LCME Self-Study Summary August 30 with formatting_Beck
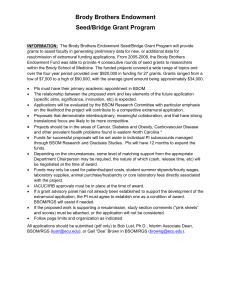
advertisement

LCME Self-Study Summary Report The Brody School of Medicine East Carolina University Greenville, North Carolina October 1, 2011 i Table of Contents Introduction ................................................................................................................................................. 1 Prior Findings by the LCME ..................................................................................................................... 1 I. Institutional Setting ........................................................................................................................ 2 A. Governance and Administration ........................................................................................... 2 B. Academic Environment .............................................................................................................. 4 II. Educational Program for the M.D. Degree................................................................................... 8 A. Educational Objectives ........................................................................................................... 8 B. Structure of the Educational Program ................................................................................ 10 C. Teaching and Evaluation ...................................................................................................... 12 D. Curriculum Management ..................................................................................................... 14 E. Evaluation of Program Effectiveness ...................................................................................... 16 III. Medical Students ....................................................................................................................... 17 A. Admissions ................................................................................................................................. 17 B. Student Services ........................................................................................................................ 21 C. The Learning Environment...................................................................................................... 24 IV. Faculty........................................................................................................................................ 26 A. Number, Qualifications and Functions ................................................................................... 26 B. Personnel Policies ...................................................................................................................... 28 C. Governance ................................................................................................................................ 29 V. Educational Resources.................................................................................................................. 30 A. Finances ..................................................................................................................................... 30 B. General Facilities ........................................................................................................................ 34 C. Clinical Teaching Facilities .................................................................................................. 34 D. Information Resources and Library Services......................................................................... 37 Summary.................................................................................................................................................... 39 ii Introduction The Brody School of Medicine (BSOM) at East Carolina University (ECU) presents this self-study summary report to the Liaison Committee on Medical Education (LCME) for consideration in our accreditation process. The self-study began on December 11, 2009 and is the result of analysis and collaboration among 123 faculty, students, resident physicians, staff and administrators. All subcommittee chairs met with their respective section committees and prepared responses to their section standards to be reviewed by members of the steering committee by February 2011. The steering committee members co-edited each section collaboratively with the subcommittee chairs and presented each section report for review by the entire steering committee during weekly meetings from March 2011 to August 2011. All members of the data base committees had access to the LCME intranet “SharePoint” site designed as an electronic repository for reports throughout the study period of 21 months. Prior Findings by the LCME The most recent LCME accreditation report was received on June 8, 2004. The following programs have been instituted to address areas of concern or non-compliance in response to the 2004 accreditation site visit. . ED-2 : With the help of new Associate Dean of Medical Education in 2004, all clerkships developed objectives defining the types of patients, procedures, level of responsibility and clinical setting in which these patients should be assessed. A log book data collection process was implemented and has been monitored since 2005 by the Office of Medical Education. Mid-term feedback sessions were also implemented and are monitored by clerkship directors. ED-33: The institutional responsibility to integrate, manage and evaluate the curriculum was initially addressed by using the AAMC CurrMIT tool. This worked for the basic science courses but was not effective for the clinical science courses. In order to integrate courses, a curriculum renewal project was begun in 2006 and the M3 and M4 curricular design was studied by clerkship directors, students and administrative leaders for approximately one year. Curriculum changes were presented to the Executive Curriculum Committee in 2007 and implemented in 2008-09. M3 changes included a new M3 elective (2 weeks), a new Cardiovascular course (2 weeks), shortened Psychiatry (6 weeks) and ObstetricsGynecology (6 weeks) clerkships, and a third year duration of 48 weeks instead of 50. M4 changes included a new Emergency Medicine clerkship (4 weeks), a new Clinical Neurosciences/PM&R clerkship (2 weeks), a new Intensive Care Unit requirement (4 weeks) and a reduction of elective time from 16 to 14 weeks. The curriculum renewal process was continued in 2009-10 for the M1 and M2 years. Two students were financially supported in a summer research opportunity to track redundancies and omissions in the M1 and M2 years. Their research was presented to the M1 and M2 course directors by the Assistant Dean of Academic Affairs for Basic Sciences and course directors revised or augmented courses. This has resulted in 15% fewer hours in the classroom and better integration of courses across the first two years. Further integration has occurred in the M2 year by the course directors of Pathology, Pharmacology, Introduction to Medicine, and Doctoring II courses. A fully integrated Physiology and Neuroanatomy course has been taught for over 10 years. A course review process was begun in 2006 under the leadership of the Office of Medical Education and involves formal review of course performance, content and evaluation approximately every 3-4 years. This course review system is conducted by the appropriate year curriculum committee with recommendations forwarded to the Executive Curriculum Committee (ECC). The ECC informs the responsible Department of strengths and areas for improvement on each course with a follow up expected from the Department of record. The medical school has contracted with a curriculum mapping software company (E*Value) and will be mapping curriculum content with this tool beginning in August 2011. 1 ED-32: A policy was adopted in September 2005 defining the “Appropriate Treatment of Medical Students in the Educational Setting”. See http://www.ecu.edu/cs-dhs/bsomstudentaffairs/BSOM_Policies.cfm The AAMC 2011 GQ Medical School Graduation Questionnaire report validates that 95.7 %( BSOM) vs. 88.7% (Nationally) in 2011 were aware of the policy and 15.2% (BSOM) vs. 16.8% (Nationally) reported an incident of mistreatment. This issue will need continued monitoring. FA-1: The BSOM strongly supports cultural diversity. The Vice Chairs of Diversity Initiatives is a standing committee supported by the Dean and composed of faculty and student representatives from each Department and medical school class. They sponsor monthly Diversity events at the BSOM and advise the Assistant Dean of Diversity Affairs. The Brody Women’s Faculty Committee is a formal committee also supported by the Dean. Their members include basic science and clinical science women who have researched such issues as retention, promotion and compensation among faculty. They sponsor annual symposia to support leadership. The BSOM also participated in the Faculty Forward project sponsored by the AAMC . This Faculty Forward committee continues to meet and report during faculty meetings on issues of success or concern. There are currently three women chairs among the Basic Science Departments and four women serving as Deans in administrative leadership roles. ER-7: Classroom space for students in the clinical years is adequate and the student lounge at Pitt County Memorial Hospital has been renovated with new appliances and computers. There is no longer a call room space issue. With regard to the areas in transition at the previous site visit: Several departments were served by interim chairs, but now only one department (Radiation Oncology) has an interim chair due to the recent illness of the serving Chair. Doctoring I has been enhanced in the past 8 years and integrated with the Doctoring II course. Their reviews are contained in the Course and Clerkship Review Section (VI) and are much improved. The financial status of the medical school is stable due to fiscal management of the state and practice plan budgets and continued success in procuring research grants. See the Educational Resources (V) database. The new Laupus Library is a valued resource for faculty and students. Access is safe and readily available. The addition of a student technology center housing computers and printers on the second floor of the medical school building allows 24 hour access for study and research. This area is devoted solely to students. I. Institutional Setting A. Governance and Administration 1. Describe how institutional priorities are set. Evaluate the utility and success of institutional planning efforts, and discuss how planning has contributed to the accomplishment of the program’s educational, research, and clinical services missions. The institutional priorities are aligned with and are set to follow the tripartite mission of the medical school to: 1) educate primary care physicians, 2) provide access to careers in medicine for minority and disadvantaged students, and 3) improve the health care services in eastern North Carolina. In our current strategic planning process, we use scenarios called Strategic Conversations that allow our Brody community (staff, faculty, students, and community) to enact change within the Brody 2 School of Medicine. Strategic planning is a continuous process. We are newly engaged in this process that includes the use of Appreciative Inquiry, as also employed at other institutions and elsewhere within the East Carolina University Campus. The process began in January 2011 as we look at the world around us and how we see the Brody School of Medicine and its community in the coming five years. The success of these activities will be measured not by their alignment with the future, but by the depth of the conversations - strategic conversations - that they evoke. The Strategic Conversations/Planning aims to 1) improve the environment by enriching our collaboration, enabling our success, and identifying and sticking to our priorities; 2) provide a clear road map to our future state by eliminating barriers and releasing the energy of faculty and staff; 3) develop empowered, engaged, and ecumenical employees; and 4) discover the energy of tomorrow. Each element of the mission is receiving analysis and strength by the continuous process of Strategic Conversations. This is defined by the stability of our student diversity at matriculation, the high percentage of graduates entering primary care, and the ever increased service and research commitments of our faculty. 2. Evaluate the role of the governance structure in the administrative functioning of the medical school. Is the governance structure appropriate for an institution of this size and these characteristics? Are there appropriate safeguards in place to prevent conflict of interest at the level of the governing board, are these safeguards being followed, and are these safeguards effective? Describe any situations that require review by or approval of the governing board (board of trustees) of the school or university prior to action being taken. The governing board with responsibility for the Brody School of Medicine at East Carolina University is the Board of Trustees of East Carolina University. The Board of Trustees consists of thirteen members with four appointed by the Governor, eight elected by the Board of Governors, and the president of the Student Government Association as an ex-officio member. The governance structure is appropriate for the size of East Carolina University and the Brody School of Medicine and is consistent with other public universities. In 2006, the NC General Assembly passed the State Government Ethics Act, providing safeguards to identify and manage conflicts of interest at the level of the faculty, the administration and the governing board. The statute requires that all Board of Trustees members (as well as senior university officials) file annual statements of economic interest and requires formal ethics and conflict-of-interest training for all Board of Trustee members. These safeguards have been effective. For example, a Board of Trustees member recused himself from a discussion and vote on a motion to name a locker room because the naming would honor two of the member’s relatives. 3. Evaluate the relationship of the medical school to the university and its clinical affiliates with respect to: a. The effectiveness of the interactions between medical school administration and university administration. b. The cohesiveness of the leadership among medical school administration, health sciences center administration, and the administration of major clinical affiliates. The Brody School of Medicine administration and East Carolina University administration are mutually linked in an organizational reporting structure. The Dean and the Vice Chancellor for 3 Health Sciences share the responsibilities of, and play an integral role in, advancing the University’s mission to improve healthcare in eastern North Carolina. The Dean, who also has the role of Senior Associate Vice Chancellor for Medical Affairs, advises the Vice Chancellor for Health Sciences and the Chancellor on all matters related to the practice of medicine and the education of physicians, biomedical scientists, and public health professionals. The primary teaching hospital and major clinical affiliate is Pitt County Memorial Hospital (renamed University Health Systems Medical Center [UHSMC] on 9-1-11). UHSMC is a private not-for-profit corporation that is owned by University Health Systems of Eastern Carolina. There is no governance relationship, direct or indirect, between the leadership of the School or University and the teaching hospital. However, there are financial reimbursements under a variety of contractual agreements with the hospital which support designated leadership of all clinical departments within the hospital by the clinical chairs of the medical school departments. Financial support from UHSMC for GME has recently been re-negotiated, resulting in an increase of 83% over the next three years. BSOM and UHSMC also have launched a joint venture partnership for a regional cancer center governed together. Dr. Ernest Larkin, Assistant Dean for Operations, supports the work of Dean Cunningham in facilitating the relationship of Brody School of Medicine and University Health Systems through his joint appointment and funding from both institutions. 