Pediatrics Review 2015 - Emergency Medicine National Review
advertisement

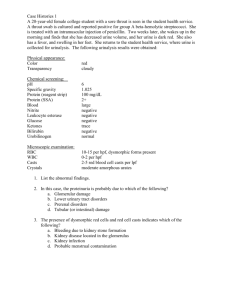
Pediatrics Review 2015 Dr. Andrea Boone, MD, FRCPC Alberta Children’s Hospital Foothills Medical Centre University of Calgary Disclosures I have no financial disclosures or academic conflicts. Objectives Pediatric emergenices…in 50 minutes! Review key pediatric emergencies – from neonates to adolescents Evidence base reviews of select emergencies Fever: Neonate (0-28 days) Full septic work up: CBC + diff, Blood culture, Urine culture, lumbar puncture Empiric antibiotics: Ampicillin/cefotaxime or Ampicillin/Gentamicin To cover typical bugs causing neonatal sepsis: Group B Strep E. Coli Listeria monocytogenes Chlamydia trachomatis N. gonorrhea Add acyclovir Herpetic skin lesions Seizure Maternal history genital HSV Abnormal LFTs Fever: Infant (29-90 days) Philadelphia Rochester Boston Age 29-60d <60days 28-89d Temp >38.2C >38C >38C History Not specified Term infant No perinatal Abx No underlying disease Not hospitalized longer than the mother No immunizations < 48h No antimicrobial < 48h Not dehydrated Physical Exam Well-appearing Unremarkable exam Well-appearing No ear, soft tissue or bone infection Well-appearing No ear, soft tissue, or bone infection Labs (define Lower risk) WBC<15,000 Band-neutrophil ratio<0.2 UA <10 WBC/hpf Urine gm stain: negative CSF<8 wbc/hpf CSF gm stain: negative CXR: no infiltrate Stool: no RBC, no WBC WBC 5,000-15,000 Absolute band <1500/mm3 UA<10 WBC/hpf Stool smear <5WBC/hpf WBC <20,000 CSF<10/mm3 UA<10wbc/hpf CSF < 10 WBC/hpf CXR: no infiltrate Fever: Infant (29-90 days) Designed to detect low risk patients that could be managed as outpatients Boston criticized for higher WBC cut off resulting in high rate of SBI (~5%) in patients identified as low risk; requires empiric antibiotics Philadelphia requires LP, but no empiric antibiotics Rochester criteria, no LP, no empiric antibiotics, rate of SBI in low risk infants < 1 % Fever: Infant (29-90 days) Approach – partial septic work-up: Well appearing, >37 wks, no identifiable soft tissue infection/source, not hospitalized longer than mom Low risk infants: WBC: 5000-15000, < 1500 bands Urine cath R&M: WBC < 10 /hpf Stool analysis, only if diarrhea: < 5 /hpf Discharge with 24 hour follow up pending cultures. No empiric antibiotics. If plan for empiric antibiotics (ceftriaxone 50 mg/kg), do LP. UTIs in Children > 2 months Check urine in 2-36 months with unexplained fever Urine collection: Not toilet trained, < 2 y/o Urine cath or suprapubic aspirate for U/A, C&S Bag specimen – screen only. If positive, need cath for C&S (not exam answer….do cath on exam) Toilet trained Mid stream/clean catch urine for R/M, C&S Risk factors for UTI: Uncircumcised male < 12 mo, circumcised < 6 mo GU abnormalities Female < 24 months, fever > 39 C without focus UTIs in Children > 2 months Management: Antibiotics geared towards local susceptibility patterns and usual bugs E. Coli, Klebsiella, Serratia, Enterbacter, Citrobacter Common PO choices cefixime, septra, clavulin vs IV for uncomplicated febrile UTI > 2 months PO acceptable provided HD stable, not toxic, tolerating po, normal GU anatomy, with close follow up available UTIs in Children > 2 months Indications for ED Imaging: Not clinically improving within 48 hours: Renal Bladder US (RBUS) for ?abscess ?hydronephrosis to suggest obstruction/high grade VUR Indications for f/u imaging with family MD: 1st episode febrile UTI – RBUS indicated 2nd episode febrile UTI - VCUG indicated Case 2 yr old