Reproductive System
advertisement

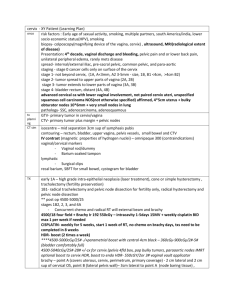
Reproductive System ZOYA MINASYAN, RN, MSN-EDU Benign Prostate Hyperplasia Enlargement of prostate gland resulting from increase in number of epithelial cells and stromal tissue Enlargement gradually compresses urethra. Partial or complete obstruction Compression leads to clinical symptoms. Most common urologic problem in males Occurs in 50% of men over 50 and 90% of men over 80 Approximately 25% will require treatment by age 80. Does not predispose to development of prostate cancer Benign Prostate Hyperplasia Benign prostatic hyperplasia. The enlarged prostate compresses the urethra. Etiology and Pathophysiology Possible risk factors Family history Obesity Increased waist circumference Physical activity level Alcohol consumption, smoking Diabetes Clinical Manifestations Symptoms categorized into two groups Obstructive symptoms Due to urinary retention Decrease in force of urinary stream Difficulty in initiating urination Dribbling at end of voiding Irritative symptoms Associated with inflammation or infection Urinary frequency and urgency Dysuria Bladder pain Nocturia Incontinence Complications Related to urinary obstruction Acute urinary retention complication with sudden, painful, inability to urinate Treatment involves catheter insertion and possible surgery UTI and sepsis Incomplete bladder emptying with residual urine-provides medium for bacterial growth. Calculi may develop in bladder because of alkalinization of residual urine. Renal failure: caused by hydronephrosis (swelling of kidney due to a backup of urine) Pyelonephritis (an ascending urinary tract infection that has reached the pyelum (pelvis) of the kidney) Bladder damage Diagnostic Studies History and PE DRE ( digital rectal exam), prostate can be palpated by DRE. Urinalysis with culture( presence of infection). PSA level (Prostate-specific antigen is a protein produced by cells of the prostate gland). Serum creatinine (for renal insufficiency) TRUS scan(trans rectal ultrasound) for the size of prostate. Uroflometry (volume of urine expelled from the bladder per second) Cystoscopy for internal visualiziation of the urethra and bladder. Diagnostic Studies • Using DRE, the health care provider can estimate the size, symmetry, and consistency of the prostate gland. In BPH the prostate is symmetrically enlarged, firm, and smooth. • A urinalysis with culture is routinely done to determine the presence of infection. The presence of bacteria, white blood cells, or microscopic hematuria is an indication of infection or inflammation. • Serum creatinine: • • • Creatinine is a chemical waste molecule that is generated from muscle metabolism. Creatinine is produced from creatine, a molecule of major importance for energy production in muscles. Creatinine is transported through the bloodstream to the kidneys. The kidneys filter out most of the creatinine and dispose of it in the urine. As the kidneys become impaired for any reason, the creatinine level in the blood will rise due to poor clearance by the kidneys. • TRUS scan allows for accurate assessment of prostate size and is helpful in differentiating BPH from prostate cancer. Biopsies can be taken during the ultrasound procedure. • Uroflowmetry is helpful in determining the extent of urethral blockage and thus the type of treatment needed. • Cystoscopy is performed if the diagnosis is uncertain and in patients who are scheduled for prostatectomy. Allowing internal visualization of the urethra and bladder. Collaborative Care Drug therapy: 5α-Reductase inhibitors Example: finasteride (Proscar), dutasteride (Avodart) ↓ size of prostate gland Takes 3 to 6 months for improvement Side effects: decreased libido, decreased volume of ejaculation, ED (erectile Disfx) α-Adrenergic receptor blockers Examples: tamsulosin (Flomax), doxazosin (Cardura), silodosin (Rapaflo) Promotes smooth muscle relaxation in prostate; facilitates urinary flow Improvement in 2 to 3 weeks Side effects: orthostatic hypotension and dizziness, retrograde ejaculation, nasal congestion Collaborative Care Transurethral microwave therapy (TUMT) Outpatient procedure: delivers microwaves directly to prostate through a transurethral probe Heat causes death of tissue and relief of obstruction. Postop urinary retention is common. Patient sent home with catheter 2 to 7 days Antibiotics, pain medication, and bladder antispasmodic medications given. Anticoagulant therapy should be stopped 10 days before treatment. Collaborative Care Transurethral needle ablation (TUNA) ↑ temperature