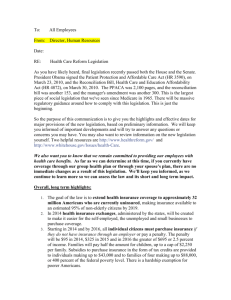
Federal Health Care Reform
advertisement

Federal Health Care Reform: Implications for the Marketplace Name Date Agenda ▪ Legislative overview ▪ What it means for you ▪ Continuing need for reform ▪ How to stay informed 2 Patient Protection and Affordable Care Act Signed March 23, 2010 3 Congressional Action on Federal Health Care Reform 3/21/10: House vote on Senate bill 3/21/10: House immediately votes on reconciliation “sidecar” 3/23/10: Final bill signed by President 3/23/10: Senate takes up reconciliation bill; begins 20-hour debate 3/25/10: Senate passes amended reconciliation bill, forcing House vote 3/25/10: House passes amended reconciliation sidecar 3/30/10: Reconciliation bill signed by President 4 Federal Reform Key Elements . New Taxes and Fees Market Reforms Individual Mandate Insurance Exchanges Employer Mandate 5 Key Elements: New Taxes and Fees New Taxes and Fees Effective in 2010: Annual tanning tax: 10% tax on indoor tanning services ($2.7 B) Effective in 2011: Annual pharmaceutical industry fee: Begins at $2.5 billon per year ($27 B) Effective in 2012: Annual medical device manufacturer fee: Excise tax of 2.3% on the sale of any taxable medical device ($20 B) Effective in 2013: Annual Medicare tax on high earners, and unearned income: 0.9% increase in payroll tax. Unearned income tax of 3.8% ($210.2 B) Effective in 2014: Annual insurer fee: Applies to fully-insured business ($60.1 B) Effective in 2018: Annual high-cost insurance tax: 40% excise tax on “Cadillac” plans ($32 B) 6 Key Elements: Market Reforms Market Reforms (2014) Small Group (2014+) Products ▪ All health insurance products in all markets “guaranteed issue” ▪ No health status rating; rating factors limited to: • • • • Age: 3:1 Tobacco: 1.5:1 Family size Geography ▪ Small Group redefined in most states from group size 2-50 to group size 1-100 ▪ Health insurance products must meet new benefit mandates and at least exhibit a 60% “actuarial value” 7 Key Elements: Insurance Exchanges Insurance Exchanges Effective in 2014: ▪Insurance Exchanges will act as a new sales channel beginning in 2014 ▪Requires states to establish Exchanges for individuals & small employers ▪Subsidies for individuals up to 400% of the federal poverty level, only available in exchange ▪Small employer tax credits available only in exchange ▪Potential role for agents/brokers 8 Key Elements: Individual Responsibility Individual Mandate (2014+) ▪ All U.S. citizens and legal residents required to have coverage Subsidies (2014+) ▪ Sliding scale, up to 400% of federal poverty level ($88,000/year for family of 4) Medicaid (2014+) ▪ Expanded to 133% FPL in all states ▪ Penalty phased in • $95 per year in 2014, phasing in to $695 per year by 2016, or 2.5% of taxable income • Exempts low-income individuals • Only available through exchanges • Mandatory enrollment under 100% of federal poverty level 9 Key Elements: Employer Responsibility “Play or Pay” Requirement: “Play” (2014+) Coverage Penalty: “Pay” (2014+) Employers with >50 full-time employees (FTEs) must offer minimum coverage: ▪ ▪ ▪ ▪ Part-time are included on FTE basis in calculating >50 FTE Full-time employee averages 30+ hours per week No minimum contribution Must provide “essential coverage” with 60% actuarial value minimum Employers with >50 full-time employees: ▪ Not offering coverage and at least one FTE receives tax credit • $2,000 x total number of FTEs (minus first 30 FTEs) ▪ Offering coverage at least one FTE receives tax credit but actuarial value < 60% or employee cost is > 9.5% of household income • Lesser of $2000 x total FTEs or $3000 x number of employees receiving tax credit 10 Key Elements: Other Employer Responsibilities Free Choice Voucher (2014+) Employers must provide for use in exchange if: Auto-Enrollment Employers >200 employees must auto enroll FTE into health plan (employee may opt out) Treasury Reporting Employers required to submit annual coverage reports W-2 Reporting Early Retiree Reinsurance (2010) ▪ Employee premium cost sharing is 8-9.5% of household income (>400% federal poverty level) Must disclose cost of coverage Temporary reinsurance for retirees 55-64 11 Key Elements: Employer Tax Elements Small Group Tax Credit (2010+) Retirees Drug Subsidy (2013+) High Cost Plan Excise Tax (2018+) Employers < 25 employees and < $50,000/year average wages contributing > 50% of premium • 2010-2013: sliding scale credit up to 35% of employer costs (25% if tax exempt) • 2014+: credit up to 50% of employer costs (35% if tax exempt) for first 2 years; limited to exchange only Eliminate tax exclusion for Part D subsidy payments 40% nondeductible tax ▪ For coverage that costs over $10,200 individual; $27,500 