4. Assess the organizational stability and effectiveness of the medical school administration (dean, dean's staff). Has any turnover in central administration staff affected medical school planning or operations? Are the number and types of medical school administrators (assistant/associate deans, other dean's staff) appropriate for efficient and effective medical school administration? Is departmental leadership stable? If there has been turnover in departmental leadership, are vacancies replaced in a timely manner without detriment to departmental functioning? Note any concerns arising from leadership turnover in the school’s central or departmental administration. The organizational stability of the Brody School of Medicine administration has proven quite effective in a time when major cuts in our state budget can cause decreased morale among faculty and staff. The Dean has provided strong leadership and continues to mentor his administrative team with biweekly meetings to discuss issues and build collaboration. Communication has been open and welcome for this administrative team and has helped to make the administrative team more cohesive and effective in the daily functioning of the medical school. The departmental leadership has proven stable. The Chair of Radiation Oncology is currently an interim position due to the illness of the chair. In the central administrator roles, Dr. Previll serves as the Interim Senior Associate Dean for Academic Affairs and a search is in progress to fill this position. The new positions of Assistant Deans for Academic Affairs in Basic Sciences and in Clinical Sciences have been filled by Drs. Carroll and Schenarts. They are senior faculty members who have served the medical school for many years. B. Academic Environment 5. Evaluate the graduate program(s) in basic sciences and other disciplines, including overall contribution to the missions and goals of the medical school. Describe the mechanisms for reviewing the quality of the graduate program(s) in basic sciences and comment on their effectiveness. Assess whether the graduate programs have an impact (positive or negative) on 4 medical student education. Describe opportunities for interaction between medical and graduate students and the frequency of those interactions. The graduate programs play a critical role at the Brody School of Medicine in undergraduate medical education. Graduate students are involved with teaching in the laboratory primarily as a means to develop their own pedagogical skills, rather than to compensate for decreased faculty availability. Graduate students are given the opportunity to work as paid tutors for medical students. These interactions have proven effective for both graduate and medical students. The graduate programs contribute to the overall mission by providing education to medical students as part of our tripartite mission. The opportunities for medical students and graduate students to interact include teaching laboratory and classroom settings, as well as medical student participation in research within a lab. The frequency of interactions varies depending on the context (e.g., a student doing research would interact daily with the graduate students.) The mechanisms in place for the review of the graduate programs include two interrelated activities. The first is on-site program review which occurs every seven years for each degree-granting program. The second is an outcomes assessment which is conducted on an ongoing basis. The outcomes assessment requires collection and analysis of data related to program. The self-study in the review process and the on-site review by the Review Committee allow each unit to review resources needed to accomplish the educational needs of their students. Action plans are formulated and provide the focus for the program chair and medical school administrators. 6. Evaluate the impact of residency training programs and continuing medical education activities on the education of medical students. Describe any anticipated changes in graduate medical education programs (numbers of residents shifts in sites used for training) that may affect the education of medical students. The impact of residency training programs has been widespread and truly positive. Many of the residents serve as teachers and are also able to give the medical students career advice. All programs recognize those residents who do outstanding teaching to medical students in their specialty-specific clerkship. During the awards ceremony each year the third and fourth year students recognize specific courses, clerkships, faculty and residents for their outstanding teaching. The graduate medical education programs equip residents as teachers through workshops and written guidelines. For example, Pediatrics has a dedicated resident for the students when they are in the clinics to help facilitate their learning and help the resident develop his/her own pedagogical skills. The impact of continuing medical education activities on the education of medical students has also been positive. Medical students may attend any continuing medical education activity. There may be a charge for regional conferences (to cover the cost of space, meals and printing). There is no charge for medical students at any outreach or in-house activity. Many clinical departments’ ongoing teaching series are part of their CME offerings. Departments that expect or require attendance at a CME regional conference pay the fee on the student’s behalf. Improvement plan: The graduate medical education program is in the process of developing several additional ACGME programs for consideration. These include a residency in vascular surgery and a sub-specialty program in endocrinology. If approved by the ACGME, these programs would enter their first trainees in 2011 or 2012. 5 7. Evaluate the research activities of the faculty as a whole, including areas of emphasis and level of commitment, quality, and quantity in the context of the school’s missions and goals. Note any limitations that may be affecting the research enterprise. Research activities for the faculty have increased and all priorities are related to the tripartite mission of the medical school. See (Fig. 1). There is a strong commitment to include medical students in research endeavors. From the AAMC Graduate Questionnaire, the number of students participating in research has fluctuated over the years but has remained greater than 50% since 2007-2008. Furthermore, the people of eastern North Carolina benefit from our research as described in the next paragraph. Each faculty member is committed to the medical school’s missions and goals. The quality and quantity of research is dependent on the department and the individual faculty member. Faculty members in different BSOM departments with common research interests meet regularly (e.g., Neurobiology Interest Group, Stem Cell Interest group). For the 2009-2010 academic year, East Carolina University reported an increase in external contracts and awards. The Center for Health Disparities Research is vital to the mission of ECU and aligns with the mission of the Brody School of Medicine. The Center facilitates and assists with research conducted at the University and with grant applications for university and community groups. 8. Assess the adequacy of the resources (equipment, space, graduate students) for research. Evaluate any trends in the amount of intramural support for research and the level of assistance available to faculty members in securing extramural support. The trends in the amount of extramural support have been increasing for the Brody School of Medicine despite the current economic times. Internal research seed grants are available through a variety of sources. The ECU Division of Research & Graduate Studies coordinates internal and external proposal reader pools in order to provide guidance and advice to faculty in the development of major grant applications. Some clinical departments offer small startup grants for research initiatives in the department. Grants are peer reviewed by senior faculty. Improvement plan: As we continue to recruit highly qualified faculty members who are expanding their research, the need for more equipment and space for research may become an issue. Currently Brody and East Carolina University have equipment sharing programs to enable better use of resources. 9. Assess the impact of research activities on the education of medical students, including the availability and ease of medical student access to opportunities for participation in research. 6 Research at the Brody School of Medicine has continued to flourish through the years as more faculty have gained international recognition. Faculty members include medical students as part of their research teams and as authors on manuscripts. Based on the AAMC Graduation Questionnaire we have seen the numbers of medical students who participated in research with faculty at the medical school increase from 35.7% in 2004-2005 to 51.6% in 2009-2010. Medical students gain both information from the research project itself and skills in research techniques. The opportunity for research has made our medical students more competitive applicants for residency programs. The availability of research has increased as medical school faculty members expand their research interests. Dr. Kori Brewer has increased the Summer Medical Student Research Scholars Program for first year medical students. Each student works with a faculty mentor performing research in the faculty member’s area of interest. Some students have had the opportunity to present at regional or national meetings. Each student receives a small stipend and must complete a poster and abstract at the end of the 8 week program. This program includes a small percentage of students and does not include students who individually seek out faculty mentors or those who do research at other institutions. 10. Describe programmatic and institutional goals for diversity. Evaluate the success of the medical school in achieving its goals for appropriate diversity among its students, faculty, and staff. Are there recruitment and support programs related to the school’s diversity goals and, if so, are these effective? Describe how well institutional diversity contributes to the educational environment and prepares students for meeting the health care needs of a diverse society. ECU’s Mission Statement states we aspire “to serve as a national model for public service and regional transformation by providing cultural enrichment and powerful inspiration as we work to sustain and improve quality of life.” The Dean has appointed Dr. Todd Savitt as Assistant Dean of Diversity Affairs with the responsibility to develop the Office of Diversity. He has gained input from the Brody community on the development of the diversity office and defining the needs of our faculty, staff, and students. Efforts to expand faculty and staff diversity are individualized with each department. The Brody School of Medicine recognizes the need for qualified applicants and has placed a Vice Chair of Diversity Initiative member to serve on search teams for faculty positions and major administrative appointments. After employment, minority faculty members are mentored through avenues like the INSPRE (Inclusion, Support, Professional development, Retention, Enrichment) program with a goal of retaining and professionally advancing talented minority faculty members. The Brody School of Medicine has consistently been able to recruit students with a diverse background representing 12% of the matriculates each year. The school provides recruitment and pipeline programs to engage underrepresented minorities and disadvantaged students. For instance, the Vice Chairs of Diversity Initiative, Brody Women Faculty Committee, and Academic Affairs provide financial and administrative support for the Summer Biomedical Research program for undergraduate students. Now in its fourth year, this summer opportunity encourages students to appreciate the Brody School of Medicine for post graduate work in research and the medical field. The Summer Program for Future Doctors continues to support at risk undergraduate students from underrepresented minority groups, as well as disadvantaged students. These programs have demonstrated great success in helping students improve study skills, learn basic science knowledge and successfully apply for professional school. For matriculating students, The Brody School of Medicine supports diversity efforts financially through several scholarly initiatives. The students elect a diversity representative for each class who 7 participates in the activities of the Vice Chairs of Diversity Initiative. These activities include organizing a Diversity Week and a variety of educational and informational programs each year. Furthermore, the Medical Student Council holds a Primary Care week, including a diversity day cosponsored by the American Medical Women's Association and the Student National Medical Association. The programmatic goals set each year by the various committees help to educate the Brody community. The programs are not only geared to the students but also faculty and staff. The numbers at these events have increased over the years and provide a better understanding of our diverse community. More recently, the graduating fourth year students went through a diversity exercise which included identifying barriers they met that dealt with diversity. The students rated the exercise 75% as excellent or good and 5% as poor. The students are constantly prepared to tackle diversity through their own reflections and continued care of the surrounding community in eastern North Carolina. Improvement Plan: We continue to work with our faculty and staff. The Office of Diversity at BSOM is integrating the efforts and goals of such groups as the Brody Women Faculty Committee, the Vice Chairs of Diversity Initiative, and the Student National Medical Association. II. Educational Program for the M.D. Degree A. Educational Objectives 1. Describe the level of understanding of the school-wide objectives for the educational program among administrators, faculty members, students, and others in the medical education community. Do these objectives serve as effective guides for educational program planning and for student and program evaluation? The current school-wide educational objectives were established initially in 2000 and reviewed most recently in 2008 as part of our ongoing curriculum renewal process. The objectives consist of four general attributes and 41 specific descriptors of those attributes; these may be reviewed at: http://www.ecu.edu/medicaleducation/edGoalsObjectives.cfm Specific surveys have been completed among course and clerkship directors concerning when/how these objectives are considered in course planning and content delivery. The most recent survey was completed in April 2010 with 100% participation by all course and clerkship directors. The survey results revealed that all objectives are covered multiple times during the four years of the curriculum. Students and faculty alike are made aware of these objectives: 1) through their availability online at the web site for the Office of Medical Education; 2) through periodic formal reviews of each course and clerkship, where specific attention is given to how each course/clerkship “links” their objective and assessment methods to the overall school-wide objectives; 3) through course/clerkship syllabi, where specific learning objectives are emphasized as part of orientation or otherwise at the beginning of each learning experience by students; 4) through posting within the online Blackboard course management system; 5) through periodic presentations to department chairs, course and clerkship directors and other leaders at the various curriculum committee and/or overall school faculty meetings; 6) to incoming medical students and resident physicians during group orientation sessions; and 7) to new incoming faculty at orientation sessions. 8 Overall, there is a good level of awareness and understanding of these objectives among the school’s leadership as well as faculty who lead courses/clerkships and, through them, faculty who teach our students across the curriculum. They are used extensively in educational program planning and indepth course review. They also serve as a basis for data collection purposes pertaining to program evaluation. Improvement plan: Our medical school depends on a large cadre of community-based affiliate faculty preceptors who teach our students across all four years of the curriculum. It is possible that many of these professionals may not be as familiar with the objectives as are campus based full time faculty. 2. Comment on the extent to which school-wide educational objectives are linked to physician competencies expected by the medical profession and the public. Summarize results from any associated outcome measures that demonstrate how well students are being prepared for the next stage of their training. Our process of adopting the school-wide educational objectives in 2000 was informed by a number of influential national efforts to link medical school training with “competencies expected by the medical profession and the public”. Chief among those was the Medical School Outcomes Project (MSOP), initiative sponsored by the AAMC. The content domains and clinical skills taught to and assessed in our students are also informed by national standards and discipline-based specialty recommendations. We have instituted a formal system for measuring/tracking educational outcomes that relate directly to our school-wide objectives. These outcomes are measured at the levels of student performance and at the program level. Student performance is measured using a variety of methods including student knowledge, performance in small group settings, clinical performance exams/OSCE procedures, professionalism ratings, personal observation of clinical and procedural skills, narrative essays, and simulation exercises. Program performance is measured using results of USMLE Step exams, residency program director surveys, student self-report of procedural skills competencies, the AAMC Graduation Questionnaire, and a number of other ways discussed in the LCME database (please see ED section of database, standards ED-1-A). Based on these data sets pertaining to educational outcomes, we are confident that we are producing high quality graduates who are ready to enter the next phase of their training. Improvement plan: Since an in-depth review of school-wide objectives has not been completed since 2000, the Executive Curriculum Committee has agreed to review them beginning in the fall of 2012. Many of our courses and clerkships have already revised their own objectives to reflect the “Six General Competency” approach; this framework will be prominent in our review. 