of prostate tissue for localized necrosis Low-wave frequency used Only tissue in contact with needle affected Majority of patients show improvement in symptoms. Outpatient uses local anesthesia and sedation. Lasts 30 minutes with little pain and quick recovery Complications include urinary retention, UTI, and irritative voiding symptoms. Some patients require a catheter. Hematuria up to a week Collaborative Care Laser prostatectomy Delivers a laser beam transurethrally to cut or destroy parts of the prostate Common procedure: visual laser ablation of the prostate (VLAP) Takes several weeks to reach optimal results Urinary catheter inserted Contact laser techniques Minimal bleeding during and after procedure Fast recovery time Patients may take anticoagulants. Photovaporization of the prostate 12 Collaborative Care Transurethral resection (TURP) Removal of obstructing prostate tissue using resectoscope inserted through urethra Outcome for 80% to 90% is excellent. Relatively low risk Performed under spinal or general anesthesia and requires hospital stay Bladder irrigated for first 24 hours to prevent mucous and blood clots Complications include bleeding, clot retention, dilutional hyponatremia. Patients must stop anticoagulants before surgery. 13 Nursing Implementation Focus: early detection and treatment Yearly physical exam and DRE for men over 50 Educate patients that alcohol, caffeine, and cold and cough meds can increase symptoms. Instruct patient with obstructive symptoms to urinate every 2 to 3 hours and when first feeling urge. Teach for adequate fluid intake. Use aseptic technique when using urinary catheter. Administer antibiotics preoperatively. Nursing Implementation Postoperative care Postop bladder irrigation to remove blood clots and ensure drainage or urine Administer antispasmodics. Teach Kegel exercises. Observe patient for signs of infection. Dietary intervention Stool softeners to prevent straining Prostate cancer Is a malignant tumor of the prostate gland One out of five men will develop at some point during there life Early stages are asymptomatic and later on symptoms of BPH Pain that radiate down to the hips or legs plus urinary symptoms may indicate metastasis Prostatitis Acute and chronic results from organisms reaching the prostate gland by Ascending from the urethra Descending from the bladder Invasive via bloodstream or lymphatic channels Common causative organisms are- Escherichia coli, Klebsiells Pseudominas, Enterobacter, Proteus, Chlamydia trachomatis, Neisseria gonorrhoeae, and group D streptococci. Common manifestation: Fever, chills, back pain, perineal pain, dysuria, frequency, urgency, and cloudy urine, prostatic swelling, tender and firm. Dx: urinanalysis (UA) and urine culture for WBC and bacteria presence Nursing mangement: antibiotics bactrium, cipro, floxin, vibramycin or tetracyclin. Given 4 weeks for acute bacterial prostetitis Oral 4-12 weeks Imunocompromised given for lifetime. Problems Hypospadias: urethral meatus is located on the ventral surface of the penis Epispadias: an opening of the urethra on the dorsal surface Phimosis: tightness or constriction of the foreskin around the head of the penis Paraphimosis: tightness of the foreskin resulting in inability to pull it forward Priapism: painfull erection lasting >6hour caused by obstruction of the venous outflow in the penis Peyronie’s disease: curved penis caused by plaque formation in one of the corpora cavernosa Epididymitis: inflammation caused by infection trauma, urinary reflux Orchitis: inflammation of testes; painful, tender and swollen Cryptochidism: un-descended testes into the scrotal sac before birth Hydrocele: fluid filled mass results from lymphatic mallfunction Spermatocele: sperm containing painless cyst of the epidiydimis Varicocele: dilation of the veins that drain the testes Testicular torsion: twisting of the spermatic cord that supplies blood to the testes and epididymis Erectile dysfunction: ED caused by DM, vascular disease, decreased hormones, trauma, stress, depression, Vasectomy: bilateral surgical ligation or resection of the vas deferens. Done in 15-30 min, local anesthesia Andropause: decline in androgen with aging, decreased level of testosterone Sexually Transmitted Diseases (STDs) STDs are diseases that can be transmitted during intimate sexual contact. Most prevalent communicable diseases in the US. Most cases occur in adolescents and young adults. - STDs in infants and children usually indicate sexual abuse and should be reported. The nurse is legally responsible to report suspected cases of child abuse. Nursing Assessment 1. 