family coverage ▪ Amounts indexed to standard inflation ▪ Excludes dental and vision 12 For internal and other select audiences Other Federal Reform Key Elements Product Framework (actuarial value) Four tiers based on actuarial value: 60%, 70%, 80%, 90% effective in 2014. Separate policies for “young invincibles.” Cost-sharing limits tied to the HDHP limits. Additionally, small group deductibles may not exceed $2,000/$4,000. Medical Loss Ratio Requirements In 2011, MLR is set at 85% for large group and 80% for small group and individual markets. Insurance Rate Review Beginning in 2010, federal government to establish a process with states to require insurers to justify rate increases Medicare Advantage Cuts Medicare Advantage by a total of $202 billion by freezing benchmarks for one year in 2011 and then reducing benchmarks to different percentages of feefor-service Medicare spending, with bonuses for quality and enrollee satisfaction. Increases ability to reduce MA plan payments because of plan coding practices. Administrative Simplification Requires the Secretary to adopt and regularly update standards, implementation specifications, and operating rules for the electronic exchange and use of health information for the purposes of financial and administrative transactions. 13 Agenda ▪ Legislative overview ▪ What it means for you ▪ Continuing need for reform ▪ How to stay informed 14 Immediate Provisions Effective for the 2010 tax year: ▪ Tax credits for certain small employers ▪ $250 rebate to Medicare beneficiaries who reach the Part D “donut hole” Effective 90 days after enactment: ▪ Temporary high-risk pools and early-retiree reinsurance programs Effective for plan years starting 6 months after enactment: ▪ Dependent coverage for adult children up to age 26 ▪ No lifetime coverage limits ▪ No cost-sharing for preventive services (applies only to individuals not “grandfathered”) 15 Dependent Coverage for Adult Children Up to Age 26 Who: ▪ Existing members’ dependents who would have lost dependent benefits on or after June 1, 2010, based on their birthday, will now be eligible to continue benefits ▪ This includes specialty products such as vision, dental and pharmacy ▪ Exceptions noted below When: ▪ Beginning June 1, 2010 Why: ▪ The extension is designed to fill the coverage gap between June and September 23, 2010, when the dependent care provision in health care reform legislation takes effect Exceptions: ▪ Administrative Services Only (ASO), fully or partially self funded accounts with more than 100 lives, and fully insured accounts with more than 100 lives are able to opt out of the extension – we will work with these groups individually to meet their needs 16 Delete this slide if not relevant to audience Immediate Provisions “Grandfathering” of existing members ▪ Grandfather provision allows existing members to keep their products, except, requires all products renewed after September 23, 2010 to: • Allow members to add dependents up to age 26 regardless of student status • Eliminate lifetime limits on policies ▪ For new sales and subscribers who change policies after 3/23/10, we will be required to make additional changes beginning in approximately six months, such as removing any member cost sharing for "preventive" benefits, as defined by the legislation. 17 Effective Dates of Reform Provisions Beyond 2010 2011-2013 2014 Medicare Advantage cuts Individual mandate Grants for small employer wellness programs Individual market guaranteed issue All working adults enrolled in Community Living Assistance Services and Supports (CLASS) longterm care program, unless they opt out Rating reforms for Individual and Small Group Cost-sharing for preventive services in Medicare eliminated Limit FSA contributions to $2,500 per year 2018 High-cost insurance tax – 40% on single coverage over $10,200 and family coverage over $27,500 Employer mandate Insurance exchanges, with subsidies up to 400% of the federal poverty level Medicaid expansion Insurer fee, $8B, increasing to $14B in 2018 18 For relevant internal audiences Effective Dates of Reform Provisions 2010 Rate justification New product requirements (dependents to age 26, no lifetime limits, etc.) Individual market rescission reform Prohibition on pre-ex exclusion for children Early retiree reinsurance program Federal-required high risk pool Tax credits for small employers Insurer compensation cap on deductibility of $500,000 per year Coverage of recommended preventive services Internet comparison shopping tool Consumer appeal process (inc. ASO) No benefit differences by employee salary Grants for states to enhance health insurance ombudsman programs 2011-2013 2014 Medical loss ratio requirement – 80% for Individual and Small