3. Comment on the effectiveness of the system in place to ensure that all students encounter the specified types of patient/clinical conditions needed for the clinical objective to be met. Immediately after our most recent site visit in 2004-2005, we initiated a process whereby clinical faculty prepared formal criteria for each clinical rotation, in order to bring the school into full compliance with the requirements of ED-2 and linking our core rotation objectives to our school wide clinically-oriented objectives. These criteria are communicated to the students via clerkship rotation syllabi; students collect data in the form of patient logbooks to demonstrate that they are achieving the goals for each rotation. The mid-clerkship rotation feedback session is also designed to facilitate a conversation between each clerkship director and each student, so that accountability 9 on the part of students for meeting these criteria is maintained. The clerkship director reviews patient logbook data and is responsible for ensuring that all such criteria are met by every student. Students are required to turn in a completed logbook as a condition of receiving their final rotation grades. The Office of Medical Education supports this role by entering all data collected by students and furnishing annual data reports to each rotation director. Improvement plan: The logbook data collection and reporting function will soon be migrated from a paper based system to the E*Value online database system. This will facilitate more timely and accurate data collection as well as making the data available easily for formative review via the web. B. Structure of the Educational Program 4. Delineate the mechanisms in place to ensure that the educational program provides a general professional education that prepares students for all career options in medicine. Cite relevant outcomes indicating success in that preparation. Our school provides a structured educational program based on the 2+2 curriculum model. During the first two years, students receive the general foundation in basic sciences and also learn about behavioral and social sciences that are essential to medical practice. A prominent feature of the first two years is the longitudinal Doctoring course, which provides early clinical skills training, exposure to primary care, broad reinforcement of the biopsychosocial model of care, and extensive testing of basic medical interviewing and examination techniques. The third year provides training in seven core clerkships and allows a two week clinical elective which is used primarily for career exploration. During year four, students experience a combination of required rotations designed to complete their knowledge and skill bases while simultaneously providing them with career-oriented elective periods. Overall, we are confident that our curriculum structure facilitates the expected general preparation for students to pursue the next phase of their training and achieve the foundation necessary for success in any chosen field of medicine. Outcome indicators in support of this model include: 1) the afore-mentioned residency program director survey, which indicates that our graduates are well-prepared and performing well at the next training level; 2) successful match into residency programs of their choice; 3) results of student surveys that indicate overall satisfaction with general preparation and specific services focused on career choices (e.g., AAMC’s Careers in Medicine program, our career advising services including the Career Tasters seminar series); and 4) student performance on the USMLE Step exams. Improvement plan: Students perform at a lower than desirable level on M3 clerkship NBME subject exams and the USMLE Step 2 CK exam. Better performance on these exams is an area of targeted improvement for our school. 5. Evaluate the adequacy of instructional opportunities for students to engage in active learning and independent study. Assess the effectiveness of the program’s efforts to prepare students to engage in self-assessment of their learning needs and to develop other skills to support habits of lifelong learning. The overall philosophy of our school is to use a variety of teaching methods in order to appeal to the learning styles of all students, while simultaneously presenting the required curriculum content on multiple occasions. The curriculum encourages active learning by use of a variety of instructional methods including guided discussions in small groups, laboratory sessions, team-based learning (TBL), case-based seminars, journal clubs, interactive sessions with real and/or standardized patients, and patient care activities using the traditional rounding and case presentation methods. 10 Approximately 22% of our total instructional hours in the M1 and M2 years take place within the small group context where active learning is emphasized. Independent study is also encouraged across all four curricular years. The average number of student contact hours is 24.3 in the fall and 25.6 in the spring semester of the M1 year, and 26.6 in the fall and 23.1 in the spring semester of the M2 year. This average is based on the total student contact over the semester, including examination weeks (when no classes are scheduled). Remaining time is available for active learning; students are strongly encouraged to make the most effective use of this time. Refining the student's ability to assess their own learning needs begins at M1 orientation with an inventory designed to allow the students to identify their preferred learning style (e.g., auditory, visual, collaborative, or individual). In particular, there is heavy emphasis across the first two years on assisting students with better understanding how they learn and how to adapt their particular learning preferences or styles to the demands of the curriculum. The M3 clerkships require practice OSCE review sessions and/or oral exam procedures, both of which are designed to provide students with formative feedback and to assist them in refining their learning on an ongoing basis. In sum, there are planned experiences across the entire curriculum that provide students with ample opportunities to assess their own learning needs as well as their performance. Improvement plan: Ongoing curriculum monitoring of lecture hours in the M1 and M2 years will present an opportunity to further streamline and refine the curriculum. Total lecture hours, particularly in the M2 year, remain greater than 25 hours a week. Consideration should be given to reducing lecture hours wherever possible, in favor of more independent study time. 6. Evaluate the adequacy of the system for ensuring consistency of educational quality and of student assessment when students learn at alternative sites within a course or clerkship. Three of seven M3 core clerkships (Family Medicine, Pediatrics and Psychiatry) use a distributed educational model whereby students rotate for a significant portion of their training at external affiliated campus locations. These rotations inform their off-site faculty members of educational objectives and grading methods through rotation orientation sessions, faculty meetings, the use of the Blackboard course management system, electronic mail communications, and individual meetings. Communication is emphasized throughout, but specific processes used vary somewhat across these three clerkships. Written communication occurs before and after each cohort group rotates, wherein affiliate community-based faculty are provided with rotation objectives and grading forms. Informal consultations via telephone and/or email messaging also occur routinely. Clerkship directors meet regularly with students about the off-campus portions of their experiences and respond to student concerns rapidly. Student Affairs Deans also respond to specific issues in this regard. Data collected by students regarding the types of patients seen (e.g., via ED-2 requirements) indicate consistency across sites, and there is evidence that students gain in-depth 11 clinical experience at some of the off-site rotation locations. Student ratings of clerkships do not indicate concern with community site experiences and they rate the one-on-one relationship with their preceptors highly. Improvement plan: In spite of challenges pertaining to having adequate time, clerkship directors must meet in person more frequently with community preceptors at their off-site locations. Formal studies of student knowledge and clinical performance using “training location” as a variable should be considered. 7. Comment on how well all content areas required for accreditation are addressed in the curriculum. How confident is the educational program leadership that these topics are appropriately addressed? School leaders are confident that all content areas required for accreditation are addressed in our curriculum. Data from the former CurrMIT database, course/clerkship syllabi, our ongoing survey of residency program directors, and the AAMC Graduation Questionnaire confirm that content areas are adequately addressed. Scores on internal assessments (written and clinical performance), NBME Subject examinations (pre-clerkship and clerkship), and the USMLE Steps 1 and 2 CK examinations are benchmarks to assure that required material is adequately covered and that students are provided with appropriate opportunities and guidance for mastering material. Faculty members also recognize that content is evolving and the curriculum cannot remain static. Issues such as patient safety, quality of care, global health and medical informatics are increasingly part of modern health care. The ongoing challenge is to find the appropriate balance between various content areas in terms of breadth and depth of coverage. 8. Assess the balance between inpatient and ambulatory teaching and the appropriateness of the teaching sites used for required clinical experiences. We feel that this is a definite strength of our curriculum. The approximate overall ratio of inpatient versus ambulatory patient encounters is 60% outpatient and 40% inpatient. All of the required clinical rotations provide ambulatory learning experiences and provide an approximately equal balance between learning in the inpatient versus outpatient settings. Because of our primary care mission, there is an additional 4 week requirement for primary care that all M4 students must complete. The selective choices to satisfy this requirement are predominantly outpatient in nature. Our strong and long-standing relationship with our teaching hospital and the affiliate clinical faculty in our region translate into outstanding educational experiences in the realm of clinical instruction. Over the past three years, we have put additional effort into recruiting alumni of BSOM to assist in precepting students and resident physicians in community settings, with very positive results. The effectiveness of our clinical educational model is confirmed by student feedback surveys, both internal and as expressed on the AAMC Graduation Questionnaire. C. Teaching and Evaluation 9. Comment on the adequacy of the supervision of medical students during required clinical experiences. Discuss the effectiveness of efforts to ensure that all individuals who participate in teaching, including resident physicians, graduate students, and volunteer faculty members are prepared for their responsibilities in medical student teaching and assessment. During required clinical experiences, our students learn primarily through either direct one-on-one relationship with faculty members who are practicing physicians or via assignment to a more 12 traditional learning team. Each rotation director is responsible for assigning faculty to each student and each student to teams that are well supervised. All clinical faculty members are strongly encouraged to seek appropriate training in clinical teaching, student evaluation, and clerkship objectives prior to being assigned to teaching students. Faculty members are also instructed on supervisory responsibilities directly by their Clerkship Directors and through faculty development programs. In response to survey items on the AAMC Graduation Questionnaire (e.g., “A faculty member personally observed me taking a patient history during the clerkship”, “Performing a physical examination during the clerkship”, "Faculty members provided me with sufficient feedback on my performance"), we note that our students do not report serious concerns about this area. Preparation of resident physicians, graduate students and volunteer faculty members for their teaching roles is primarily a departmental function. Student feedback from various surveys does not indicate a concern in this regard. However, we have identified this particular area as one that could be improved by monitoring the familiarity of resident physician and volunteer faculty (at least in certain disciplines) with institutional educational objectives. More recently, the Office of Graduate Medical Education has instituted a formal presentation on “Residents as Teachers” that is required of all new incoming residents at our teaching hospital (see LCME ED-24 section of the database). Improvement plan: Institute an enhanced centralized monitoring system during the 2011-2012 academic year, to ensure that all resident physicians and affiliate community faculty are fully aware of institutional educational objectives. 10. Evaluate the adequacy of the methods used to assess student attainment of the objectives of the educational program. Comment on the appropriateness of the mix of testing and evaluation methods. Describe the frequency with which students receive formative assessment in addition to summative evaluations. Discuss the timeliness of performance feedback to students in the preclinical and clinical years. In addition to approximately four written block exams per semester in year one and three per semester in year two, the BSOM uses a number of formative and summative internal and external measures to evaluate attainment of its educational program objectives. An important internal process used to assess our students' knowledge and clinical skills is a multi-facet clinical skills assessment program, which uses OSCEs and standardized patient exams across all four years of the curriculum. Students who do not perform at the appropriate level on these evaluations are provided individual remediation. Students’ participation in small group sessions, encounters with standardized patients and simulators, and clinical performance in the community-based M1 and M2 preceptorship program and on M3 and M4 clerkships are all components of the overall assessment of our students. We also instituted a new emphasis on procedural skills and are carefully tracking performance as self-reported by M4 students each spring. The trend of self-reported exposure to and competence with core procedural skills is positive. Important external measures include students’ performance on NBME Subject and USMLE Step examinations and data received from residency program directors’ surveys each year. Timely summative and formative feedback to the student is an explicit requirement for all clinical rotations/clerkships. Exam scores are communicated in most courses within a 48 hour period. Course grades must be submitted within one week after the course's final examination or according to established school guidelines. Clerkship grades must be submitted within six weeks of the end of the clerkship. 13 Improvement plan: Our self-study revealed that certain clerkships did not comply with the school requirement to turn in official grades within the expected six week time frame. We are instituting enhanced tracking mechanisms that will boost the timeliness of these grade reporting procedures. 11. Describe the system for ensuring that students have acquired the core clinical skills specified in the school’s educational program objectives. Evaluate the frequency with which students are observed and receive feedback on their clinical skills. Are there any limitations in the school’s ability to ensure that the clinical skills of all students are appropriately assessed? There do not appear to be any limitations in our ability to ensure that the clinical skills of our students are assessed. Students are very closely monitored on a daily basis during all clinical rotations. The teaching and assessment of students’ clinical skills has been a prominent feature of the curriculum at our school for many years. This teaching and assessment begins from day one with the longitudinal Doctoring course that runs the entire first two years of the curriculum. For M3 and M4 students, clinical skills are assessed in numerous settings by use of a variety of methods including NBME subject examinations, direct observation, performance ratings, simulation exercises, standardized patient interactions, and videotaped instructional sessions. Students work closely with attending faculty members and resident physicians who observe these skills. Required clinical rotations provide mid-rotation feedback and proactively address any presenting issues or concerns. The close faculty to student ratio ensures that this feedback is meaningful. All students undergo standardized patient exams while on each of the M3 core clerkships, and a cumulative exam of this nature occurs at the end of the M3 year. The M1, M2 and M3 Student Promotion & Review Committees meet several times each year to review the individual performance of students. Finally, our residency program director survey data indicates that our graduates are well-prepared in regard to these clinical skills. D. Curriculum Management 12. Assess the adequacy of the system for managing the curriculum and ensuring that it is coherent and coordinated. Do the curriculum as a whole and its component parts undergo regular, systematic review? Describe the procedures in place to identify and rectify any problems in the curriculum as a whole and in individual courses and clerkships. Evaluate the effectiveness of these procedures, and provide specific illustrative examples. Provide evidence that the school monitors the content covered in the curriculum to ensure that all desired content is covered, that gaps or unwanted redundancies do not occur, and that there is appropriate horizontal and vertical integration among content areas. The Senior Associate Dean for Academic Affairs (SADAA) has delegated authority from the Dean of the school to ensure that