boy wakes up at 3 AM with difficulty breathing URTI sxs for 3 days. Hoarse voice and barky cough. T 39, RR 48, HR 140, O2 sat 95% Moderate distress. Stridor at rest. Indrawing. Management? Differential diagnosis? Croup Parainfluenza most common RSV, influenza, adenovirus Hoarse voice, barky cough, stridor Young children, Peak fall and spring Neck soft tissue xray if atypical, severe, not improving Dexamethasone (0.6 mg/kg) for all, effect by 6 hrs Nebulized Epinephrine effect by 30 min Consider Nebulized Budesonide 2 mg if severe Difficult airway!!! Croup: Westley Croup Score Mild 0-3, Moderate 47, Severe >8 Respiratory failure if >12 Mild (0-2) No stridor No to minimal indrawing Moderate (3-5) Stridor/indrawing at rest No distress/agitation Severe (6-11) Stridor/indrawing at rest Agitation/distressed Resp. failure > 12 Lethargy/cyanotic Retropharyngeal Abscess Complication of Pharyngitis, Head & Neck infections, Penetrating trauma Grp A strep, oral anaerobes and S. aureus < 6 yrs Retropharnygeal lymph nodes regress Stridor, sore throat, muffled voice Neck pain and stiffness Fever, unwell appearance Retropharyngeal Soft Tissues * Age (yrs) Maximum (mm) 0-1 1.5 x C2 1-3 0.5 x C2 3-6 0.4 x C2 6-14 0.3 x C2 * Retrotracheal Soft Tissues * Age (yrs) Maximum (mm) 0-1 2.0 x C5 1-2 1.5 x C5 2-3 1.2 x C5 3-6 1.2 x C5 6-14 1.2 x C5 * Retropharyngeal Abscess Complications Airway compromise Erosion into carotid artery Aspiration pneumonia Mediastinitis Lateral pharyngeal space rupture Extension into spine IV Ceftriaxone and Clindamycin Consult ENT Consider CT Epiglottitis Involves all supraglottic tissues GAS, Strep pneumoniae H.influenza rare Rapid onset of severe sore throat, stridor, drooling, sniffing/tripod position Do not disturb patient Consult Anesthesia, ENT- Intubate in OR IV Ceftriaxone and Clindamycin Bacterial Tracheitis Toxic, unwell appearing Severe Croup sxs – non responsive to treatment Mortality 4% Staphylococcus aureus Also S. pneumo, H.influenza, M.catarrhalis, C.diphtheriae ICU admission Consult anesthesia if need intubation IV Ceftriaxone and Clindamycin (or Clox, or Vanco) Foreign Body Aspiration Highest risk between 1 -3 yrs old Immature dentition, poor food control More common with food than toys peanuts, grapes, hard candies, sliced hot dogs Acute respiratory distress (resolved or ongoing) Witnessed choking Cough, Stridor, Wheeze, Drooling Uncommonly…. Cyanosis and resp arrest Inspiratory Expiratory Respiratory Emergencies - Bronchiolitis Bronchiolitis < 2 y/o, most common < 12 y/o “first episode wheeze”, clinically variable presentation, viral URTI to severe LRTI Typically coryza, cough, variable WOB with crackles/wheeze on exam RSV most common cause human metapneumovirus, influenza, parainfluenza, adenovirus Higher risk – preterm < 35 wks, < 2 months of age, Congenital heart disease, immunodeficiency Respiratory Emergencies - Bronchiolitis Investigations: Routine labs not helpful, including NP swab CXR not helpful, misleading, leads to inappropriate antibiotics Fever + bronchiolitis Neonate – full septic work up, rate of SBI still high 1-3 months – rate of UTI 5%, do urine cath C&W; rate of bacteremia <1%; meningitis rare VBG/ABG – only in impending respiratory failure Respiratory Emergencies - Bronchiolitis Management: Supportive care is the mainstay Epinephrine – short term response, may trial Nasal suctioning – superficial/frequent; short term response Salbutamol – not recommended Hypertonic saline nebs – not recommended; some evidence to support use in inpatient, need to give with epi as