Group; 85% for Large Group beginning in 2011 Individual mandate Medicare Advantage cuts Rating reforms for Individual and Small Group Grants for small employer wellness programs Increased tax on nonqualified medical expenses for Archer Medical Savings Accounts Quality initiative reporting Limit FSA contributions to $2,500 per year Uniform coverage summaries Standard terms and conditions Employer mandate Individual market guarantee issue 2018 High-cost insurance tax – 40% on single coverage over $10,200 and family coverage over $27,500 Expands Small Group from 2-50 in most states to 1-100 Insurance exchanges (with government-run plan), subsidies up to 400% federal poverty level New product framework Medicaid expansion Insurer fee, $8B, increasing to $14B in 2018 19 For relevant internal audiences Insurance Reforms / Plan Requirements Plan Years Beginning Enactment 3/23/10 June/July ’10 • Review of “unreasonable” rates • National high risk pool • HHS web portal • Temporary employer reinsurance Sept 2010+ 2014 • No pre-ex for kids* • GI/CR • Dependent coverage to 26* • Age band (3:1) • Limits on rescissions • Risk adjustment • Internal/external appeals* • Exchanges • MLRs (80% individual/ small group; 85% group) • SG = 1-100 • No lifetime limits* • No preventive cost-sharing* * Impact all plans • Patient protections* 20 What It Means for You: Implications for our customers ▪ No immediate changes to benefits, premiums, physician or hospital networks ▪ Future impacts will vary depending on product type and company size ▪ Legislation will be phased in over several years, and many provisions require federal agencies to issue more detailed regulations ▪ Premiums may be impacted in future 21 Delete this slide if not relevant to audience What It Means for Large Groups Effective in 2010: ▪ New product requirements at renewal after 9/23/10 ▪ Early retiree reinsurance for certain eligible early retirees Effective in 2011: ▪ Employees automatically enrolled in Community Living Assistance Services and Supports (CLASS) long-term care program, unless they opt out Effective in 2013: ▪ Tax deduction for Medicare Part D retiree drug subsidies eliminated ▪ Flexible Spending Account (FSA) contributions limited to $2,500 per year Effective in 2014: ▪ Employer mandate (with auto-enrollment) ▪ Products must meet new requirements, 60% actuarial value ▪ Health Insurance Exchange vouchers required for some employees Effective in 2018: ▪ High-cost insurance tax – 40% on Single coverage over $10,200 and family coverage over $27,500 22 Delete this slide if not relevant to audience What It Means for Small Groups Effective in 2010: ▪ New product requirements for renewals after 9/23/10 ▪ Tax credits for certain employers Effective in 2011: ▪ Grants for wellness programs ▪ Employees automatically enrolled in Community Living Assistance Services and Supports (CLASS) long-term care program, unless they opt out Effective in 2013: ▪ Limits Flexible Spending Account (FSA) contributions to $2,500 per year Effective in 2014: ▪ Elimination of premium rate variables may result in a significant premium increase or reduction ▪ New product requirements, prohibition on deductibles over $2,000/$4,000 ▪ Health insurance exchange as new sales channel ▪ New taxes built into premium costs Effective in 2018: ▪ High-cost insurance tax – 40% on Single coverage over $10,200 and family coverage over $27,500 23 Delete this slide if not relevant to audience What It Means for Individual Members Effective in 2010: ▪ New product requirements for renewals after 9/23/10 Effective in 2014: ▪ Rating reforms with weak individual mandate will lead to substantial premium increases for many members ▪ New product requirements with new framework ▪ Health insurance exchange as new sales channel ▪ New taxes built into premium costs 24 Delete this slide if not relevant to audience What It Means for Senior Members Effective in 2010: ▪ $250 rebate to offset the Part D “donut hole” • Coinsurance rate phases down to 25% by 2020 Effective in 2011: ▪ Reductions to Medicare Advantage program payments, which may result in reduced benefits and/or increase member cost-sharing ▪ Cost-sharing for preventive services in Medicare eliminated ▪ Discounts on prescriptions in the Medicare Part D “donut hole” begin to phase in 25 Delete this slide if not relevant to audience What It Means for Brokers Effective in 2010: ▪ Grandfather provision requires all products renewed after September 23, 2010 to: • Allow members to add dependents up to age 26 regardless of student status • Eliminate lifetime limits on policies ▪ For new sales and subscribers who change policies after 3/23/10, we will be required to make additional changes beginning in approximately six