all curriculum management systems are functioning effectively. Much effort has taken place in this regard since our previous site visit in 2004, including the creation of new Associate & Assistant Dean positions related to curriculum, implementation of new staff support procedures, increased communication across the entire faculty pertaining to the curriculum, and initiation of an in-depth course & clerkship review system. These components of curriculum management have been effective across the board. For example, our new course/clerkship review system (whereby every course across all four years is reviewed in depth by an ad hoc review team) has proven to be a valuable tool in diagnosing educational issues and suggesting peer-driven remedies. The identification of curriculum gaps and/or un-necessary redundancies has proven to be more challenging, but significant progress has been made. Course directors across the M1 and M2 years continue to address integration issues regularly, as evidenced by an integrated testing approach used 14 during M2 Pathology, Introduction to Clinical Medicine and Pharmacology, and by the use of curricular content themes (or “threads”) pertaining to selected topics. Further efforts lie ahead in terms of finalizing our total efforts of effective integration, particularly with regard to further reemphasis of basic science content in the clinical years of the curriculum. We must also address student concerns pertaining to selected content areas that may be over-represented in the curriculum, while simultaneously creating more curriculum content in new or evolving areas. Improvement plan: As previously stated, full implementation of the new E*Value curriculum management project and final implementation of all curriculum renewal activities (as detailed in section ED-9 of the LCME database) will further strengthen our overall efforts in this area. 13. Does the chief academic officer have sufficient resources and authority to ensure that the educational program can achieve institutional goals and learning objectives? The Senior Associate Dean for Academic Affairs (SADAA) serves as the Chief Academic Officer and has sufficient resources and authority delegated by the Dean. It is expected that the SADAA actively participate in setting the budgets for the Division of Academic Affairs and its various operational units. S/he works closely with the Dean, the Curriculum Committees, the Brody Council and the Department Chairs to ensure that sufficient numbers and types of faculty members are available to implement the educational program. S/he is also an effective advocate for our educational mission in a variety of administrative meetings across the entire University. Resources for the educational mission of the School are adequate at the present time. In recent years, the economic climate within our state, as in most other places in the US, has required significant adjustments designed to maximize the effectiveness of available resources for education. In North Carolina, state tax revenues have been shrinking and the school is actively engaged in pursuit of non-traditional forms of revenue to support education. Operating revenues appear to be sufficient, but expansion plans as well as facilities upgrades are currently on hold. Improvement plan: The School is considering a more formal process of allocating funding for education based on formula-driven procedures. There is concern about this issue among faculty members and course/clerkship directors, who may experience tension concerning time constraints impacting education. 14. Assess the effectiveness of curriculum planning in the medical education program. Describe efforts to ensure that there is appropriate participation in planning and that resources needed to implement the plans will be available. Overall, the curriculum planning process at our school is thorough and benefits from strong faculty leadership. Our curriculum governance structure ensures that a variety of constituent groups (e.g., faculty, students, and administration) have significant opportunity to participate in planning, implementing and evaluating the curriculum. Overall internal communication about curriculum matters has increased significantly since our previous site visit in 2004, primarily due to increasingly robust reporting of educational outcomes as well as better information flow between various curriculum committees. A school wide curriculum retreat was held in 2006 for the first time in many years, and subsequent “mini-retreats” on specific topics have taken place as needed. Resources for curriculum plans are made available both centrally and via the departments. State allocations for education are jointly controlled by departments and central administration. Practice plan resources for specific educational purposes continue to subsidize education in a significant manner, but have been increasingly constrained in recent years. 15 When a new plan is put forth for a specific educational project, conversations about resources occur between the Dean’s office, Academic Affairs personnel, department chairs and course/clerkship directors. This system works well and results in a very high degree of communication about educational issues. External and internal funding sources may also be sought for specific purposes, with the school benefitting from several education-related grants in recent years. Improvement plan: A more formalized process for allocating resources specifically to education is being considered. Structurally, consideration about operations of selected resources for education (e.g., simulation activities, clinical skills assessment programs) is an ongoing item of discussion. 15. How does the curriculum committee ensure that students have sufficient time for learning? Evaluate the educational workload and the balance between education and service in the clinical years. Assess the effectiveness of the mechanisms used to monitor student duty hours. Do students receive sufficient formal teaching during their clinical clerkships? The year curriculum committees actively monitor students’ schedules, the frequency of exams and overall workload. For M1 and M2 students, the capture of all lectures and other large group didactic presentations via video recordings demonstrates additional learning experiences and this system is utilized to supplement live instruction and enhance the efficiency with which students learn the required material. In the clinical years, the school has adopted the ACGME duty hour rules for guiding student work hours. We actively monitor developments regarding ACGME duty hour policies and make whatever adjustments are deemed best for the students. This policy is communicated to the students during the orientation session of each clerkship and other core rotations, as well as during large group orientations to the M3 and M4 years. Students report no issues with clinical duty hours, which are actively monitored by each clinical rotation director. 16. For schools that operate geographically separate campuses, evaluate the effectiveness of mechanisms to ensure that educational quality, curricular content, and student services are consistent across areas. In order to determine the comparability of teaching and student assessment across campuses, review patterns of grades and indicators of student performance and satisfaction. The Brody School of Medicine does not currently have geographically separate campuses. E. Evaluation of Program Effectiveness 17. Describe the evidence indicating that institutional objectives are being achieved by enrolled students. Our school uses a variety of educational outcome measures to determine whether our objectives are being met effectively. These are fully detailed in section ED-46 of the LCME database. A formal process for ensuring that all BSOM school-wide objectives are taught within the entire curriculum has been completed twice since the last LCME site visit. This process helps assign responsibility for the objectives and supports the fact that all objectives are being achieved. The most recent results from this survey (completed in April of 2010) shows that all of the objectives are addressed within multiple courses across the four year curriculum. Evidence that the educational program objectives of the Brody School of Medicine are being 16 achieved is provided to varying degrees by a number of indicators or instruments. 1. The “ultimate” USMLE pass rate is high, with an improving for first time takers. In addition, for the 2009-2010 and 2010-11 academic years, our first time takers of USMLE Step One scored above the national mean on the total test score. 2. Students achieve standards set by the faculty for internally developed multiple choice exams (primarily focusing on knowledge) and performance-based exams (primarily focusing on skills and behaviors). Individual student and class cohort performance is tracked as students/classes progress through the educational program. 3. Responses on the AAMC Graduation Questionnaire relating to our school wide objectives, in the vast majority of areas, are at or above the national norm. 4. Student feedback indicates overall satisfaction with the vast majority of courses and clerkships. 5. Student advancement and graduation rates have shown improvement, especially within the last four years. For instance, the number of students who are in extended programs for academic reasons has decreased from a range of four to seven per class to zero to three per class. 6. As noted above, data from a newly-established annual survey of residency program directors have provided valuable information indicating that we are producing well-trained graduates who are ready to proceed to residency training. 18. Discuss how information about enrolled students and graduates is used to evaluate and improve the medical education program. Use of the information previously listed is primarily the responsibility of faculty course/clerkship directors, curriculum committees and administrative personnel. Protocols for regular review of outcomes data are in place, and discussion is held in a variety of departmental and school-wide forums on any problem areas identified. As an example of how this process works, an item on the residency program director survey indicated that our students were initially rated lower than expected on their procedural skills competency. This information was subsequently used by the M3, M4 and Executive Curriculum committees to 1) appoint an ad hoc task force to study the issue; 2) create a proposed new procedural skills curriculum with assigned teaching responsibilities per clinical course & clerkship; 3) consider and implement a newly required M4 rotation in Emergency Medicine with an emphasis on procedures; 4) implement an expanded simulation training program within the M3 and M4 curricular years; and 5) implement a new survey of graduating medical students concerning their perceived competence in these procedural skills and suggestions for training improvements. This is an ongoing process. III. Medical Students A. Admissions 1. Critically review the process of recruitment and selection of medical students, and evaluate the results of that process. Is the size of the applicant pool appropriate for the established class size, both in terms of number and quality? How are the medical educational program’s selection criteria validated in the context of its mission and other mandates? 17 The Brody School of Medicine recruits and selects students who are North Carolina residents and who have characteristics and traits that are consistent with the tripartite mission of the school. The Associate Dean of Admissions recruits intensely from the colleges and universities located in North Carolina and has programs in place to enhance recruitment from Historically Black Colleges and Universities (HBCUs) in North Carolina as well as UNC Pembroke (an eastern North Carolina university that has a relatively high minority enrollment, including Native Americans). The efforts of the Admissions Office include hosting an annual conference for all NC college pre-medical advisors and encouraging the attendance of individuals from HBCUs, contacting premedical advisors twice per year and visiting numerous NC campuses each year. The ECU Early Assurance Program recently expanded to UNC Pembroke, NC A&T University and Bennett College, serves to enhance recruitment of students likely to be strongly recruited nationally. In 2006, a task force assessing the school’s readiness for expansion of the medical student class size evaluated numerous issues including the pool of NC applicants and determined that current resources, limited primarily by the physical plant, could accommodate up to 80 students in the entering class and that with expansion of the teaching facilities locally and the addition of new clinical training sites the class could be expanded to approximately 120. Since 2006, the size of the entering class has gradually increased from 72 to the current 78. The table below illustrates the stability of the size of the pool for the classes entering from 2003 through 2011: 2003 2004 2005 2006 2007 2008 2009 2010 2011 NC apps 671 705 745 768 815 878 879 918 851 Interviews 453 452 432 450 393 454 505 506 488 As reflected in Section III, Part A, the mean MCAT scores and mean overall GPAs for the matriculating students over the time period from 2004-2005 through 2010-2011 have increased. It is clear that the pool of NC applicants is sufficient in size and strength to allow us to continue to limit admissions to this group. We believe that this is important for the continued success of the school in educating students who will ultimately practice medicine in North Carolina. The students matriculating at BSOM also create success in the other areas of the mission. In its 2011 Mission Management Tool, the AAMC lists BSOM in the highest ranking of schools in the following categories: Percentage of graduates from 1996-2000 practicing in rural areas; Percentage of graduates from 1996-2000 practicing in underserved areas; Percentage of graduates from 2007-2009 entering family medicine; Percentage of graduates from 2004-2009 who are American Indian or Native American; and Percentage of graduates from 2004-2009 who are black or African-American. The Brody School of Medicine at East Carolina University is one of top medical schools in the country for sending graduates into family medicine, according to the American Academy of Family Physicians. Based on a three-year average for the period ending October, 2010, 18.9 percent of the school’s graduates have entered an accredited family medicine residency program. That ranked 18 BSOM second in the country and marked the fifth consecutive year ECU has been ranked in the top 10. According to a report in the magazine U.S. News & World Report (April, 2011), BSOM ranks 10th overall among primary care schools. Between 2008 and 2010, BSOM sent the seventh-highest percentage (54.3%) of its graduates into primary care residencies. U.S. News defined primary care residencies as family medicine, pediatrics and internal medicine. In the most recent match (March, 2011), 19 percent of Brody's graduating students matched with family medicine residency programs during the school’s annual Match Day. Also in March, a study by the American Academy for Family Physicians showed ECU topped the nation in producing family doctors from 1999-2009. During that span, ECU sent 19.5 percent of its graduates into family medicine residencies. According to the AAFP, the national average is 9.6 percent. Improvement plan: In 2006, the AAMC initiated a call for the expansion of medical schools across the United States. The planned expansions of BSOM and UNC School of Medicine coupled with the addition of new allopathic and osteopathic schools in the region could impact the ability of BSOM to continue to restrict admission only to NC residents. Consideration of expansion of the applicant pool to include regional students (VA, SC) may be warranted. The 2006 task force also suggested that some expansion slots be reserved for a nationally recruited MD/PhD pool. 2. Evaluate the number of students of all types (e.g., medical students, residents, visiting medical students, graduate students in basic sciences) in relation to the constellation of resources available for teaching (e.g., number of faculty members, space, clinical facilities, patients, educational resources, student services). 2003-2004 Entering class size 2009-2010 72 78 Total enrollment 304 306 Residents and fellows 274 342 70 86 300 333 Full-time basic science faculty Full-time clinical faculty The doctoral programs housed within BSOM enrolled a total of 61 students in 2003-2004 and 64 students in 2009-2010 (62 in 2010-2011). Since the last LCME accreditation, the impact of these learners upon the medical students has decreased. Historically many doctoral students were enrolled in the same basic science classes as medical students. Over the past decade the needs of the two populations of students have diverged significantly resulting in lower Ph.D. student enrollment in medical courses. The new 2011 MS program in Biomedical Sciences will involve a small number of faculty in the basic science and clinical departments of BSOM. No impact upon medical students and their education is anticipated from implementation of this program. Space allocated for education of medical students in the Brody Medical Sciences building and Pitt County Memorial Hospital (now called University Health Systems Medical Center) is sufficient but 19 operating at near capacity. A careful assessment of available teaching space in terms of classrooms, small group rooms, teaching laboratories and associated spaces, like lounge space and call rooms, was made by the Task Force for Class Enhancement in 2006 (Section III Appendix ?). The current size of the entering class was determined to be appropriate for current educational resources. Improvement plan: The East Carolina School of Dental Medicine opened with an inaugural class of 52 students in Fall Semester, 2011. The presentation of the basic science portions of its integrated curriculum will be through a partnership with the Brody School of Medicine. Ample resources have been transferred to BSOM for the development and presentation of the curriculum however there will be lag time in hiring and preparing new faculty to assist with the program. The initial offerings of this program have the potential to place strain on the teaching time of senior basic science educators of BSOM. Until the opening of Ross Hall, home of the School of Dental Medicine in 2012, space for the D1 students’ lecture hall and simulation lab is being provided in the Brody Medical Science Building. The space to be used has been carefully planned and renovated and should have minimal impact upon our medical students. 