Basic Pulmonary Anatomy
advertisement

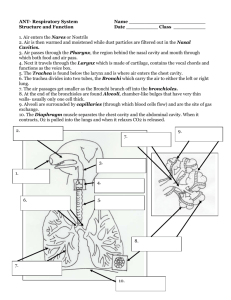
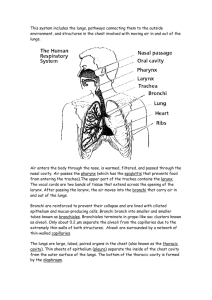
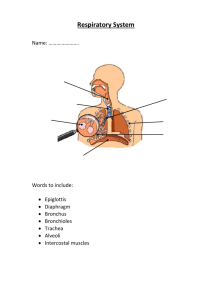
Basic Pulmonary Anatomy The Upper and Lower Airways Respiratory System Upper Airways Nose Paranasal sinuses Pharynx The Functions of the Nose Filter the air Humidify the air Warm the air Site for sense of small To generate resonance in speech The Nose Rigid structure composed of cartilage and bone Septal cartilage divides nasal cavity into two nasal fossae Palate divides nasal cavity and oral cavity Nose divided into 3 regions Nasal structure Nares and Nasal Cavity Regions of the nose Nares or nostrils serve as opening for the nasal fossae—two cavities in middle of the face Vestibule/vestibular region Lined with stratified squamous epithelium Contain vibrissae-nasal hair, first line of defense, function to filter inspired air Sagital section of the head Nasal regions Vestibular area contains sebaceous glands; secrete sebum Keeps vibrissae soft and filter gases Olfactory region: pseudostratified columnar epithelium and olfactory cells Regions of the nose Respiratory—highly vascular; ciliated, pseudostratified columnar epithelium Contains turbinates or conchae; increase surface area (166 cm2) for humidification, heating/cooling and filtering of air Mucous membranes provide up to 6501000 ml of water/day to humidify air Respiratory region of nose Goblet cells in mucus membrane secrete 100 ml/day of mucous; aids in trapping inspired particles and prevents them from entering lower respiratory trace Each columnar cell contains 200-250 cilia; beat in waves toward oropharynx (mouth), 2cm/min Sinuses Air-filled cavities within the skull (cranium) Aka paranasal sinuses (four pairs) Function not clear, lighten head and provide voice resonance Lied with pseudostratified cliated columnar epithelium and goblet cells Paranasal Sinuses Oral Cavity Alternate respiratory passage Anterior 2/3 of tongue located in oral cavity Another “respiratory” muscle Lined with stratified squamous epithelium +Pharaynx (Throat), hollow, upper portion of the airway and the digestive tract Subdivided into: nasopharynx, oropharynx, laryngopharynx Nasopharynx Pseudostratified ciliated columnar epithelium Pharynx Nasopharynx Filters bacteria and foreign particles from inspired air Carries this to the stomach Eustachian tube and auditory tube open into lateral surfaces, connect nasopharynx to middle each, equalizes pressure of middle ear Nasopharynx Oropharynx Between soft palate above and base of tongue below From tip of uvula to epiglottis Stratified squamous epithelium Gas conduction, filtering of air Defense mechanism: gag reflex Oropharynx Laryngopharynx Stratified squamous epithelium Gas conduction Connecting zone between upper and lower airway (vocal cords and below) Lower Airway Begins with true vocal cords and extends to alveoli Larynx Trachea Main stem bronchi Segmental bronchi Subsegmental bronchi Bronchioles Terminal bronchioles Respiratory bronchioles Alveolar ducts Alveolar sacs alveoli Larynx Lies between base of tongue and trachea Protrusion is the thyroid cartilage, aka “Adam’s apple.” Houses the vocal cords, primary use is vocalization Connection point-upper and lower airways Larynx Larynx Extends from C3 to C6 Pseudostratified ciliated columnar epithelium Functions: Free flow of air to the lungs During inspiration, vocal folds abduct, move apart, and widen glottis Valsalva maneuver and Muller maneuver Larynx Composed of 3 single cartilaginous structures: Epiglottis-flap, swings down to meet larynx during swallowing Thyroid-bulk of this forms larynx Cricoid-circular, keeps head of trachea open Larynx Posterior view Epiglottis Covers the rima glottidis during swallowing (glottis=cords & space) Larynx has poor lymphatic drainge, prone to edema Epiglottitis is a life-threatening condition (supraglottic croup), bacterial origin Narrowest part of lower airway in adult Glottis Thyroid Largest of the laryngeal cartilages Primary housing the vocal cords Inflammation below the vocal cords known as laryngotracheobronchitis Croup Subglottic croup Viral orgins Cricoid A complete cartilaginous ring Narrowest portion of the lower airway in a neonate and infant Actual start of the lower airway Larynx – superior view Tracheobronchial Tree Series of branching airways commonly referred to a “generations” or “orders” The first generation or order is zero (0), the trachea