bronchoconstrictor Epi + dexamethasone (Plint et al. NEJM 2009) CanBest – one study, approached significance in reduction in admissions, controversy re large steroid doses; not routinely recommended Respiratory Emergencies - Bronchiolitis Indications for admission: Persistent sats < 90% room air Dehydration requiring NG/IV fluids Significant WOB High risk infants History of apnea at home or in department Family not coping Pertussis Most commonly < 6 months 3 clinical stages: Catarrhal – mild URTI symptoms, 1-2 weeks Paroxysmal – staccoto cough, post-tussive emesis, apnea, classic whoop often absent < 3 y/o; 2-4 wks Convalescent – gradual resolution Diagnosis – clinical, suspect if prolonged cough contact, NP swab for C&S, PCR; CXR often normal Management admit if < young age, apnea, increased WOB Erythomycin to reduce spread of infection Congestive Heart Failure Left to Right shunts Presentation at 1 month Decreasing pulmonary vascular resistance 1st month of life Symptoms Increased blood flow into lungs Irritability, Diaphoresis Poor feeding (early fatigue), Failure to thrive Signs Tachypnea, Tachycardia, Respiratory distress Enlarged liver Gallop/murmur Congestive Heart Failure VSD most common Other: ASD, PDA Diagnosis Pansystolic Murmur, Hyperactive precordium ECG – LVH CXR – cardiomegaly, vascular redistribution ED Management ABC’s, Glucose Furosemide 1mg/kg CPAP Congenital Heart Disease - Age of presentation Cardiac Emergencies: A Case EMS call enroute with blue baby, 6 wk male On arrival ++crying, RR 60 Sats 55% on 100% NRBM, HR 180, BP 72/48, T 37.2 R glucose 5.1 CR 4 sec, mottled Clear lungs. Single S2. + systolic murmur No hepatomeglay. Benign abdo Further history – term baby, poor feeding since birth, poor weight gain, known murmur Cardiac Emergencies: A Case Tetralogy of Fallot Right ventricular outflow tract obstruction (RVOTO) Right ventricular hypertrophy(RVH) Overriding aorta Ventricular septal defect (VSD) Cardiac Emergencies: Tet Spell Pathophysiology: Worsening right to left shunt secondary to sudden decrease in SVR Metabolic acidosis increases hyperpnea/preload Precipitants: Crying, exercise (feeding), tachycardia, defecation, hypovolemia Management principles: Increase SVR, abort hyperpnea, correct hypoxia, correct acidosis Cardiac Emergencies: Tet Spell Management: 100% Oxygen - pulmonary vasodilation Knees to chest/squat – increases SVR Soothe child – stops crying/hyperpnea cycle/drops venous return Fluid bolus 10-20 cc/kg – improve RV filling Morphine 0.1 mg/kg IV – anxiolysis Propranolol 0.1 mg/kg IV – reduces RVOTO spasm Refractory cases – HCO3/ketamine/phenylephrine Case 2 yr old boy with fever for 6 days. Red eyes but no discharge. Generalized rash. Erythema of the palms of hands and soles of feet. Red, swollen lips. Enlarged cervical lymph nodes. Diagnosis? Complications? Kawasaki Disease Usually < 4 yrs old peak 1-2 yrs Fever for >/= 5 days and 4 of: Bilateral non-purulent conjunctivitis Rash Changes of peripheral extremities • • Initial stage: reddened palms and soles, edema Convalescent stage: desquamation of fingertips and toes Changes of lips and oral cavity Cervical lymphadenopathy ( >1.5 cm) Kawasaki Disease Subacute phase - Days 11-21 Desquamation of extremities Arthritis Convalescent phase - > Day 21 If untreated ~ 25% coronary artery aneurysms Other manifestations: Uveitis, Pericarditis, Myocarditis Hepatitis, Gallbladder hydrops Aseptic meningitis Incomplete Kawasaki’s Disease Incomplete (Atypical) 5 d fever 2 -3 criteria AAP Kawasaki statement Newburger et al. Pediatrics, 2004 