3. Describe the school’s successes in broadening diversity among medical school applicants. How well are the school’s programs to enhance the diversity of the medical school applicant pool functioning? How effective are the school’s efforts to track pipeline program graduates? Because of its mission, BSOM has always fostered diversity in the student population. The original legislated charge that “special efforts be taken to encourage the recruitment and medical education of racial minorities” (Chapter 1190, page 312, Sessions Laws 1973, NC General Assembly) has evolved so that the Admissions Committee strives for the recruitment of a class that is diverse with respect to race, color, creed, national origin, sex, sexual orientation, age and other attributes. The 2004 LCME Letter of Accreditation stated that our student body was noteworthy for its demographic diversity. As presented in A.1 above, BSOM continues to excel in the recruitment, retention and graduation of a diverse student body. Based upon ethnicity, a current snapshot of the student body is presented below: Category First-Year Students All Students Hispanic/Latino 3.5 3.6 Black or African American 17.7 12.9 White 63.5 69.2 American Indian 3.5 2.3 Asian 9.4 10.4 Native Hawaiian or Pacific 0 0 20 Islander Two or more races 2.4 1.6 Total 100 100 The pre-matriculation component of the BSOM Summer Program for Future Doctors which focuses upon the development of students aspiring to attend medical school is also mission-driven; the program gives preference to under-represented minorities, socioeconomically disadvantaged and non-traditional students. Students who perform well in this program have a high probability of matriculation at BSOM or other medical schools. BSOM is also committed to success in providing access to medical education for NC residents from all socioeconomic backgrounds. Even in this time of economic difficulty for NC, BSOM continues to charge the lowest tuition of all US medical schools and our graduates have the lowest average debt upon graduation. A student initiative sponsored by Student National Medical Association with faculty support actively recruits peer students during an annual pre-med conference for minority and underserved college students, advisors, high school students and their parents. 4. Evaluate whether the acceptance of transfer students, or visiting students in the school’s affiliated teaching hospitals, affects the educational program of regular students. Historically, BSOM has accepted very few transfer students (currently none are enrolled) and they have had no measurable impact upon resources. Visiting students are granted acceptance to rotations here only after our own students have filled their schedules thereby eliminating the impact of visiting students as well. B. Student Services 5. Comment on the levels of student attrition and academic difficulty in relation to the medical education program’s admission requirements, academic counseling efforts, and remediation programs. Evaluate the efficacy of the program’s system for early identification and remediation of students in academic difficulty. Describe the counseling and remediation systems that are in place, and assess their effectiveness. The overall student attrition rate is low. Retention data for the time period 1994-2009 reveals the following: 1. African American Students: 94.4 % of the matriculating students completed or are still progressing through the program. Average loss is less than one student per year with no losses for nine years. 2. Other Students: 97.5 % of the matriculating students completed or are still progressing through the program. Average loss is less than one student per year with no losses for four years. The first semester of the M1 year presents the greatest challenge to students in terms of academic difficulty. Remediation and/or Leaves of Absence for academic difficulty combined with academic counseling through the Office of Medical Education and Student Development (OMESD) (formally Academic Support and Counseling Services) has proven to be effective in such cases. Timely review 21 of student performance by the Promotion and Review Committees for each of the academic years has effectively identified students experiencing difficulties and has effectively students to appropriate resources. The new Academic Achievement Program, placed in effect in July, 2011 by the Executive Curriculum Committee, is designed to enhance our ability to identify students early who are experiencing academic difficulty and to provide them with a formal structure ensuring that they will access and use the resources available to them. The Program includes official criteria for “academic difficulty” in the M1 and M2 years and separately for the M3 and M4 years, along with directed assistance for students who meet these criteria. 6. In the context of data from the student independent analysis and data from the most recent AAMC Medical School Graduation Questionnaire, evaluate the effectiveness of the systems in place for career counseling, residency preparation, and the selection of elective courses. The student independent analysis cites the availability and awareness of career and residency counseling (Question 8) as an area of concern. In their analysis, it is stated that the Class of 2014 ranks this question with the highest percentage of “Excellent” (26% vs. 23% across all classes) or “Good” (44% vs. 37% across all classes) and their interpretation is that progress is being made in this area. The overall satisfaction with career planning services expressed by the graduating class of 2010 in the 2010 Medical School Graduation Questionnaire has a mean rating of 3.7 vs. a rating for all schools of 3.6 (on a 5 point Likert scale) and no graduate indicated that they were “Very Dissatisfied” compared to 4.5% from all schools. Both data sets indicate a positive trend in this service. It is anticipated that implementation of the newly required “Pirate MD” course in 2011 will greatly improve career counseling for our students. This course will launch initially with content for the M1 and M2 years and will expand to include all years of the curriculum as these classes advance. The Assistant Dean for Student Affairs responsible for the clinical years provides oversight and guidance to students choosing electives during the M4 year. With the exception of 2009, the graduating classes of 2006 through 2010 rated the statement “I received appropriate guidance in the selection of electives” more favorably than students at all schools. For the class of 2010, 67.2% either chose “Agree” or “Strongly Agree” whereas 57.3% chose those ratings for all schools. The process that is in place now is working well but will face challenges with future class expansion. It is anticipated that the “Pirate MD” course will foster improvement in this area as well as for career counseling 7. Evaluate the level of tuition and fees in relation to the amount of graduates’ accumulated debt and to the level of financial aid needed and available. Describe the efforts in place to minimize medical student indebtedness and comment on the effectiveness of these efforts. Describe the adequacy and availability of financial education and debt management programs. Throughout its history, the Brody School of Medicine has consistently been able to charge students less in tuition and student fees than any other accredited US medical school. According to the AAMC Student Tuition and Fees Reports this continues to be the case for the reporting year and for 2010-11. The average debt of BSOM graduates has increased from $63,400 in 2005 to $92,416 in 2011. While the debt load of BSOM students is relatively modest, current students express some concern with the adequacy of debt management counseling (question 11 of the student independent analysis). According to their survey, 56% of the student respondents rated the adequacy of debt management counseling as “Excellent” or “Good” and 14% rated it as “Fair” or “Poor”. Data presented in the AAMC 2011 Medical School Graduation Questionnaire indicate that BSOM just met the national level in meeting the needs of graduates in debt management counseling. For 22 graduating classes from 2007 through 2011, the average Likert score for BSOM graduates range from 2.8 to 3.7 compared to the mean score for all schools of 3.7. This is an area to monitor. According to data reported in the 2009-2010 LCME Part I-B Student Financial Aid Questionnaire, BSOM students received approximately $1.17M in grants and scholarships and $5.54M in loans for that academic year. East Carolina University has embarked on a major philanthropic effort, dubbed the Second Century Campaign, which will add funds for scholarships across the University. Approximately $22-23M of the $186M raised to date has been designated for scholarships and approximately $24M has been designated to provide funding for the Medical & Health Sciences Foundation for several purposes. 8. Evaluate the adequacy and availability of student support in the following areas: a. Personal counseling and mental health services, including their confidentiality and accessibility. b. Preventive and therapeutic health services, including immunizations and health and disability insurance. c. Education of students about bodily fluid exposure, needlestick policies, and other infectious and environmental hazards associated with learning in a patient care setting Personal counseling and mental health services are available through a variety of opportunities. Venues include the Office of Medical Education and Student Development, the ECU Counseling and Student Development Center, ECU Psychiatry and outside of ECU, the Carolina Centre. The Carolina Centre is a community resource providing psychotherapy and psychological testing services. These services are funded by the medical school. As of July, 2011 all psychiatric services will be provided by BSOM’s Department of Psychiatric Medicine. The Carolina Center will continue to see students already under their care. Accessibility and confidentiality are of highest priority as this change occurs. Students also have a variety of venues available for preventive and therapeutic health services. These include BSOM facilities (Family Practice Center, Pediatric Outpatient Center, Brody Outpatient Center), ECU Student Health Service (primary care center supported by student fees), Carolina Centre and the ECU Psychiatric Outpatient Center. For the 5 years presented in the 2011 AAMC Medical Student Graduation Questionnaire the average rating on the question concerned with their satisfaction with student health services varied from a low of 3.1 to a high of 3.9 (on a 5 point Likert scale). The mean score for all schools for the class of 2011 is 3.8. In the independent student analysis, 55% of students indicated that the adequacy of student health services is “Excellent” or “Good” and 12% said “Fair” or “Poor”. It appears that BSOM students are reasonably satisfied with the availability of health services. Graduates express less satisfaction with the health insurance plan that is provided for them. For the same population of graduates, the mean rating for the student health insurance varies from 2.7 to 3.5 and the 2010 mean for all schools is 3.2. The most recent graduating class was above the mean for all schools. This is an area deserving continued attention. All students are required to attend Blood Borne Pathogen training annually during orientation. This training includes directions on the procedures to follow in the event of an exposure. Visiting students are required to present evidence of blood-borne pathogen training prior to acceptance. The independent student analysis reveals that an average of 66% of students in the classes of 2011 23 through 2014 rate the adequacy of their education about prevention and exposure to infectious disease has been “Excellent” or “Good” and 8% rate is as “Fair” or “Poor”. C. The Learning Environment 9. How effective are the medical education program and its clinical partners in ensuring an appropriate learning environment for medical students? Summarize successes and challenges in evaluating the learning environment to support positive and mitigate negative influences on student’ acquisition of defined professional attributes. A task force appointed by the Executive Curriculum Committee was charged with defining what is meant by “medical professionalism” and what steps could be taken to improve the overall professionalism and learning environment of BSOM. This group submitted its report in May, 2006. Since that time professionalism and the learning environment has been a major focus of the administration and the faculty. Desired professional attributes are taught both formally and informally across all years of the curriculum. M1 and M2 students are informally assessed by faculty members. During 2009-2010 all M3 students in Psychiatry were assessed using a ratings instrument based upon the adopted attributes of professionalism. Because of the positive results from that pilot testing, all required M3 and M4 clerkships now use this ratings instrument (since July 1, 2010). Effective with the 2009-2010 academic year, a new item was added to the ratings form used by students to provide feedback on courses and clerkships. As assessed during that year, an average of 79% of M1 and M2 students either agreed or strongly agreed with the statement “This course promoted a positive learning environment”. An average of 89% of M3 and M4 students agreed or strongly agreed with the statement “The learning environment of this course encouraged professional attitudes & behaviors among students”. Also effective with the 2009-2010 year, a new item was added to the ratings forms used by students to provide feedback to individual teaching faculty members: “The faculty member is a positive professional role model for students”. The success of our efforts to promote professionalism is also seen in data generated by an annual survey of residency directors for the members of the preceding year’s graduating class. With response rates of 80% to 95%, BSOM graduates are rated highly on item related to their professionalism. Improvement plan: Challenges facing the school in this area include assessing the professional attributes of M1 and M2 students. This is discussed at the level of the M1 and M2 curriculum committees but has yet to produce an instrument that will foster the effective monitoring of professional development in the preclinical years. Also, based in part upon the data in the AAMC 2010 Medical School Questionnaire, the education of residents as teachers and their development as role models of the desired professional attributes deserves continued attention. 10. Citing data from the independent student analysis and the AAMC Medical School Graduation Questionnaire, comment on the effectiveness of school policies for addressing allegations of student mistreatment and for educating the academic community about acceptable standards of conduct in the teacher-learner relationship. Student awareness of our policy addressing student mistreatment has risen to a level that consistently places BSOM ahead of the national level. Similarly, the percentage of students reporting an incident of mistreatment has decreased since the last accreditation site visit. Questions 30 and 31 of the independent student analysis address the students’ awareness of policies for preventing student mistreatment and the adequacy of policies for preventing student 24 mistreatment. Across all classes, 67% if the responding students answered “Excellent” or “Good” to each of the questions. The Class of 2014 had the highest number of respondents to both questions and 74% answered with “Excellent” or “Good” to each question. The trends have been favorable both for student awareness of the policy and for reports of mistreatment. This has been an area of focus since the last accreditation review. Although even one report of mistreatment of a student is too many, the percentage of BSOM students from the Class of 2010 reporting mistreatment was less than 50% of the national percentage. Improvement plan: Even though the numbers of incidents are relatively low, they do indicate that we need to continue to improve the education of faculty and residents teaching students in the M3 and M4 years. 