months, such as removing any member cost sharing for "preventive" benefits, as defined by the legislation. Effective in 2014: ▪ Health insurance exchange will exist as a new sales channel for individual and small group 26 Some Early Impacts: Employers Facing New Expenses Major American companies say they will face hundreds of millions of dollars in new health care costs: ▪ AT&T ($1 billion charge in 2010) ▪ Deere & Company ($150 million charge in 2010) ▪ Caterpillar ($100 million charge in 2010) ▪ 3M Company ($85-90 million charge in 2010) Source: Associated Press articles, March 2010 27 Some Early Impacts: Legal Challenges The legislation faced immediate legal challenges from several parties: ▪ At least 21 states ▪ Association of American Physicians and Surgeons (AAPS) ▪ New Jersey Physicians Inc. Source: FierceHealthcare news, March 30, 2010 28 Agenda ▪ Legislative overview ▪ What it means for you ▪ Continuing need for reform ▪ How to stay informed 29 Medical Costs Continue to Rise U.S. National Health Expenditures (trillions) $3.0 10% 8.6% 9.0% 9% 8.3% $2.5 $2.40 (P) 8% $2.24 $2.11 6.9% $2.0 $1.98 7.0% $1.85 $1.73 6.8% 7% 6.7% $1.60 $1.5 6.1% 6.1% (P) $1.47 6% 5% $1.35 4% $1.0 3% 2% $0.5 1% $0.0 0% 2000 2001 2002 2003 2004 2005 2006 2007 2008 (P) Source: National Health Expenditure Accounts, CMS 30 Profit Misperceptions Delete this slide for external presentations How much profit do consumers think insurers make? A. Less than 5% B. 15% C. 30% D. 50% 31 Profit Misperceptions Delete this slide for external presentations Many consumers have an inaccurate perception of health insurer profits % profit % consumers 41%+ 25% 31-40% 15% 21-30% 20% 11-20% 21% 6-10% 0-5% 40% of consumers surveyed think we make a profit of 30% or more. 14% 6% 32 Where Does Your Health Insurance Dollar Go? 33 Hospital Cost-Shifting Aggregate Hospital Payment-to-Cost Ratios, 1981-2006 Cost shift Source: Avalere Health analysis of American Hospital Association Annual Survey data, 2005, for community hospitals. (1) Includes Medicaid Disproportionate Share payments. 34 Lessons From Massachusetts The results from Massachusetts demonstrate continued need to implement responsible reform that addresses cost and quality: ▪ Covered about half of the uninsured (already exhibited lowest uninsured rate in U.S.) ▪ Premium costs for individuals in Massachusetts are the second highest in the U.S. ▪ Overall, the costs of Massachusetts health reforms have been much higher than expected ▪ Lack of an effective, enforceable individual mandate only exacerbates the cost issue in Massachusetts, and there is evidence of enrollment gaming 35 Agenda ▪ Legislative overview ▪ What it means for you ▪ Continuing need for reform ▪ How to stay informed 36 Implementation Communications ▪ Several teams are working on implementing the various provisions with 2010 and 2011 implementation dates ▪ We will be sending communications to employers, individuals, and brokers about upcoming changes 37 Health Action Network ▪ One-stop platform to follow and participate in the debate on health care reform ▪ Contact Members of Congress ▪ Register to receive weekly news on health care reform ▪ Tell others about the Health Action Network www.HealthActionNetwork.com 38 Health Action Network on Facebook ▪ Articles and dialogue about health care reform ▪ Take Action tab allows for conversions from fans to advocates ▪ Interactive widget allows fans to easily promote health care reform to their friends www.facebook.com/thehealthactionnetwork 39 Anthem Blue Cross and Blue Shield is the trade name of: In Colorado and Nevada: Rocky Mountain Hospital and Medical Service, Inc. In Connecticut: Anthem Health Plans, Inc. In Indiana: Anthem Insurance Companies, Inc. In Kentucky: Anthem Health Plans of Kentucky, Inc. In Maine: Anthem Health Plans of Maine, Inc. In Missouri (excluding 30 counties in the Kansas City area): RightCHOICE® Managed Care, Inc. (RIT), Healthy Alliance® Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. RIT and certain affiliates only provide administrative services for selffunded plans and do not underwrite benefits. In New Hampshire: Anthem Health Plans of New Hampshire, Inc. In Ohio: Community Insurance Company. In Wisconsin: Blue Cross Blue Shield of Wisconsin ("BCBSWi"), which underwrites or administers the PPO and indemnity policies; Compcare Health Services Insurance Corporation ("Compcare"), which underwrites or administers the HMO policies; and Compcare and BCBSWi collectively, which underwrite or administer the POS policies. Independent licensees of the Blue Cross and Blue Shield Association. ® ANTHEM is a registered trademark of Anthem Insurance Companies, Inc. The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. 40