insulin delivery system presentation
advertisement

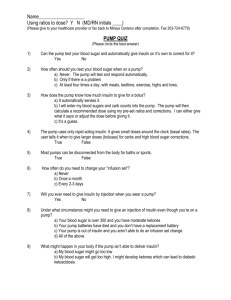
Insulin Pump Therapy Gary Scheiner MS, CDE Integrated Diabetes Services 333 E. Lancaster Ave., Suite 204 Wynnewood, PA 19096 (877) 735-3648 Gary@integrateddiabetes.com www.integrateddiabetes.com 101 Insulin Pump Therapy 101 How Pumps Work Pros & Cons Strategies for Success Q & A What A Pump IS Beeper-sized, battery-operated. A way of giving insulin. Worn externally. Programmable for individual needs. Pump Evolution 1970s Pump Evolution 1970s Pump Evolution 1970s 1980s Pump Evolution Modern Day Insulin Pumps Insulin Used In Pumps Rapid-Acting Analogs are Preferred Aspart (Novolog) Lispro (Humalog Glulisine (Apidra) Modes of Delivery Basal Bolus Basal Insulin Steady “Drip” of Insulin Matches Glucose Released by Liver Meets Body’s Basic Energy Needs May Need Different Settings at Different Times of Day 12:00 AM 9:00 PM 6:00 PM 3:00 PM 12:00 PM 9:00 AM 6:00 AM 3:00 AM 12:00 AM Units per hour 2 1.8 1.6 1.4 1.2 1 0.8 0.6 0.4 0.2 0 12:00 AM 11:00 PM 10:00 PM 9:00 PM 8:00 PM 7:00 PM 6:00 PM 5:00 PM 4:00 PM 3:00 PM 2:00 PM 1:00 PM 12:00 PM 11:00 AM 10:00 AM 9:00 AM 8:00 AM 7:00 AM 6:00 AM 5:00 AM 4:00 AM 3:00 AM 2:00 AM 1:00 AM 12:00 AM Bolus Insulin Given to “cover” carbs in meals and snacks. Used to “correct” high blood glucose levels Insulin Infusion (aka “getting under your skin”) Durable, clog-resistant tubing carries insulin from the pump to the infusion set*. The infusion set delivers insulin into the fatty layer below the skin. Set uses either a flexible plastic catheter (canula) or a steel needle. Almost always disconnectable near the infusion site. * OmniPod does not have tubing; it attaches directly to the skin. Infusion Set Types Infusion sets vary by: Angle of insertion Canula length Plastic vs. steel Tubing length Infusion Set Insertion Soft plastic canula inserted by way of an introducer needle. Mechanical “inserters” are available for some types of insusion sets. Clinical Advantages of Pump Therapy Reduction in HbA1c1 Less BG Variability2 Reduction in duration, frequency and severity of hypoglycemia3 Better psychosocial outcomes & quality of life4 Clinical Advantages of Pump Therapy 1 Bode et al; Diabetes Care 1996; 19:324-7 Weinzimmer et al; Pediatrics 2004; 114: 1601-5 5 Nations Trial; Diabetologia 2004; 47 (1): #82 DeVries et al; Diabetes Care 2002; 25:2074-80 2 DeVries et al. Diabetes Care. 2002 Nov; 25(11):2074–80 Diabetes Nutr Metab. 2004 Apr;17(2):84-9 N. Weintraub et al: Arch Pediatr Adolesc Med. 158: 677-684, 2004 3 Hissa et al; Endocrine Practice 2002: 8; 411-416 DeVries et al. Diabetes Care. 2002 Nov; 25(11):2074–80. Rudolph and Hirsh; Endocrine Practice 2002: 8; 401-405 Siegel et al; Diabetes Care 2004; 27: 3022-3. 5 Nations Trial; Diabetologia 2004; 47 (1): #82 4 Peyrot and Rubin; Diabetes Care 2005; 28: 53-58 McMahon et al; DiabeticMedicine 2005; 22:92-96 Bruttomesso et al 2002; 19:628-634 Shapiro, 1984; Skyler, 1982 References Practical Benefits: Pump Basal Aspects NPH (nighttime only) Avg. Basal Needs 12am 3am 6am 9am 12pm 3pm 6pm 9pm 12am 6pm 9pm 12am 6pm 9pm 12am NPH (morning and night) 12am 3am 6am 9am 12pm 3pm 6pm 9pm 12am Pump Basal Delivery 12am 3am 6am 9am 12pm 3pm Lantus or Levemir 12am 3am 6am 9am 12pm 3pm 6pm 9pm 12am 12am 3am 6am 9am 12pm 3pm Practical Benefits: Pump Basal Aspects Avg. Basal Needs NPH (nighttime only) Potential Problems: 12am 3am 6am 9am 12pm 3pm 6pm 9pm 12am Too much in middle of the night? Too little late in the day? General Inconsistency Practical Benefits: Pump Basal Aspects Potential Problems: Basal and Needs NPHAvg. (morning night) Too much in middle of the night? 