11. Evaluate the familiarity of students and course and clerkship directors with the school’s standards and policies for student advancement, graduation, disciplinary action, appeal, and dismissal. Review the adequacy of systems for providing students with access to the records and ensuring the confidentiality of student records. Students and course and clerkship directors are very aware of the school’s standards and policies for student advancement, graduation, disciplinary action, appeal, and dismissal. In addition to their availability in the Bulletin of the Brody School of Medicine (Appendix MS-A) and on the Student Affairs website, the Assistant Dean for Student Affairs presents the information during orientation to all four student classes and provides them with written copies of the documents. Additionally, any student experiencing academic difficulty meets individually with the Assistant Dean at which time the policies and procedures are reviewed. Course and clerkship directors routinely discuss and review these policies at meetings of the curriculum committees. Faculty members, including course and clerkship directors also review the policies in preparation for service on other committees including the year specific Student Review and Promotion Committees, and ad hoc Promotions Review and Appeals Committees (Appendix MS-K). It is anticipated that the implementation of the Academic Achievement Program will serve to enhance the knowledge of both students and faculty members in all aspects of student advancement. The BSOM system for providing students with access to their records and for ensuring the confidentiality of student records is functioning smoothly. Medical student academic records are maintained securely in the Admissions Office which also houses the BSOM Registrar. In compliance with FERPA, only administrative staff members of the Admissions/Registrar’s office and BSOM officials with a legitimate educational interest are permitted to review medical student records, which are never removed from the office. Upon inquiry to the BSOM Office of the Registrar, any student will be allowed access to the contents of his/her file under the supervision of staff of the Admissions/Registrar’s office. In the independent student analysis, 62% of current students view the availability of student records for review and challenge as “Excellent” or “Good”, 6% as “Fair” or “Poor”. 12. Access the adequacy and quality of student study space, lounge and relaxation areas, and personal storage facilities at all educational sites. Do available resources for study contribute to an environment conducive to learning? Since the last accreditation site visit a new Health Sciences Library has been constructed. The majority of the second floor space of the old library which is located contiguous to the M1 and M2 classrooms has been converted to student accessible space. This space, consisting of a total of 6,900 square feet contains the Medical Student Technology Center, study space, and student locker and lounge space. These spaces are used primarily by M1 and M2 students. The technology center 25 contains 20 desktop computers, 2 networked printers, a copier and a scanner. There is also a small group study room in the center. The study space contains cubicles, study rooms, tables and chairs with wireless network access. The locker and lounge area contains individual lockers and mailboxes, as well as couches, chairs, and a kitchen area. All areas are available to the students 24/7 by card access. The student independent analysis reveals that 65% of the respondents believe the adequacy of this area as “Excellent” or “Good”, with 20% as “Fair” or “Good”. It should be noted that new furniture has been purchased and installed in this area since the survey was completed. This area is spacious, with access restricted to students and a limited number of faculty and administrators. A portion of this space (approximately 1/3 of the study area) has been temporarily assigned to the School of Dental Medicine to contain simulated dental operatories. The portion that has been renovated for this purpose will revert to the School of Medicine upon completion of Ross Dental Hall. During the construction phase of this project, 2 rooms on the west hallway of the second floor of the Brody Building were reserved for medical student study. During 2011-2012, 52 first year dental students will share the study and lounge area with the medical students. They will also use a classroom on the second floor of the Brody Building temporarily assigned for their use. While this will likely cause some inconvenience to our students, the partnership with the School of Dental Medicine has provided funding for upgrades in furnishings and amenities in these student areas. Future interprofessional training opportunities will enhance the education in both professional schools. Question 28 of the independent student analysis assesses the adequacy of the M3/M4 student lounge. Thirty-seven percent of the M3 and M4 students rated this area as “Excellent” or “Good” and 43% as “Fair” or “Poor”. This area is located in the teaching annex of Pitt County Memorial Hospital (UHSMC) and is a locker area. The students express the opinion that the lounge area is very small with inadequate seating and computer access. The space was refurbished in 2011. IV. Faculty A. Number, Qualifications and Functions 1. Assess the appropriateness of the current size and mix of faculty for the attainment of the medical education program’s goals. The current size and mix of the faculty are fully appropriate to meet the tripartite mission of the school. BSOM has a long-standing tradition as a national leader in graduates entering primary care, rural practice and caring for the under-served. BSOM has responded to the increasing numbers of patients being transferred from regional hospitals for both primary and tertiary care by expansion the number of non-primary care faculty as well as the development an integrated disease-based approach for cardiovascular health and for cancer. This has improved the medical care provided to the people of eastern North Carolina, and simultaneously created a more robust educational experience for our students. BSOM has the highest minority enrollment (23 percent) of all historically white medical schools nationwide, resulting in the school being a national leader in graduating minority physicians. Additionally, the BSOM is also a top-ranked medical school for Hispanic and Native American students. Despite these achievements, our current faculty only reflects the national norm and further diversification of the faculty continues to be an area for improvement. One such attempt was the development of The INSPRE (Inclusion, Support, Professional development, Retention, Enrichment) Program which is a formal mentoring program initiated by the medical school in 2009 to improve the recruitment and retention of outstanding faculty members of color and women 26 faculty. Participants for this program are selected by department chairs. INSPRE faculty development program activities take place throughout the academic year addressing a variety of topics. There are scheduled peer mentoring sessions where participants gain valuable advice from senior faculty. 2. Describe and evaluate the availability of opportunities for both new and experienced faculty members (full time, part time, volunteer) to improve their skills in teaching and evaluation. Is institutional or departmental level assistance, such as training sessions from education specialists readily available? Comment on the level of faculty participation in such programs. Each department sets the expectation for required participation in professional development activities specifically related to teaching and assessment. However, faculty members of all departments are afforded the opportunity to attend faculty development activities offered through the Office of Faculty Development at our institution (e.g., Medical Education Grand Rounds.). A summary of each department’s expectations is provided in section FA-4. For clinical departments, all of whom provide post-graduate residency and fellowship training, the ACGME requires ongoing faculty development activities related to teaching and evaluation. The annual faculty and course evaluation processes provide important feedback on improving teaching skills. For the individual faculty member in a tenure track position, BSOM and University policies regarding promotion and tenure requirements specify that trained peer-reviewers evaluate both large and small group teaching sessions and provide feedback to the faculty. By virtue of undergoing this peer-reviewed teaching and feedback, the level of participation among those in the tenure track is nearly 100%. In academic year, 2009-2010, 115 faculty members requested a peerreview evaluation of their teaching. Course evaluations which include feedback on individual members provide another source of teaching feedback. Basic science courses are evaluated by M1 and M2 students at the end of the fall and spring semesters. M3 and M4 students complete evaluations at the end of each cohort for required core rotations, with evaluations designed for each particular rotation. Finally, while not specifically required, many faculty members also attend or are national leaders in discipline-specific organizations or societies which focus on education. 3. Do faulty receive appropriate support and mentorship related to scholarship? Are formal institutional programs available to support faculty research? Yes. There are both formal and informal mentorship programs to support faculty scholarship. ECU, BSOM and departmental programs are specifically outlined in section FA-5. While a survey of all basic & clinical science department chairs found 100% provided informal mentoring of junior faculty, 44% had formal departmental programs. University and BSOM also provide several formal mentoring programs. Formal workshops to foster scholarship development are offered twice a year by the ECU Office of Faculty Excellence, including “How to Write a Grant”, “Statistics”, and Grant Review. The BSOM Office of Faculty Development offers annual workshops on “Beginning My Clinical Research Protocol”, “Introduction to Clinical Research” and “Designing My Clinical Research.” Additional workshops included “How to Prepare a Manuscript”, “Finalizing My Clinical Research Protocol” and “Online Research: PubMed, OVID, RefWorks”. The INSPRE faculty development program addresses mentorship of research. There are scheduled peer mentoring sessions where participants gain valuable advice from senior faculty. Finally, faculty 27 members in different BSOM departments with common research interests meet regularly (e.g., Neurobiology Interest Group, Stem Cell Interest group). B. Personnel Policies 4. Evaluate the system for the appointment, renewal of appointment, promotion, granting of tenure, and dismissal of faculty members. Are the policies clear, widely understood, and followed? As a component of East Carolina University, BSOM firmly adheres to the personnel policies and procedures detailed in the ECU Faculty Manual. The general criterion for appointment, reappointment, and promotion includes evaluation on achievements in the areas of Teaching, Creative Activity/Research and Service to the university, the profession, and the community. All of these policies are available in the Faculty Manual which is available to every faculty member online. While comprehensive in nature, these policies are clear, understood and followed. 5. Assess the adequacy of institutional and departmental conflict of interest policies relating to faculty members’ performance of their academic responsibilities. Policies related to potential conflicts of interest are comprehensively addressed in FA-8. The University, the Division of Research & Graduate Studies, and BSOM each have specific, yet integrated policies regarding conflict of interest. Each is available to every faculty member online. In addition, the BSOM Code of Conduct also provides guidance in areas of conflict of interest. Every faculty member is required annually to sign an attestation statement in regard to conflict of interest and code of conduct policies. 6. Describe the extent of feedback provided to faculty members about their academic performance and progress toward promotion and/or retention. Are faculty members regularly informed about their job responsibilities and the expectation that they must meet for promotion and/or retention? Information regarding faculty responsibilities is contained within Appendices C & D of the Faculty Manual, available to faculty at all times online. Faculty members are informed about their responsibilities in teaching, research and patient care in discussion with the Chair of their department when they assume their roles. With respect to teaching responsibilities, prior to making final faculty assignments and at least two weeks prior to the beginning of each semester, the unit administrator informs the faculty member, in writing, of the duties and responsibilities in teaching, after soliciting faculty teaching preferences. If changes in a faculty member's assignment become necessary, the faculty member shall be notified of such changes prior to the effective date of the amended assignment. Likewise for clinical responsibilities, the Chair or his/her designee is responsible for outlining expectations for clinical performance. Policies related to evaluation of a faculty member’s academic performance, as well as progress towards promotion and tenure, are comprehensively outlined in Appendices C and L of Faculty Manual and summarized in section FA-10. Evaluation of each faculty member occurs in the spring and is completed prior to the next academic year. The School of Medicine requires that the final faculty evaluation forms be in the Office of Health Sciences Personnel by June 15th each year. By policy this annual evaluation is in writings, states the percentage of variable salary increment available to the unit to be recommended by the unit administrator for the faculty being evaluated, is with the faculty member prior to being sent to any other administrator or placed in the faculty member's personnel file and in the case of faculty members with probationary period appointments, a record of this discussion shall be placed in the faculty member's personnel file. The evaluation is 28 signed and dated by the unit administrator (i.e., department chair) and the faculty member, who may attach a concise comment. The signature of the faculty member signifies that the faculty member has read, but does not necessarily concur in, the evaluation. 7. Discuss the extent to which education is valued in the institution. How are the degree and quality of participation in medical student education factored into decision about faculty retention and promotion? East Carolina University requires that evaluation of teaching is included in the annual review of each faculty member. For probationary term (tenure-track) faculty, peer evaluation of teaching is a required part of faculty annual evaluation during the first and third years of the probationary term of employment. All tenured faculty members undergo periodic post-tenure review, including review of teaching effectiveness. As a constituent institution of the University of North Carolina system, ECU recognizes that teaching is the primary consideration of all UNC institutions. Education of future physicians while providing patient care is a primary focus of BSOM. This educational commitment is demonstrated by the BSOM Governance Code, Section V. which stipulates that the relative weight given for teaching and research during the annual faculty evaluation must range between 10 to 80%, and the relative weight for service (including clinical service) range between 10 to 40%. Departmental promotion and tenure guidelines show that accomplishment as an educator can be a primary component in evaluating faculty performance. Despite the financial stress created by the nationwide economic recession which has placed more pressure on the faculty for clinical and research grant productivity, there is a clear expectation that excellence in contribution to the teaching mission must be achieved for tenure and promotion. ECU and BSOM support teaching excellence through a variety of high profile awards and activities. BSOM faculty members have achieved national and international recognition for innovations in medical education, including the Standardized Patient program and with multidisciplinary teaching. Support for these programs comes from internal funds, Title VII funds and external grants. C. Governance 8. Evaluate the effectiveness of mechanisms for organizational decision-making. Are necessary decision made in a timely and efficient manner with appropriate input from faculty and other concerned parties? Describe and asses the relative roles of committees of the faculty, department heads, and medical administrators in institutional decision making. From the standpoint of faculty input, as demonstrated in section FA-13, there is active involvement by the faculty across the full spectrum of academic, research and clinical issues. The average number of members per committee listed in the table in section FA-13a, is 14.3. As a result of this strong faculty participation, a variety of potential options may be elicited for any specific problem. With rare exception, each committee ultimately reports to the BSOM Dean, which results in an organized and prioritized approach to problem solving. While organizational decision-making has traditionally been timely and effective, recently efforts have been made to increase transparency. With respect to transfer of information back to the faculty, the Governance Code requires regular general meetings of the faculty of the School of Medicine. These meetings currently take place quarterly in the auditorium and are led by the Dean. Meeting dates are announced at the beginning of the academic year, and agendas for each meeting are distributed in advance to all faculty. Agendas for these meetings typically include a Dean’s report, reports on admissions, budgets, clinical operations, research and graduate studies, and academic affairs, and, annually, approval of candidates for the MD degree, and elections of Faculty Senators, at-large members of the Executive Curriculum Committee, and Tenure and Promotions Committee members. 