itself. Bifucrates at the carina Two Types of Airways Cartilaginous -serve only to conduct air between external environment and the sites of gas exchange Non-cartilaginous -serve both as conductors of inspired air and as sites of gas exchange Tracheobronchial Tree Dichotomous branching (daughter branches) Airways become progressively narrower, shorter, and more numerous Cross-sectional area enlarges Common histology (at the nose) and throughout until the bronchiole generation Histology Three major layers Epithelial lining Lamina propria Cartilaginous layer Histology Tracheal lining Pseudostratified columnar epithelium with cilia; goblet cells, serous cells, and specialized submucosal bronchial glands 200+ cilia per cell, 5-7 microns long Beat cephalid (head) toward oropharynx Tracheal Lining Epithelial lining Pseudostratified ciliated columnar epithelium is homogenous until the level of the bronchioles Cilia disappear in terminal bronchioles Cilia absent in respiratory bronchioles Histology Mucous blanket Covers the epithelial lining Composed of -95% water -glycoproteins Carbohydrate lipids DNA Cellular debris Mucous Mucus produced by Goblet cells Found through terminal bronchioles Submucosal (bronchial) glands extend into laminar propria Innervated by vagus nerve (parasympathetic) Produce 100 ml of secretions/day Disappear at end of terminal bronchioles Mucous Blanket Two distinct layers Sol layer Gel layer Cilia move through sol layer and strike gel layer propelling it toward mouth At a rate of 2 cm/minute Mucocilliary Escalator Defense mechanism of lower airways Mucus propelled up airway to larynx Cough mechanism moves secretions into oropharynx via sheering forces Mucociliary transport & cough Factors Which Slow Mucocilliary Transport Cigarette smoke Dehydration Positive pressure ventilation Endotracheal suctioning High inspired oxygen concentrations Hypoxia Atmospheric pollutants General anesthesia Parasympatholytic drugs Lamina Propria Submucosal layer Contains loose fibrous tissue with Tiny blood vessels Lymphatic vessels Branches of the vagus nerve Two sets of smooth muscle fibers which continue/extend down to alveolar ducts Lamina propria Mast cells Found in lamina propria near Branches of vagus nerve and blood vessels Scattered throughout smooth muscle Loose connective tissue of skin and intestinal mucosa Cell constituents of submucosal glands Important part of humoral immune response (circulating antibodies) which defend against antigens Mast Cells Release histamine Cartilaginous Layer Outermost layer of tracheobronchial tree Consist of Trachea Mainstem bronchi Lobar bronchi Segmental bronchi Subsegmental bronchi Trachea 10-12 cm long 1.5-2.5 cm wide Extends to second rib anteriorly and T4T5 posteriorly 15-20 C shaped rings Main Stem Bronchi Right bronchus Wider More vertical 5 cm shorter Supported by C shaped cartilages 20-30 degree angle First generation Left bronchus Narrower More angular Longer Supported by C shaped cartilages 40-60 degree angle First generation Lobar Bronchi R main stem divides into: Upper lobar bronchus Middle lobar bronchus Lower lobar bronchus L main stem divides into: Upper lobar bronchus Lower lobar bronchus Segmental Bronchi 3rd generation R lobar divides into Segmental bronchi 10 segments on right L lobar divides into Segmental bronchi 8 segments on left Subsegmental Bronchi 4th to 9th generations Progressively smaller airways 1-4 mm diameter At 1 mm diameter connective tissue sheath disappears Noncartilagenous Airways Bronchioles 10-th to 15th generation Cartilage is absent Lamina propria is directly connected with lung parenchyma Surrounded by spiral muscle fibers Epithelial cells are cuboidal Less goblet cells and cilia With no cartilage, airway remains open due to pressure gradients Terminal Bronchioles 16th to 19th generation Average diameter is 0.5 mm Cilia and mucous glands begin to disappear totally End of the conducting airway Canals of Lambert-interconnect this generation,provide collateral ventilation Gas exchange zone Respiratory bronchioles Acinus (aka primary acinus; aka primary lobule)—respiratory bronchioles to the alveoli Ducts, sacs, alveolar Squamous epithelium The Functional Units of Gas Exchange Functional Units of Gas Exchange Three generations of respiratory bronchioles Three generations of alveolar ducts 15-20 clusters--sacs Gas exchange terminology All of the structures arising from a single terminal bronchiole are called Primary