Kawasaki Disease Supplemental Lab Criteria ESR >40 CRP >3 WBC > 15 000/mm Anemia Platelets after 7 days > 450 Elevation of ALT Albumin < 3 Urine >10 WBC/hpf Kawasaki Disease Treatment IV Immunoglobulin (2 g/kg) Reduces coronary aneurysms to 3% if given within 10 days of onset of illness Defervescence with 48 hrs ASA During acute phase high dose (80-100 mg/kg/day) then low dose (3-5 mg/kg/day) for 6-8 weeks Stop if normal ECHO Neonatal Jaundice Most common neonatal presentation in 1st week of life Unconjugated vs conjugated Acute bilirubin encephalopathy Early: High pitched cry, lethargy, hypotonia Late: Hypertonia, seizures, coma, death Chronic bilirubin encephalopathy Athetoid cerebral palsy, seizure d/o, deafness HYPERBILIRUBINEMIA Conjugated Hemolysis Immune Blood group •ABO •Rh •minor Enzyme •G6PD •Pyruvate kinase Non-immune Membrane •HS •Poikilocytosis •Elliptocytosis Non-hemolytic •Breast feeding associated •Breast milk •Sepsis •Hypothyroid •Bruising/cephalohematoma •Polycythemia •Hypoxia/Acidosis •Intestinal obstruction •Gilbert syndrome •Lucey Driscoll •Crigler Najjar (I, II) Neonatal Jaundice Key components of assessment: Septic risk factors? PPROM, Septic GBS +, intrapartum fever, prior neonate with GBS behaviour? Poor feeding, irritability, lethargy, vomiting, colour change, difficulty breathing, decreased urine output Unwell appearing neonate? Pallor, mottling, irritability, lethargy, high pitched cry, abnormal vital signs, weight loss > 10% of birth weight Neonatal Jaundice Investigations: Total serum bilirubin (TSB) + direct (conjugated) bilirubin CBC, Blood group, DAT (direct antibody test=Coombs test) Consider: Septic work up – blood culture, urine culture, lytes, creat, VBG ~8% of jaundice requiring treatment have UTIs (even in absence of symptoms/signs of infection) – so check urine if meet treatment threshold Neonatal Jaundice Risk Factors: • • • • • • • • Isoimmune hemolysis G6PD Asphyxia Resp distress Lethargy Temp instability Sepsis Acidosis Neonatal Jaundice Management: Start intensive phototherapy Consider IV fluids Keep baby warm Consider IV antibiotics if concerning for sepsis Check exchange transfusion chart! Case 3 week old boy vomiting every feed for 24 hours. Vomit is yellow/green. No diarrhea. Dry diaper since this morning. HR 180, RR 40, T 37.2 R. Irritable and restless. Eyes sunken. Mouth dry. Cap refill 5 sec. Abd distended and diffusely tender. What is your approach to this infant? Differential diagnosis? Volvulus Malrotation with midgut volvulus Short small bowel mesentery, ligament of Treitz poorly fixed Twisting of the bowel around the superior mesenteric artery Sudden onset of bilious vomiting, usually 1st month of life Acute abdomen with shock Bowel ischemia and necrosis, GI bleeding ABC’s, Fluid resuscitation, Glucose, NG tube Plain AXR – cannot rule out Upper GI series – definitive test Emergent surgery Pyloric Stenosis 4-6 weeks of age Male to female 4:1, first born males 5% of siblings and 25% if mother was affected Symptoms of gastric outlet obstruction Non-bilious vomiting Emesis increases in frequency and eventually becomes projectile Peristaltic wave, palpable mass in epigastrium “olive” Labs – hypochloremic hypokalemic metabolic alkalosis Ultrasound Rehydration, correction of metabolics prior to surgery Case 1 yr boy with vomiting and diarrhea since last night. This morning he had three loose stools with blood. He cries intermittently in cycles of 10 to 20 minutes. T36.5, HR 118, RR 40, BP 100/50. Pale and lethargic. Abd soft, mild tenderness. Mass palpable in