12am 3am 6am 9am 12pm 3pm 6pm 9pm 12am Midday peak requires consistent mealtimes Poor coverage of post-lunch peak General Inconsistency Practical Benefits: Pump Basal Aspects Avg. Basal Needs Lantus or Levemir Potential Problems: 12am 3am 6am 9am 12pm 3pm 6pm 9pm 12am Failure to offset dawn phenomenon Too much in middle of the day? 1 shot May not last full 24 hrs Practical Benefits: Pump Basal Aspects Pump Avg. Basal Basal Delivery Needs Basal insulin can be matched to the body’s daily needs. 12am 3am 6am 9am 12pm 3pm 6pm 9pm 12am Practical Benefits of Pump Basal Delivery: Stable BG between meals & overnight Can skip/delay meals without dropping Can vary sleep & work schedules Fewer issues with travel/time zone changes Can correct for dawn effect No long-acting insulins (more consistent insulin action) Immediate, temporary basal adjustments possible Practical Benefits of Bolusing with a Pump Can dose very precisely (.1 or .05 units) Convenient to give insulin anytime, anywhere “Unused Insulin” adjustment prevents stacking of boluses Rate of delivery can be extended Insulin delivery history stored in pump One needle stick every 3 days (approx) Built-in bolus calculator Bolus Calculator: Example Estimate Details Est total: Food intake: BG: 7.0 U 60 gr 6.0 U Correction: 2.0 U Active ins: 1.0 U ESC to back up ICR 1:10 gram 200 (11.1) Food: ACT to proceed Automatically calculates insulin bolus requirement for the patient 200 (11.1) – 100 5.5 = 2.0 units 50 (2.8) Active insulin is subtracted from the correction What A Pump Is NOT A cure for diabetes. A substitute for blood glucose monitoring & carb counting. As effective as a healthy pancreas. Potential Drawbacks to Pump Therapy Cost Learning Curve Extra Testing Risk of Ketosis & DKA Weight Gain Potential Skin Irritation Inconvenience Time/Discomfort of Set Changes Teaching & Follow-Up Required What Makes A Good Pump Candidate? Responsible Pre-Pregnancy Irregular Schedule Endurance Athletes Existing Complications Difficulty w/BG Control Frequent or Severe Lows Insulin-Dependent (1 or 2) Hypoglycemic Unawareness Sensitivity to Small Insulin Doses Possess Proper Self-Management Skills Adequate Insurance or Financial Resources Strategies for Success: Pre-Pump Education BG monitoring 4+ times/day Detailed Record Keeping Carbohydrate Gram Counting Self-Adjustment of Insulin Principles of Basal/Bolus Therapy Strategies for Success: Post-Pump Management Frequent communication w/health care team Basal Testing Bolus/Correction dose fine-tuning Activity adjustments Application of advanced pump features Persistent self-care (don’t miss boluses!) Effective troubleshooting, prevention of DKA Strategies for Success: DKA Prevention Unexplained High Blood Sugar Check for Ketones Ketones Negative Bolus w/Pump BS Drops O.K. Ketones Positive BS Doesn’t Drop 1. Shot w/Syringe 2. Drink Water 3. Change Out Pump Strategies for Success: Pump Selection Criteria Insulin Reservoir Volume Screen Readability Bolus Maximums & Increments Bolus Calculator Flexibilty Alarm Distinction Water-Tightness Strategies for Success: Pump Selection Criteria Link w/Meter or CGM Convenience Factors (tubing, clip) Infusion Set Options Aesthetics Out-Of-Pocket Costs Strategies for Success: Infusion Set Selection/Use Appropriate Correct Site depth for body type priming amount preparation technique Frequency Proper of change-outs 3 days site rotation Think Like A Pancreas!