2. 3. 4. 5. 6. 7. 8. Syphilis ( Treponema Pallidum) Gonorrhea (Neiserria Gonorrheae) Chlamydia ( Chlamydia Trachomatis) Trichomoniasis ( Trichomonas Vaginales) Candidiasis ( Candida Albicans) Herpes Type 2 (herpes Simplex Virus 2) HPV ( Human Papilloma Virus) HIV and AIDS ( Human Immunodeficiency Virus) STDs Nursing Diagnoses Deficient Knowledge related to Anxiety related to Anticipatory grieving related to Nursing Plan and Interventions Use a non judgmental approach. Be straightforward when taking history. All information is strictly confidential. Obtain a complete sexual history. Develop teaching Plan include: Sign and symptom of STDs. Mode of transmission of STDs Reminder that sexual contact should be avoided with anyone while infected. Concise written instruction about treatment; request a return verbalization of these instructions to ensure the client has heard the instructions and understands them. Encourage client to provide information regarding all sexual contacts. Report incidents of STDs to appropriate health agencies and departments. Instruct women of childbearing age about risk to a newborn: a. Gonorrheal conjuctivitis b. Neonatal herpes c. Congenital syphilis d. Oral candidiasis Teach safer sex Nursing Plan and Interventions Safer sex behavior include: a. b. c. d. e. f. g. h. Reduce the number of sexual contacts. Avoid sex with those who have multiple partners. Examine genital area and avoid sexual contact if anything abnormal is present. Wash hands and genital area before and after sexual contact. Use a latex condom as a barrier. Use water based lubricants rather than oil based lubricants. Avoid douching before and after sexual contact: douching increase the risk for infections because the body’s normal defenses are reduced or destroyed. Seek attention from health care provider immediately if symptoms occur. Complications Complications of STD’s Pelvic Inflammatory Disease (PID) Sterility Ectopic pregnancy Blindness Cancer (associated with HPV) Fetal and infant death Birth defects Mental retardation AIDS has a set of complications much broader than the other STD’s Sexually Transmitted Diseases Infectious diseases most commonly transmitted through sexual contact Can also be transmitted by Blood Blood products Autoinoculation Can be bacterial or viral Usually start as lesions on genitals or mucous membranes and can spread to other areas All cases of gonorrhea and syphilis (and in most states chlamydia) must be reported to state or local public health authorities. Still underreported. Sexually Transmitted Diseases Changes in methods of contraception Condom is best protection against STDs but still is not used frequently in general population. Oral contraceptive effects on acidity of vaginal/cervical secretions promote growth of certain organisms, causing STDs. Gonorrhea: Etiology and Pathophysiology Caused by Neisseria gonorrheae Gram-negative bacteria Direct physical contact with infected host Mucosa with columnar epithelium is susceptible. Present in genitalia, rectum, and oropharynx Easily killed by drying, heating, or washing with antiseptic Incubation period: 3 to 8 days Provides no immunity to subsequent reinfection Elicits inflammatory process that can lead to fibrous tissue and adhesions Tubal pregnancy Chronic pelvic pain Infertility in women Neonates can develop a gonococcal infection from an infected mother during delivery. Gonorrhea Clinical Manifestations Men Initial site infection is urethra. Symptoms Develop 2 to 5 days after infection Dysuria Profuse, purulent urethral discharge Unusual to be asymptomatic Gonococcal Urethritis Profuse, purulent drainage in a patient with gonorrhea. Gonorrhea : Clinical Manifestations Women Mostly asymptomatic or have minor symptoms Vaginal discharge Dysuria Frequency of urination After incubation Redness and swelling occur at site of contact. Greenish, yellow purulent exudates often develops. May develop abscess Disease may remain local or may spread by tissue extension to uterus, fallopian tubes, and ovaries. Endocervical Gonorrhea Endocervical gonorrhea. Cervical redness and edema with discharge. Gonorrhea: Clinical Manifestations Eye infections in newborns Instillations of prophylactic erythromycin (0.5%) ophthalmic ointment or silver nitrate (0.1%) aqueous solution Untreated infants develop permanent blindness. Orogenital: Gonococcal pharyngitis can develop. Anorectal gonorrhea: Usually from anal intercourse Symptoms include soreness, itching, and discharge of anus. Complications Women Include pelvic inflammatory