RLQ. Investigations? Diff Dx? Intussusception Usually invagination of ileum into cecum (75%) 6 months to 3 yrs Males to female 3:2 90% are idiopathic Post viral illness – hypertrophy of Peyer patches Pathologic causes - Meckel diverticulum, polyps, hematoma (Henoch-Schonlein Purpura), lymphoma/leukemia, cystic fibrosis Intussusception Classic triad present in 10-30% Intermittent, crampy abdominal pain Vomiting “Currant jelly" stools Late sign, indicates intestinal edema and mucosal bleeding Lethargy in 25% Ultrasound (Sens 97-100%, Spec 88-100%) AXR (Sens 45%, Spec 21%) Lack of air in RLQ, obstruction Target sign, Crescent sign Intussusception Plain AXR: Paucity of air in RLQ Absent liver edge Obstruction Target sign RUQ mass, sometimes looks like a target Crescent sign Intussceptum lead point protruding into gas filled pocket Management: Air Contrast Enema • • Recurrence rate 10-15% • • Success rate 95% Bowel perforation in 1-3% 50% within first 24 hrs Other 50% within 10 mos Admit for observation Case 4 yr old with bruising to both legs today Pain with walking, swollen ankles. Abdominal pain with blood in stool. Diagnosis? Complications? Henoch-Schonlein Purpura IGA mediated vasculitis 2-11 yrs Rash 100% Arthritis 70% Ankles > knees >wrists > elbows Abdominal pain 50% Palpable petechiae/purpura, can be urticarial, buttock/leg Intussusception 2% Nephritis 40% (ESRD in ~1%) Henoch-Schonlein Purpura Investigations CBC, PT PTT, Lytes, BUN, CR; Urinalysis Prot, Alb, Immunoglobulins Strep testing – Throat swab, ASOT Weekly U/A and BP until sxs resolve then monthly for 6 mos Treatment NSAID’s for pain relief Consider steroids for abdominal, testicular, CNS involvement Controversial for renal complications Nephrology consult if hypertension, nephrotic sx’s Case 4 yr old with 2 week history of polyuria and polydipsia Very sleepy today. Complaining of headache. Normal vital signs. Tired but arousable. Dry MM. Eyes sunken. Normal cap refill. Blood sugar at triage “HIGH” Initial Management? Diabetic Ketoacidosis DKA Diagnostic criteria: pH<7.30 and/or HCO3<15 mmol/L random serum glucose > 11.1 mmol/L + urine ketones Symptoms Polyuria/Polydipsia, Wt loss Abdominal pain, Fatigue Signs Kussmaul respirations Ketotic breath “Look dry”; usually mild-mod dehydration CNS changes – headache, confusion, irritability, lethargy Diabetic Ketoacidosis Cerebral edema in 0.7-3.0% Patient risk factors Age < 2 years New onset DM, Longer duration of Sx More severe dehydration – high urea, K+, hct Greater acidosis - Low initial pC02, pH < 7.1 Treatment risk factors Rapid administration of hypotonic fluids IV bolus of insulin Early insulin infusion Failure of serum Na to rise during treatment Use of NaHCO3 Wolfsdorf J et al. Pediatric Diabetes 2014 Diabetic Ketoacidosis Fluid bolus only if hypotensive 10 ml/kg over 30-60 min Calculate fluids based on 10% dehydration replaced over 48 hrs; do not exceed 2x maintenance NS + 40 meq KCl/L (if voiding and K<5) Diabetic Ketoacidosis Start Insulin infusion 1-2 hrs after IV fluids Insulin 0.05 – 0.1 units/kg/hr No Insulin bolus No Bicarbonate Monitor hourly VS, neurovitals, glucose Gas, lytes, osm, urine ketones q2-4h Diabetic Ketoacidosis Cerebral Edema For headache alone Raise head of the bed to 30o Decrease fluids to maintenance If altered LOC (GCS<10) 3% Saline 5 cc/kg over 20 min OR Mannitol 0.5 gm/kg iv over 20 min Prepare for intubation STAT CT scan Febrile Seizure Simple Febrile Seizure T>38.5 6 mo-5 yr Generalized seizure, < 15 min One seizure within 24 hours Neurologically normal before and