29 9. Assess the effectiveness of the methods used to communicate with and among the faculty. Do faculty perceive themselves to be well informed about important issues at the institution? Do faculty believe that they have sufficient opportunities to make themselves heard? A variety of methods are used to communicate with and among the faculty. As a result, it is a generally held belief that the majority of faculty members feel they are kept appropriately well informed and have multiple opportunities to make themselves heard. One objective measure of faculty satisfaction with communication can be seen in the 61% response rate for the AAMC initiated Faculty Forward Program. This faculty response rate was the highest in the nation and the majority of the feedback was positive. However, as with any communication system in a large, multi-purpose organization there is always room for improvement; the administration continuously works to further enhance communication. Several examples of current methods of communication are outlined below. The importance of communication is reflected in the Governance Code which requires regular faculty meetings with the entire faculty. Copies of draft policies and procedures, and related materials being considered for enactment are typically distributed prior to the general faculty meetings in which they’re being discussed. Also as stated above the BSOM committee structure allows for broad representation and an open exchange of ideas. For those faculty members who may not be able to attend a faculty meeting or serve on a committee, communication is maintained using electronic media, via the BSOM-wide e-mail system. Using this mechanism, the Dean communicates with faculty through e-memoranda announcing major decisions and events, such as new administrative appointments. Other administrators of both the School of Medicine (department chairs, assistant and associated deans etc.) and the University extensively use the University e-mail system for distribution of informational memoranda, flyers, and posters in addition to traditional written communications. Finally, the Dean has recently developed a blog that he regularly updates, which allows for ongoing communication with the faculty and students. V. Educational Resources A. Finances 1. Discuss the stability of and the balance among the various sources of financial support for the medical education program and school (i.e., state and local appropriations, income from patient care, endowments, tuition income, research income, hospital revenues). Discuss the implications of any downward trends in specific revenue sources. Describe the financial prospects for the medical school over the past five years. Are there any departments in financial difficulty? Are there systems/policies in place to address departmental financial difficulties? Practice Plan State Appropriation Hospital Support Grants and Contracts Other Tuition and Fees Future Stability Improving Stable Improving Improving Stable Stable Current Stability Improving Poor Good Good Good Good Recent Stability Poor Poor Fair Good Good Good Balance 50% is too high 22% is about right 16% is a little low 8% is too low 2% is too low 1% is about right 30 The overall financial picture of BSOM has shown steady improvement over the past 3 years resulting in operating margins of 99.19% in 2008, 99.90% in 2009, and 100.73% in 2010. The major financial drivers for BSOM during the past six years, however, have been inconsistent, as indicated in the table above. Shortly after the 2004 LCME site visit, the state appropriation began to experience annual cuts, and the faculty practice plan began to run a deficit, depleting reserves accumulated in the 1990s. A variety of changes were made, including the temporary involvement of an independent management group , and the practice plan has been revenue neutral or contributing to reserves during the 2010 and 2011 fiscal years. The ability of the practice plan to generate income in this challenging financial time is a tribute both to the efforts of the clinical faculty and the strategic expansion of the ECU Physicians clinical enterprise into new areas. The dramatic positive turnaround in the practice plan was offset by a decline in state appropriations during the economic downturn of 2009 and 2010. During the spring of 2011, the fiscal balance sheet of the state of North Carolina is improving slowly, reflecting the beginnings of an economic recovery. Our hope for 2012 and beyond is that both the faculty practice plan and state appropriation continue their upward trajectory. ER2.c.iv and ER2.d.iii and iv describe additional steps that have been taken to enhance revenue and consequently further replenish the practice plan reserves. In addition, streamlining of grant submission processes and revitalization of the clinical trials office is expected to further increase revenue from grants and contracts. Endowment income is too low for a medical school, and efforts are underway to enhance both community and alumni contributions. During 2011, BSOM plans to develop a multi-year financial plan for the first time in its history. This plan will emphasize practice plan and state revenues, which together account for 72% of the school finances. Details about this financial planning are included in question 3 of the Educational Resources section of the institutional self summary. Regarding the financial performance of individual departments, BSOM and ECU Physicians use multiple methods to track the financial performance of academic departments on a regular basis. The finances for basic science departments are drawn primarily from state appropriations and from extramural funding. There is no opportunity for any of these eight departments to run a deficit. They carefully manage their state funds against extramural funding to cover personnel and operating expenses. None of these departments have had financial difficulty. The eleven clinical departments draw from state appropriations, extramural funding, and practice plan funds. These departments cover most of their personnel and operating expenses from practice plan funds. The Dean uses several approaches to work with these department chairs to track their financial performance: On a monthly basis, the Dean meets individually with each clinical chair. The Vice Dean and the Executive Director for ECU Physicians also attend. Part of this meeting is a financial review. For departments with significant financial difficulties, these meetings are held twice a month. The ECU Physicians Finance Committee monitors the financial performance of each clinical department, including the monthly variance reports for each department. A process for closer financial oversight for two departments is nearly complete and likely to be implemented during the fall of 2011. This process will include the triggers for stopping discretionary spending by the department so that available funds can be devoted to core responsibilities such as education and patient care. 31 2. Comment on the degree which pressures to generate revenue affect the desired balance of activities of faculty members. What mechanisms are in place to support the accomplishment of the educational mission? BSOM is fortunate to have significant state appropriations to support the educational mission. Faculty salary lines in the basic science departments are fully funded, and support teaching in the medical, graduate, and allied health professional programs. Additional teaching duties in professional programs, including the new School of Dental Medicine, are offset by new funds to support faculty expansion. Thus, in the basic science departments, pursuit of research funding does not negatively impact medical education, and in fact enhances it by ensuring that instructors remain current in the advances in their discipline. For clinical departments, a similar financial support system ensures that any increase in clinical duties is offset by an expansion of the clinical faculty (see ER3.a.i.1 for additional information and metrics). The pressure to generate revenue is a well-described challenge by most clinical faculty in most medical schools. The outcomes they associate with the pressure are a decrease in time to teach and reduced scholarly productivity; the clinical faculty at Brody School of Medicine are not exceptions to these feelings. While the number of MD faculty has increased, the academic full term equivalent has remained stable: more faculty to provide clinical care teaching. In addition, since 2004-2005 we have increased the number of nurse practitioners, physician assistants, and certified nurse midwives by 26%. These personnel enhance medical student experiences by reducing the clinical load for the faculty and providing an interprofessional experience with clinical care teams which include advanced practice professionals. Finally, the percent of State Funding support for clinical faculty compensation has decreased since 2004-2005, but the amount of salary support which is state funded exceeds the vast majority of state medical schools. The percentage of operating budget generated from tuition and fees is low, and is not a financial driver for BSOM. 3. Describe how the school has positioned its clinical enterprise for achieving optimal results in the local health care environment. Is planning related to the clinical enterprise occurring? Are medical school leaders involved in such planning? How effective is this planning in meeting institutional goals? The shifting reimbursement patterns and health care reform nationally have impacted BSOM as much as any other medical school over the past several years. After careful planning, we have taken several important steps to position ECU Physicians, the multispecialty group practice, to achieve optimal results in our local environment: Opened the East Carolina Heart Institute in the fall of 2008 with over 240,000 square feet of clinical, teaching, research, office, and conference space constructed and supported with state appropriations; Completed a new Family Medicine Center in July 2011 containing over 110,000 square feet of clinical, teaching, office, and conference space constructed and supported with state appropriations; In addition, acquired nearly 100,000 square feet through leases for new ambulatory clinical space for teaching clinics, faculty clinics, an endoscopy center, and a sleep disorders center; Negotiated a new agreement with our primary teaching hospital (University Health Systems Medical Center) to support the School’s efforts in graduate medical education that increased funding by 33% in the first year alone; 32 Reached agreement with the North Carolina Division of Medical Assistance and the Centers for Medicare & Medicaid Services (CMS) for “upper payment limit” reimbursement of care provided for Medicaid patients that will provide upwards of $4 million new funds annually, retroactive to July 1, 2010; Launched a new corporate venture for cancer care with PCMH that creates a new foundation for multidisciplinary care of all forms of cancer; and Participated in the groundbreaking of the James and Connie Maynard Children’s Hospital of Eastern North Carolina which will ultimately have five floors of ultramodern pediatric services, in which all pediatric subspecialty care is delivered by the School’s faculty. These new facilities and organizational approaches will build on the existing volume of over 500,000 patient visits annually and our rich tradition of providing care for the people of the region. Planning for the clinical enterprise is led by the Dean, who serves as the CEO of ECU Physicians. In collaboration with the Executive Director and the Medical Director, he is working with several clinical chairs to elaborate the most advantageous model of partnering with external entities and strengthen our position as the premier group practice in the eastern third of the state. ECU Physicians executives are also joining with the leadership of the University Health System of Eastern North Carolina (UHS) in discussions to create a new model of care for dual-eligible patients (both Medicare and Medicaid) in collaboration with CMS and the State of North Carolina. The ECU Physicians Board of Directors meets twice a month to provide the strategic management of our clinical enterprise. In addition to directly overseeing the financial performance of the practice, the Board determines the success of such tactical measures as retention of referrals within ECU Physicians, providing patients with the best possible experience, and development of patient centered medical homes. This group is the final determinant on all planning efforts for the practice, the success of which is demonstrated in the steps noted above. The Board is chaired by the Dean and includes all Clinical Chairs, three faculty representatives, the Vice Chancellor for Health Sciences, the Vice Chancellor for Administration & Finance, the Chief of the Medical Staff of UHSMC, and the Associate Dean for GME. 4. Describe how present and future capital needs are being addressed. Is the financial condition of the school such that these needs are being and will continue to be met? BSOM is fortunate in that the present and future capital needs are met through requests and prioritization from ECU to the UNC system and from there through the State of NC planning process. Capital needs related to the clinical practice are addressed through the funding of the practice plan. The expansion of the West Health Sciences Campus is a priority in the ECU strategic plan. The new Laupus Health Sciences Library has been constructed since the last LCME site visit, as have buildings housing the College of Nursing and the College of Allied Health Sciences. Ross Hall, the future home of the School of Dental Medicine is currently under construction. More directly related to the Brody School of Medicine, a floor of the East Carolina Heart Institute is being completed for the Cardiovascular Institute and the Metabolic Institute. Also as part of this process, the Department of Family Medicine moved into a new state of the practice 112,000 ft.² facility in July 2011. This new facility will house both Family Medicine and Geriatrics. The practice plan has leased two recently constructed outpatient facilities, referred to as Moye Medical 1 and Moye Medical 2, which house Internal Medicine services, surgical services, an outpatient Endoscopy Center, Medicine/Pediatric clinic, and outpatient Pharmacy. Plans are being 33 discussed for constructing a new outpatient facility, Moye Medical 3, for women's and children's services. B. General Facilities 5. Evaluate the adequacy of the general facilities for the teaching, research, and service activities of the medical school. Are there opportunities for educational excellence or educational change (e.g., introduction of small group teaching, opportunities for active learning) or for the attainment of other medical school missions constrained by space concerns? Describe the likelihood that needed space of space upgrading will be available in the near future. Have enrollment increases led to space constraints? If so, describe how these constraints are currently being addressed. The general facilities for teaching research and service activities are adequate for the current number of students enrolled at BSOM. The majority of the preclinical lecturing is done in the lecture halls on the second floor of the Brody Medical Sciences Building. The technology used for teaching was updated in 2010, allowing video lecture capture (see additional details in ER4.a). During the preclinical years, the doctoring courses often meet in the clinical skills assessment and education facility, the technology of which has also recently been upgraded. As the preclinical curriculum shifts to greater use of small group activities, the number of small group rooms available during the afternoons does represent a potential limitation that can be overcome by careful scheduling. Space for instruction during the clinical clerkships at UHSMC and in the ambulatory settings is also adequate (more details in summary 7 below). The pursuit of a cross-disciplinary “Institute” model for research has allowed the research resources and space for select areas (Cancer, Cardiovascular, and Metabolic) to expand. The strengthening of these areas does create resource disparities for research areas not under an institute umbrella. The research program at BSOM is not sufficiently large to allow excellence in all areas, and the strategic decision was to focus the research activities on areas reflecting the health needs of the people of eastern North Carolina. Not surprisingly, additional resources can enhance the educational program. For example, the Simulation Center is a resource that is underutilized, and the student educational experience would be enhanced by allocation of additional space and resources. As testing and assessment moves to more on-line formats, a computer testing facility needs to be established. The Introduction to Medicine and Microbiology courses are experimenting with Team-Based Learning instructional format, and the laboratory on the 7th floor is suited for this activity. That same laboratory is used for Histology, Neuroscience and Pathology, and if TBL is expanded, scheduling issues may emerge. The preclinical educational space is fully utilized. Consequently, there is little opportunity for class size expansion with the current resources. Plans for expansion of class size are contingent on construction and allocation of additional resources, as indicated in the reports included in the selfstudy as Attachment V Item 1a and 1b. 6. Describe the adequacy of security systems on each campus and affiliated sites. Security systems at ECU, BSOM and the affiliated hospital UHSMC are professional and excellent. There have been no incidents or complaints at other affiliated teaching sites. C. Clinical Teaching Facilities 34 7. Analyze the resources for clinical teaching available to the medical