disease (PID), Bartholin’s abscess (the buildup of pus that forms a lump (swelling) in one of the Bartholin's glands, which are located on each side of the vaginal opening), ectopic pregnancy, and infertility Usually asymptomatic, so seldom seek treatment Small percentage develop disseminated gonococcal infection (DGI). Skin lesions, fever, arthralgia, arthritis, or endocarditis Men Include prostatitis, urethral strictures, and sterility Often seek treatment early, so less likely to develop complications Disseminated Gonococcal Infection (DGI) Skin lesions with disseminated gonococcal infection. A, On the hand. B, On the fifth toe. Gonorrhea: Diagnostic Studies Women Smears and discharge do not establish diagnosis. Female GU tract harbors organisms resembling N. gonorrhea. Must have culture to confirm diagnosis Drug therapy Treatment in early stage is curative. Most common Oral dose of cefixime (Suprax) IM dose of ceftriaxone (Rocephin) Fluoroquinolones are no longer used. Patients with coexisting syphilis are likely to be treated with azithromycin (Zithromax) or doxycycline (Vibramycin). Gonorrhea: Collaborative Care All sexual contacts of patients must be evaluated and treated. Patient should be counseled to abstain from sexual intercourse and alcohol during treatment. Reexamine if symptoms persist after treatment. Syphilis: Etiology and Pathophysiology • • Caused by Treponema pallidum; Spirochete bacterium Enters the body through breaks in skin or mucous membranes Facilitated by abrasions that occur during sexual intercourse Causes production of antibodies that react with normal tissues • Destroyed by drying, heating, or washing May also be spread through Contact with infectious lesions Sharing of needles among IV drug users Spread in utero after 10th week of pregnancy Infected mother has a greater risk of stillbirth or of having a baby who dies shortly after birth. • Association with HIV Syphilitic lesions on the genitals enhance HIV transmission. Syphilis: Clinical Manifestations Variety of signs/symptoms can mimic another disease. Neurosyphilis causes degeneration of brain with mental deterioration. Sudden attacks of pain Loss of vision and sense of position Primary stage Chancres appear. Painless indurated lesions Occur 10 to 90 days after inoculation Lasting 3 to 6 weeks See Table 53-3 for more information. Chlamydial Infections: Clinical Manifestations Men Urethritis Dysuria Urethral discharge Proctitis Rectal discharge Pain during defecation Urethritis Dysuria Urethral discharge Proctitis Rectal discharge Pain during defecation Women Cervicitis Urethritis Purulent exudate Perihepatitis Dysuria Frequent urination Pyuria Bartholinitis Mucopurulent discharge Hypertrophic ectopy Fever, nausea, vomiting, right upper quadrant pain PID Abdominal pain, nausea, vomiting, fever, malaise, abnormal vaginal bleeding, menstrual abnormalities Can lead to chronic pain and infertility Chlamydial Infection Chlamydial epididymitis. Red, swollen scrotum. Genital Herpes: Etiology and Pathophysiology Caused by herpes simplex virus (HSV) Enters through mucous membranes or breaks in the skin during contact with infected persons HSV reproduces inside cell and spreads to surrounding cells. Virus enters peripheral or autonomic nerve endings. Ascends to sensory or autonomic nerve ganglion, where it is dormant Recurrence when virus descends to initial site of infection Persists for life Genital Herpes: Clinical Manifestations Primary (initial) episode Burning or tingling at site Small vesicular lesion appear on penis, scrotum, vulva, perineum, perianal areas, vagina, or cervix. Vesicles contain large quantities of infectious virus particles. Complications Autoinoculation to extragenital sites Lips, breasts, and fingers High risk of transmission in pregnancy with episode near delivery Active lesion is indication for cesarean section. Unruptured Vesicles Unruptured vesicles of herpes simplex virus type 2 (HSV-2). A, Vulvar area. B, Perianal area. C, Penile herpes simplex, ulcerative stage. Autoinoculation of Herpes Simplex Virus Autoinoculation of herpes simplex virus (HSV) to the lips. Genital Herpes: Collaborative Care Drug therapy Inhibit viral replication Suppress frequent recurrences Acyclovir (Zovirax) Valacyclovir (Valtrex) Famciclovir (Famvir) Not a cure, but shorten duration and healing time and reduce outbreaks Symptomatic care Genital hygiene Loose-fitting cotton underwear Lesions clean and dry Sitz baths Barrier methods during sexual activity Genital Warts Estimated 20 million Americans are currently infected. Most common STD in