after Occur in ~ 5% of children Recurrence in 30% Management – as per fever management. Febrile Seizure Risk of epilepsy is 1% Epilepsy in general population 1% Higher risk (2.4%) if: Complex febrile seizures 2 or more in 24 hr Prolonged > 15 min focal < 12 mos at the time of first febrile seizure Family history of epilepsy Seizure Management ABC’s, Check Glucose Extended lytes Anticonvulsant levels Phenytoin, Phenobarbitol, Valproic acid, Carbamazepine Anion gap, Osm gap, ASA, Acet, Toxic alcohols Septic work up? Imaging? Consider ingestion 1st line - Benzodiazepines 2nd line – Fosphenytoin or phenytoin, Phenobarb 3rd line - Midazolam infusion Other – Thiopental, Pentobarbitol, Paraldehyde, Propofol, Valproic acid, Topiramate, Levetiracetam Status Epilepticus CPS Guidelines Paediatr Child Health 2011;16(2):91-7 Minor Head Injury: CATCH CATCH - Canadian Assessment of Tomography for Childhood Head Injury Inclusion criteria Witnessed loss of consciousness or disorientation Definite amnesia Persistent vomiting (two or more distinct episodes of vomiting 15 minutes apart) Persistent irritability in the ED if < 2 yrs GCS > 13 in the ED Injury within the past 24 hours. Osmond et al, CMAJ 2010 Minor Head Injury: CATCH Osmond et al, CMAJ 2010 Minor Head Injury: CATCH Subsequent multi-centre validation of CATCH rule Sensitivity of 87% with 4 high risk factors Sensitivity of 98% with 7 high and medium risk factors Required 38% of patients to undergo CT Main criticism: increased rate of CT likely due to inclusion of all MVCs and boggy hematoma Poor sensitivity with high risk criteria – missed 4 ciTBI EDH Improved sensitivity with 7 criteria but still missed 1 EDH Osmond et al. CJEM. Vol 14. S1, 2012 Minor Head Injury: PECARN Identification of children at very low risk of clinically-important traumatic brain injuries: Inclusion criteria Any child with injury < 24 hours GCS 14-15 Looks at who does not need a CT rather than who needs a CT Kupperman et al, Lancet 2009 Minor Head Injury: PECARN < 2 y/o Kupperman et al, Lancet 2009 Minor Head Injury: PECARN > 2 y/o Kupperman et al, Lancet 2009 Minor Head Injury Optimal clinical decision rule not yet established PECARN vs CATCH vs CHALICE Single site external validation comparing physician judgment to 3 decision rules Physician judgment and PECARN only rules to identify all clinically important TBIs Both CATCH and CHALICE missed clinically important TBIs CATCH had lowest specificity (Sens 91%, Spec 44% Annals of EM. 64 (2). Aug 2014 Child Abuse Suspect if history vague, changing, inconsistent with degree of injury or child’s development Bruises Can not date bruises by color “If they don’t cruise they don’t bruise” Uncommon for toddlers to bruise buttocks, genitalia, inner arms or legs, neck or trunk Patterned marks – linear, hand prints Bites – adult if > 3 cm Child Abuse Fractures Metaphyseal (corner, bucket handle) shearing force from shaking usually < 1yr Posterior ribs Femoral in non-ambulatory child Scapular, sternal, spinous process Multiple fractures, different ages Low risk – clavicle, tibia in toddler Child Abuse Skull fractures Multiple, occipital, wide Retinal hemorrhages Multiple layers with peripheral extension most specific for abuse Bilateral, flame shaped uncommon in accidental trauma (<1.5%) Child Abuse Admit all children < 2 yrs Skeletal survey for < 2 yrs (consider for 2-5 yrs) CT head if < 1 yr Opthalmologic exam Ideally within 24 hours (must be <72 hrs) Arrange clinical photography of marks/bruises Mandatory reporting to child welfare agency Questions? Thank you!