. The procurement coordinator then should fill out a form and the ODST physician should submit it in electronic form as well. Data collection between the hospital and OPO is critical to drive the project. Celebrate your successes by dinner and luncheons with teams. It is believed that our process works great due to the support of Dr. Darby, Dr. Simmons and UPMC. Caveats & Lessons Learned We tried using a phone consult on all donors with group of 3 trauma physicians at a regional hospital with no change in yield. Thus, we changed the process to on-site consult which showed increase in yield. OPO staff at first did not support the ODST, but the program gained support after working with the team. We have tried this same process at AGH and CAMC without much success. Failure attributed to lack of support of donor hospital and inability to identify physician champion. Donation Service Area Best Practice Workgroup OPO Toolbox Contents Supporting Materials Attachment K: Intensivist Implementation Responsibilities Attachment L: Intensivist Implementation – Brain Death Order Set Attachment M: Intensivist Implementation – Brain Dead Organ Donor Order Set Attachment N: Intensivist Implementation – Physician Order Set Brain Death Attachment O: Intensivist Implementation – ICU Diabetes Insipidus Management Order Set Attachment P: Intensivist Implementation – ODST Feedback Form Attachment Q: Intensivist Implementation – Brain Injury Guidelines Attachment R: Intensivist Implementation – Kansas Pediatric Consult Form Attachment S: Intensivist Implementation – Kansas Donor Management Guidelines Attachment T: Intensivist Implementation – Kansas CC Consult Form Attachment U: Intensivist Implementation – Kansas CC Consult Form Organ Donor Management Attachment V: Intensivist Implementation – Kansas Policies