the United States Caused by human-papilloma-virus (HPV) Usually types 6 and 11 Highly contagious Frequently seen in young, sexually active adults Incubation period: 3 to 4 months Discrete single or multiple growths White to gray and pink-fleshed colored May form large cauliflower-like masses Genital Warts Genital warts. A, Severe vulvular warts. B, Perineal wart. C, Multiple genital warts of the glans penis. Genital Warts: Collaborative Care Treatments Chemical Patient managed Trichloroacetic acid (TCA) Bichloroacetic acid (BCA) Podophyllin resin For small external genital warts Podofilox (Condylox/Condylox gel) Imiquimod (Aldara) Immune response modifier If warts do not regress with previously mentioned therapies Cryotherapy with liquid nitrogen (freezing a wart using a very cold substance). Electrocautery (to cut through soft tissue to access a surgical site) Laser therapy Use of α-interferon (to trigger the protective defenses of the immune system) Surgical removal Nursing management Subjective data Past medical history, including sexual history Medication use IV drug use Nausea/vomiting Dysuria Urethral discharge Burning lesions Vaginal discharge Presence of genital or perianal lesions Objective data Fever Visual assessment of lesions, warts, rash Purulent rectal discharge Proctitis Urethral and cervical discharge Laboratory findings Nursing Diagnoses Risk for infection Anxiety Ineffective health maintenance Nursing Management: Planning Patient with STD will Demonstrate understanding of mode of transmission and risks imposed Complete treatment and follow-up Notify or assist in notification of sexual contacts Abstain until infection is resolved Demonstrate knowledge of safer sex practices Nursing Management: Nursing Implementation Discuss practices with all patients. Teach to inspect partner’s genitals. Some protection if void immediately after intercourse; wash genitalia and adjacent areas with soap and water Proper use of condoms Avoiding sexual contact with HIV-infected persons Compassion and respect Locating and examining all contacts of person with STD for testing and treatment Counseling to verbalize feelings Explaining side effects, need for treatment adherence, and follow-ups Emphasize hygiene (hand washing, bathing). Avoid douching. Avoid synthetic materials in undergarments. Abstinence during treatment period, condoms afterward Avoid oral-genital contact. Nursing Management:Evaluation Patient with STD will Demonstrate modes of transmission Use appropriate hygienic measures Experience no reinfection Demonstrate compliance with follow-up protocol Question When caring for a patient with a sexually transmitted disease, it is important that the nurse teach the patient to: 1. Advise all sexual partners of the need for treatment. 2. Use a condom for sexual intercourse during treatment. 3. Engage in monogamous relationships to prevent reinfection. 4. Wash the genitalia before sexual intercourse to prevent disease transmission. Question The nurse teaches the patient with genital herpes about the use of: 1. Acyclovir ointment. 2. Oral acyclovir (Zovirax). 3. Human papillomavirus vaccine. 4. Podofilox (Condylox) topical gel. PID ( Pelvic Inflammatory Disease) It involves one or more of the pelvic structures. Fallopian tubes (salpingitis) Ovaries (oophoritis) Pelvic peritonitis (peritonitis) PID is often the result of untreated cervicitis: infection ascends to cervix-uterus-fallopian tubesovaries-peritoneal cavity. Chlamydia trachomatis and Neisseria gonorrhoeas are the most common organisms of PID. Pelvic Inflammatory Disease Pelvic inflammatory disease. Acute infection of the fallopian tubes and ovaries. The tubes and ovaries have become an inflamed mass attached to the uterus. A tubo-ovarian abscess is also present. PID ( Pelvic Inflammatory Disease) Clinical manifestation: Lower abdominal pain Walking can increase the pain Spotting after intercourse-purulent discharge from cervix or vagina Cramping pain with menses, irregular bleeding Lower abdominal tenderness Tubo-ovarian abscess may leak or rupture resulting in pelvic or generalized peritonitis Embolisms may occur as the result of thrombophlebitis of the pelvic veins Septic shock and Fritz-Hugh-Curtis syndrome When PID spreads to liver and causes acute perihepatitis Collabotative care: Manage the pain associated with PID with analgesics and warm sitz baths. Bedrest in a semi-fowler position may increase comfort and promote drainage. Antibiotic treatment is necessary to reduce inflammation and pain Doxycycline (Vibromycin) Cefoxitin (Mefoxin) Extreme cases-hysterectomy