education program. For the size of the student body, are there adequate numbers of patients and supervisors available at all sites? Has the school needed to expand its clinical teaching network to address either expanded enrolment or decreased patient volume? Is the patient mix appropriate? Are clinical facilities, equipment, and support services appropriated for exemplary patient care? Discuss the availability, quality, and sufficiency of ambulatory care facilities for teaching. Clinical teaching facilities (except as noted below) are excellent and well suited for medical education. Most medical students on Core MS3clerkships have a major portion (50-100%) of their educational experiences at University Health Systems Medical Center (inpatient) or BSOM outpatient facilities. The Psychiatry MSIII core clerkship is the only clerkship where students can spend their entire clerkship away from BSOM or UHSMC. BSOM and UHSMC have an excess of high quality and high acuity clinical material for the current number of medical students. The patient mix is somewhat skewed, as UHSMC and Brody School of Medicine serve a disproportionate share of the indigent patients in eastern North Carolina. Self-pay, Medicaid, and Medicare account for 58% of the BSOM patient care funding. More than 90% of the patient populations at the core facilities are available to adequately supervised medical student education. The ratio of clinical full time faculty to 12-16 students per core rotation ranged from 0.94 to 3.25 in June 2010. The supervision, coordination, evaluation, and faculty development at the core facilities are consistent, appropriate, and timely. Overall, the clinical facilities, equipment, and support comfortably accommodate a class size of 80 or less. If the clerkship numbers exceed 16 per rotation, some resources will be stretched. The number of rooms for small group education (5-20 seats) and large group education (40-60 seats) rooms could accommodate a larger number of students. The equipment and support personnel are adequate for the quaternary care delivered by the two institutions. One mission of Brody School of Medicine is to provide clinical experience in rural primary care. Family Medicine and Pediatrics commit a portion of their core M-3 rotation to community clinic experiences. The education experience is similar for all students within a clerkship. The ambulatory clinics at Brody combined with the 16 Pediatric community sites, 27 Family Medicine community sites, and 3 Psychiatry community sites provide a great patient variety and great ambulatory care experience for our students. There are enough community sites so that there is no difficulty with availability when it comes making student assignments. Each of our sites provides modern clinical facilities, equipment and support services for excellent patient care. Training sites have good patient volume and sufficient distribution of both well child visits and acute care visits to provide a broad ambulatory educational experience. Pediatrics and Family Medicine continue to try to add additional community sites for the clerkships - mostly to provide a variety of options to the students, but also to make sure there are enough sites in case some of the community partners cannot take students during particular months. In contrast to the modern facilities used by all community sites and most BSOM ambulatory clerkships, the ambulatory care facilities at BSOM are not well suited for medical student teaching in Pediatrics and in Obstetrics/Gynecology. These settings function in facilities built 20-30 years ago. There is a distinct lack of space for small group teaching in close proximity to patient care. The newer spaces in the other disciplines have more than adequate availability, quality, and sufficiency for ambulatory care facilities. The recent groundbreaking for the Children’s Hospital UHSMC is a significant step toward upgrading these facilities, as is the planning for a new outpatient building (Moye Medical III) for women’s and children’s health. 35 8. Describe and evaluate the interaction between the administrators of clinical affiliates used for teaching and the administrators of the medical school. Does the level of cooperation between these groups result in a smoothly operating and effective clinical education program? Communication and interactions between the clerkship directors and the administrators at the community sites are excellent; consequently, the clinical education program runs smoothly. The clerkship coordinator contacts each site prior to each academic year, generally through the site's practice manager, to assess each site's availability for BSOM students during the coming academic year. Student assignments are confirmed through mail at the beginning of the year - with changes in these assignments confirmed through phone conversations and e-mail through the clerkship coordinators. Throughout the year, if there are either student or preceptor concerns regarding this educational experience, communication by phone or e-mail occurs between the clerkship director and/or the associate clerkship director in order to discuss these concerns. Student evaluation forms are mailed or faxed to our different community locations and completed forms are faxed back to our office. Visits by the clerkship director and/or associate clerkship director are performed at any new potential community sites before students are sent there. At these visits, the goals and objectives of the clerkship, preceptor evaluation or our students, and assessment of the clinical experience for our students are reviewed with each faculty preceptor. Similar visits are expected every 1-2 years at our existing community sites. Cooperation overall between our community sites and our clerkship is very good, leading to a great educational experience that is appreciated by the majority of our students. This relationship is a reflection of our region's commitment to support medical education and the mission of our institution. 9. Describe and evaluate the level of interaction and cooperation related especially to the medical education program that exists between the staff members of the clinical affiliates used for teaching and medical school faculty members and department heads, related especially to the education of medical students. Clerkship Directors in each discipline report supportive and adequate supervision of the medical students and interactions with their coordinators. Communication with the staff members at the clinical affiliates is through a combination of bi-annual meetings, direct site visits, phone calls, email, and letters. The affiliates are readily available to be reached as the need occurs. Family Medicine provides annual curricular updates, goals/objectives, and evaluation guidelines to their affiliates. On a bi-annual basis, they provide direct student-documented feedback to our affiliates to use for personal growth. In the event there is a negative comment, Family Medicine acts immediately to clarify any areas for improvement. Similarly, communication and interactions between these outlying sites and Pediatrics are maintained by periodic visits by the clerkship director and/or associate clerkship director, and continued open communication by email and phone between these same members of the department of pediatrics and the faculty preceptors. The Psychiatry clerkship director also meets with the affiliated staff during a bi-annual clerkship meeting and in person as needed. Students provide excellent feedback regarding their educational experience at the “away” locations. In the event that there is a concern from a student, the clerkship director and/or chair have been able to work directly with the preceptor site to clarify any discrepancies. 36 Improvement plan: We shall monitor on-site meetings between the clerkship directors and the clinical affiliate coordinators including measurement of the quality of off-site education, and the plan for pedagogic education for the clinical affiliate faculty. These challenges are especially true for Psychiatry. D. Information Resources and Library Services 10. Evaluate the quantity and quality of the print and non-print holdings of the library as a resource for medical students, graduate students, and faculty members. Membership in multiple consortia (see ER-11.b) provides students, faculty and staff at BSOM with excellent electronic access to journals and other materials to support research and education. The same electronic resources can be accessed from off campus sites by logging in to the library page using the individual’s user ID. The relocation of the College of Nursing and the College of Allied Health Sciences to the Health Sciences Campus resulted in the expansion of the quantity and scope of health related print and media resources, benefitting both the medical and other learners. As is appropriate in this information age, priority has been placed on expanding access to digital resources, including a computer lab and terminals within the library and printing services. The print resources most popular with medical students are the textbook collections. Textbooks for major courses are placed on reserve, allowing shared student use. 11. Comment on the adequacy of information technology resources and services, particularly as they relate to medical student education. Are resources adequate to support the needs of the educational program? Are the information systems of the medical school and major clinical affiliates sufficiently well integrated to ensure achievement of the medical school’s missions? Note any problems and describe any plans in place to address these problems. The technology resources at Laupus Library are excellent, including “loaner” use of iPADs and other items. The technology resources within BSOM supported directly by the I.T. department at ECU, including include the Blackboard course management system and video lecture capture for the classrooms. Although there are only a few technology staff at BSOM, they are exceptionally responsive, and in particular the relocation of the IT office (Adam Brewer) to the 2nd floor of BSOM has been extremely effective. One recurring problem that is being diminished by better communication and planning is the difference between the academic calendars at BSOM and ECU. Blackboard upgrades are scheduled during the ECU spring break and immediately after the end of each ECU Semester. The BSOM academic calendar has classes and examinations during these times in the M1 and M2 years, and classes and examinations year-round in the M3 and M4 years. Through the actions of the Executive Curriculum Committee and Office of Academic Affairs, the ECU IT group is now better aware of the needs of BSOM courses, and this problem has been diminished. For example, the ECU IT group established a mirror site for use by BSOM during the upgrade of Blackboard in May of 2011. Continued vigilance is necessary to minimize or eliminate these disruptions. On-line testing facilities at Laupus Library can accommodate a portion of the class; this is suitable for NBME Subject exams in the clinical clerkships. The move to on-line testing in the preclinical years has been slow at BSOM, impeded by the lack of a dedicated on-line testing center capable of handling the entire 78 student class and the lack of appropriate software for item analysis. Histology has been an early adopter of on-line testing using the Blackboard course management system due to the use of high-resolution images. The Blackboard system has only a rudimentary item analysis 37 capability, which will hopefully be part of a future Blackboard upgrade. One consequence of the lack of detailed item analysis is that even though students use computers for the Histology testing, they also complete a paper Scantron answer sheet for the same test, which is used for the item analysis. Improvement plan: Academic Affairs is actively seeking resources to establish a computer testing center. 12. Evaluate the usability and functional convenience of the library and of information resources. Are hours appropriate? Is assistance available? Is study space adequate? Are resources such as computers and audiovisual equipment adequate? Can students access information from affiliated hospitals or from home? The Laupus Health Science Library supports the medical students by providing appropriate electronic, print and media resources, assistance with information retrieval, and a quiet study environment. Sixty employees provide support at a variety of levels, and there is an emphasis on staff professional development and certification. The library has 31 small group study rooms that can accommodate 4 students each. The library is open 93.5 hours per week, in addition to extended hours during examination weeks. All online databases and resources are available to affiliated users, including Distance Education students, from any location via the Laupus Library website. ECU students, faculty and staff use their “Pirate ID” to login and gain access to all online resources including the library catalog, citation management resources, research databases, online full-text books and journals, and various other services. 13. Assess the contributions of library and information technology staff to the education of medical student and the professional development of faculty members in the following areas: Teaching specific skills, such as instruction in computer usage and bibliographic search Retrieving and managing information. Interaction with the curriculum committee to coordinate various library and information resources with planned curricular designs. Librarians are well integrated into the curriculum of the medical students and residents. In addressing the specific points above: Two liaison librarians are assigned to BSOM to support activities in the preclinical years, including delivery of targeted instruction and building relationships with faculty and students. Liaison librarians attend and contribute to Grand Rounds for clinical departments, in addition to providing orientation and database search classes for medical students and residents as part of an “evidence based practice” program (see ER 12.c for additional information). In addition to the activities integrated in the courses and resident orientation, librarians provide oneon-one and small group consultations on in-depth questions. Classes in basic library skills are taught throughout the semester, including some available as asynchronous self-paced modules. The library has developed “LibGuides”, i.e., web-based instructional modules, podcasts and video tutorials providing an orientation to library research. 38 Librarians are resource members of the Executive Curriculum Committee, the M1, and M2 curriculum committees, and present at the M3 and M4 curriculum committee meetings. This allows the librarians to participate in discussions and decisions about student information needs, curriculum changes, and to inform students and faculty about library initiatives and resources. Summary Brody School of Medicine is strong because we remain true to our mission. In the past ten years, over 50% of our students have entered primary care careers (Family, Internal Medicine and Pediatrics). This success is due in part to the admission process where primary care is emphasized, the model experienced of strong primary care service, and our low tuition. Our growth in all clinical areas, and particularly in cardiovascular sciences, and research has enabled us to better serve the people of eastern North Carolina. We offer pipeline programs and educational enrichment to assure the enrollment and success of minority and disadvantaged students. Our students are achieving scores on national examinations which meet or exceed the mean. This is an area for continued assessment. Our students and faculty are expert in using an electronic medical record system. The relationship with our teaching hospital has evolved to include joint ventures in the creation of a cancer center and an endoscopy center, as well as impressive increases in financial support for graduate medical education. This self- study summary recognizes several areas in transition: Our new curriculum mapping tool (E*Value) will track content better and encourage curriculum revision. The incorporation of web-based examinations should be accomplished by a larger computer testing center. The addition of the new School of Dental Medicine will add teaching demands on our basic science and clinical faculty but has the potential of helping us integrate our curriculum more effectively and providing new opportunities for interprofessional education. Curriculum revision will continue to address new topics such as patient safety, global health, health care reform, the economics of medicine and medical informatics. Although students are aware of a “mistreatment” policy, the percentage of reported events must consistently fall below the national mean. The percentage of students satisfied with debt management counseling will increase. The timeliness of clinical clerkship grades will be improved. New teaching methods such as team based learning have been incorporated into the curriculum. The Doctoring courses are considering the introduction of a continuity experience. Challenges to be addressed: Faculty development for affiliate faculty and residents as teachers will need further emphasis and monitoring. 39 The funding model for educational productivity should be analyzed and improved. The future expansion of the medical school class presents our biggest challenge. The vision has been defined, but the funding is yet to be realized. Success in expansion will not only produce more doctors, but also serve the eastern region of North Carolina through very positive economic and health outcomes. Appendix: List of self-study steering committee members, subcommittees with their titles and position. (No page numbers needed) 40