Cystocele Definition: is a protrusion of the bladder through the vaginal wall. Commonly called “bladder drop”, refers to the dropping or sagging of the vagina in the anterior or upper compartment. Etiology : Caused by weakened pelvic muscles or structures. When the pubocervical fascia detaches from its upper, lower or lateral attachments a can occur. The pubocervical fascia is connective tissue that is between the bladder and anterior vaginal wall and serves as its support structure. The anterior vaginal wall is attached to the cervix at the upper portion and has attachments to the pubic bone on the lower portion. Cystocele Common symptoms: tissue protruding from the vagina, pelvic pressure, loss of ability to empty bladder to completion, pain with intercourse, positional bladder voiding, and vaginal pain. For mild s/s medical treatment can be tried. Surgery maybe indicated if not successful. Cystocele Rectocele Definition: It is a protrusion of the anterior rectal wall through the posterior vaginal wall. Etiology: Caused by a defect of the pelvic structures or a difficult delivery or forceps delivery. Rectocele The rectovaginal septum is the connective tissue that separates the rectum (bowel) from the vagina. Defects in the rectovaginal septum can result in a rectocele. The rectovaginal septum is attached at its upper portion to the cervix and the lower portion to the perineum. The perineum is the space between the vaginal opening and the anus. A rectocele occurs when a break in the septum allows the rectum to push into the vaginal area. Rectocele Symptoms Tissue protrusion from the vagina, pelvic pressure, inability to empty bowels, pain with intercourse, and discomfort with physical activities. Mild s/s can also be medical treatment can also be tried. If not successful, surgery maybe indicated. Rectocele Risk Factors for Cystocele and Rectocele Risk Factors for Cystocele Obesity Advanged age (loss of estrogen) Chronic constipation Family History Childbearing Risk Factors for Rectocele Pelvic structure defects Difficult childbirth Forceps Delivery Previous hysterectomy Diagnostic Procedures: Cystocele and Rectocele Cystocele: Pelvic Examination – reveals a bulging of the anterior wall when the client is instructed to bear down. Voiding cystourethrography to identify the degree of bladder protrusion and amount of urine residual. Rectocele: Pelvic examination reveals a bulging of the posterior wall when the client is instructed to bear down Rectal examination and /or barium enema reveals presence of rectocele. Surgeries: Cystocele : Anterior colporrhaphy – This uses a vaginal approach, the pelvic muscles are tightened. Rectocele: Posterior colporrhapy – Using a vaginal perineal approach, the pelvic muscles are tightened. Anterior Posterior Repair if surgery for both Cystocele and Rectocele is indicated. Nursing Interventions: Cystocele and Rectocele Assessments: Monitor for signs and symptoms of a Cystocele: Urinary frequency Urinary urgency Stress incontinence Urinary tract infection Sense of vaginal fullness Monitor for signs and symptoms of a Rectocele: Constipation Hemorrhoids Sensation of mass in the vagina Pelvic pressure pain Difficulty with intercourse. Nursing Interventions: Cystocele and Rectocele 1. Avoid traumatic vaginal childbirth – early and adequate episiotomy. An episiotomy is a surgical incision made in the area between the vagina and anus (perineum). This is done during the last stages of labor and delivery to expand the opening of the vagina to prevent tearing during the delivery of the baby. 2. Inform the client about measures to prevent atrophic vaginitis and of the advantage of prevention. Atrophic vaginitis (also known as vaginal atrophy or urogenital atrophy) is an inflammation of the vagina (and the outer urinary tract) due to the thinning and shrinking of the tissues, as well as decreased lubrication. This is all due to a lack of the reproductive hormone estrogen. The most common cause of vaginal atrophy is the decrease in estrogen which happens naturally during perimenopausal, and increasingly so in post-menopausal stage. However this condition can sometimes be caused by other circumstances. . 3. To loose weight if obese. 4. To eat high-fiber diet and drink adequate fluids to prevent constipation. Nursing Interventions: Cystocele and Rectocele 1. Kegel exercises – tightened pelvic muscles for a count of 10, relax slowly for a count of 10 repeat in sequences of 15 in lying down, sitting, and standing position. Kegel exercises are said to be good for treating vaginal prolapse and preventing uterine prolapse in women and for treating prostate pain and swelling resulting from benign prostatic hyperplasia(BPH) and prostatitis in men. Nursing Interventions: Cystocele and Rectocele 2. Estrogen Therapy – to prevent uterine atrophy and atrophic vaginitis. Inform client of client’s risk from complication of hormone therapy. E.g. cardiovascular or embolic history. Monitor for s/e of estrogen therapy e.g. water retention, headaches. 3. Weight loss and changes in diet. 4. Vaginal Pessary – removable rubber, plastic or silicon device inserted into the vagina to provide support and block protrusion into vagina. Teach client how to insert, remove, and clean the device. Monitor for possible bleeding or fistula formation. Vaginal Pessary A vaginal pessary is a removable device placed into the vagina. It is designed to support areas of pelvic organ prolapsed. Post – Operative Care: Cystocele and Rectocele 1. Administer analgesics, antimicrobials, and stool softeners/laxatives as prescibed. 1. Provide perineal care at least twice daily following surgery and after urination or bowel movement. 2. Apply an ice pack to relieve pain and swelling. 3. Suggest that the client take frequent warm sitz baths to soothe the perineal area. A sitz bath is a plastic tub that fits over the toilet and can be filled with water. Sitting in the warm water for 15 to 20 minutes can provide relief from the discomfort from hemorrhoids, fistulas, anal fissures, or an episiotomy (surgically planned incision on the perineum and the posterior vaginal wall during the labor). This can be done by sitting in a bathtub filled with a few inches of water, but using a plastic sitz bath that fits over the toilet is often more convenient. Post-Operative Care: Cystocele and Rectocele 5. Provide a liquid diet followed by low – residue diet until normal bowel function returns. 6. Instruct client how to care for indwelling catheter at home. 7. Recommend to client to drink at least 2,000 ml of fluid daily, unless contraindicated. 8. Following removal of the catheter, instruct the client to void every 2-3 hour to prevent a full bladder and stress on stitches. 9. Teach the client how to perform client intermittent self-catheterization techniques in the event that client is unable to void. Post-operative Care: Cystocele and Rectocele 10. Caution the client to avoid straining at defecation, sneezing, coughing, lifting, and prolonged sitting, walking, or standing following surgery. 11. Instruct the client to tighten and support pelvic muscles when coughing or sneezing. 12. Post-operative restrictions include avoidance of strenuous activity, weight lifting greater than 5 lbs. and sexual intercourse. Client may stay in the hospital from 1 to 2 days. Will probably be able to return to normal activities in about 6 weeks. Avoid strenuous activity for the first 6 weeks, and increase activity level gradually. Most women are able to resume sexual intercourse in about 6 weeks. Complications :Cystocele and Rectocele Residual urine in the bladder at risk for recurrent bladder infection and possibly kidney infections. Constipation. Dyspareunia (painful sexual intercourse) is a possible surgical complication due to surgical alteration of the orifice. Needs of Older Adults: Cystocele and Rectocele Cystocele and rectocele develop in older female clients usually following menopause. Older clients tend to overuse laxatives and enemas for the relief of constipation. Older adults are more susceptible to post- operataive complications. Performing Kegel exercises and manipulating pessary maybe more difficult for older adults. Uterine Prolapse Occurs when pelvic floor muscles and ligaments stretch and weaken, providing inadequate support for the uterus. The uterus then descends into the vaginal canal. Uterine Prolapse affects postmenopausal women who've had one or more vaginal deliveries. Damage to supportive tissues during pregnancy and childbirth. Effects of gravity. Loss of estrogen. Repeated straining over the years which can weaken pelvic floor and lead to uterine prolapse. Pregnancy and trauma incurred during childbirth, particularly with large babies or after a difficult labor and delivery. Loss of muscle tone associated with aging In rare circumstances, may be caused by a tumor in the pelvic cavity. Genetics : Women of Northern European descent have a higher incidence of uterine prolapse than do women of Asian and African descent. Uterine Prolapse: Risk Factors One or more pregnancies and vaginal births Giving birth to a large baby Increasing age Frequent heavy lifting Chronic coughing Frequent straining during bowel movements Genetic predisposition to weakness in connective tissue Some conditions, such as obesity, chronic constipation and chronic obstructive pulmonary disorder (COPD), can place a strain on the muscles and connective tissue in the pelvis and may play a role in the development of uterine prolapse. Uterine Prolapse Uterine Prolapse Sign and Symptoms: Mild uterine prolapse client may experience no signs or symptoms. Moderate to severe uterine prolapse - Sensation of heaviness or pulling in pelvis - Tissue protruding from your vagina - Urinary difficulties, such as urine leakage or urine retention - Trouble having a bowel movement - Low back pain - Feeling as if sitting on a small ball or as if something is falling out of vagina - Sexual concerns - Symptoms that are less in the morning and worsen as the day goes on. Test and Diagnostic Procedures Pelvic exam. A complete pelvic exam -Client will be examined while lying down and while standing up. Your physician may ask client to bear down as if having a bowel movement to see how much that affects the degree of prolapse. To check the strength of your pelvic muscles, client may also be instructed to contract them, as if you are stopping the stream of urine. Imaging tests. -Ultrasound or magnetic resonance imaging (MRI) Uterine Prolapse - Treatment For mild uterine prolapse, treatment usually is not needed. Options include using a supportive device (pessary) inserted into the vagina or having surgery to repair the prolapse. Loosing weight, stopping smoking Lifestyle changes Achieve and maintain a healthy weight, to Perform Kegel exercises, to strengthen pelvic floor muscles. Avoid heavy lifting and straining, to reduce abdominal pressure on supportive pelvic structures. Surgical Procedure Vaginally – less pain after surgery, faster healing and a better cosmetic result. However, vaginal surgery may not provide as lasting a fix as abdominal surgery. If the uterus is not removed during surgery, prolapse can recur. Laparoscopic techniques — using smaller abdominal incisions, a lighted camera-type device (laparoscope) to guide the surgeon— offer a minimally invasive approach to abdominal surgery. Client might not be a good candidate for surgery to repair uterine prolapse if still plan to have more children. Pregnancy and delivery of a baby put strain on the supportive tissues of the uterus and can undo the benefits of surgical repair Complications Possible complications of uterine prolapse include: Ulcers-part of the vaginal lining may be displaced by the fallen uterus and protrude outside the body, rubbing on underwear. The friction may lead to vaginal sores (ulcers); the sores could become infected. Prolapse of other pelvic organs. If client experienced uterine prolapse, client may also have prolapse of other pelvic organs, including your bladder and rectum. A prolapsed bladder (cystocele) bulges into the front part of client’s vagina, which can lead to difficulty in urinating and increased risk of urinary tract infections. Weakness of connective tissue overlying the rectum may result in a prolapsed rectum (rectocele), which may lead to difficulty having bowel movements. Abnormal Vaginal Bleeding Balloon thermotherapy for treatment of menorrhagia. A, Balloon-tipped catheter is inserted into the uterus through the vagina and cervix. B, The balloon is inflated with a sterile fluid that expands to fit the size and shape of the uterus. The fluid is heated to 188° F (87° C) and maintained for 8 minutes while the uterine lining is treated. C, Fluid is withdrawn from the balloon and the catheter is removed. Abnormal Vaginal Bleeding Menorragia-excessive or prolonged bleeding Oligomenorrhia-long intervals between meses-more than 35 days Metrorrhagia- irregular bleeding or bleeding between menses Ectopic Pregnancy Ectopic pregnancy occurring in the fallopian tube. Nursing and Collaborative Management: Ectopic Pregnancy Laparoscopic treatment of ectopic pregnancy in the right fallopian tube. Ectopic Pregnancy Implantation of the fertilized ovum anywhere outside the uterine cavity Can cause abdominal pain, vaginal bleeding, breast tenderness, GI disturbance Breast disorders Mastalgia- breast pain Mastitis- inflammatory condition Fibroadenoma-benign breast lumps Fibrocystic changes-benign condition caused by development of excess fibrous tissue and cyst formation Breast cancer Risk factor Female Age of >50 Family history Early menarche (before age 12) Pregnancy after 30 Weight gain Physical inactivity Alcohol consumption Exposure to ionizing radiation