lobule Acinus Terminal respiratory unit Lung parenchyma Functional units Acinus/Primary lobule Respiratory bronchioles with some alveoli arising from their walls Alveolar ducts arise from respiratory bronchioles--alveoli whose septal wall contain smooth muscle Alveoli Ca. 300 million alveoli Between 75 µ to 300 µ in diameter Most gas exchange takes place at alveolar-capillary membrane Anatomic Arrangement of Alveoli 85-95% of alveoli covered by small pulmonary capillaires The cross-sectional area or surface area is approximately 70m2 Acinus or Lobule Each acinus (unit) is approximately 3.5 mm in diameter Each contains about 2000 aveloli Approximately 130,000 primary lobules in the lung Acinus Alveolar epithelium Two principle cell types: Type I cell, squamous pneumocyte Type II cell, granular pneumocyte Type I Cell 95% of the alveolar surface is made up of squamous pneumocyte cells Between 0.1 µ and 0.5µ thick Major site of gas exchange Type II Cell 5% of the surface of alveoli composed of granular pneumocyte cells Cuboidal in shape with microvilli Primary source of pulmonary surfactant Involved with reabsorption of fluids in the dry, alveolar spaces Type II Pneumocyte Pore of Khon Small holes in the walls of adjoining alveoli (alveaolar septa) Between 3 to 13 µ in diameter Formation of pores may be due to: Desquamation due to disease Normal degeneration due to aging Movement of macrophages leaving holes Canals of Lambert/Pores of Kohn Provide for collateral ventilation of difference acinii or primary lobules Additional ventilation of blocked units May explain why diseases spread so quickly at the lung tissue (paremchymal) level Pores of Kohn Alveolar macrophages So-called Type III cell Remove bacteria and foreign particles May originate as Stem cells precursors in bone marro Migrate as monocytes through the blood and into the lungs Intersitium/interstial space Surround, supports, and shapes the alveoli and capillaries Composed of a gel like substance and collagen fibers Contains tight space and loose space areas Alveolar-Capillary Site-Interstitial Space Interstitium Water content in loose space can increase by 30% before there is a significant change in pulmonary capillary pressure Lymphatic drainage easily exceeded Collagen limits alveolar distensibility Area of scarring, making for stiffer or non-compliant lungs Blood Supply to the Pulmonary System Two Systems Bronchial Blood Supply Bronchial arteries From aorta to temrinal bronchioles Merge with pulmonary arteries and capillaries 1% of total cardiac output (left ventricle) Bronchial arteries Also nourish Mediastinal lymph nodes Pulmonary nerves Some muscular pulmonary arteries and veins Portions of the esophagus Visceral pleura Bronchial venous system 1/3 blood returns to right heart Azygous Hemiazygous Intercostal veins This blood comes form the first two or three generations of bronchi Bronchial venous return 2/3 of blood flowing to terminal bronchioles drains into pulmonary circulation via “bronchopulmonary anastomoses” Then flows to left atrium via pulmonary veins Contributes to “venous admixture” or “anatomic shunt” (ca. 5% of C.O.) Pulmonary Vascular System The second source of blood to the lungs Primary purpose is to deliver blood to lungs for gas exchange Also delivers nutrients to cells distal to terminal bronchioles Composed of arteries, arterioles, capllaries, venules, and veins Pulmonary Capillaries Walls are les than 0.1µ thick Total external thickness is about 10µ Selective permeability to water, electrolytes, sugars Produce and destroy biologically active substances Lymphatic System Lymphatic vessels remove fluids and protein molecules that leak out of the pulmonary capillaries Transfer fluids back into the circulatory system Lymphatics Lymphatic vessels arise within loose spaces of connective tissue Vessels then follow bronchial airways, pulmonary airways, pulmonary arteries and veins to the hilum Lymphatics Vessels end in pulmonary and bronchopulmonary lymph nodes within and outside of lung parenchyma Nodes acts as filters to keep particles and bacteria from entering the blood Lymphatics Lymphatic vessels are not in the walls of the alveoli. Within the interstial spaces to help drain fluids and foreign materials. More lymphatic vessels on surface of lower lobes than on upper and middle lobes (dependent portions) Lymphatic vessels Thoracic duct carries lymph fluid coming from tissues inferior to diaphragm and from left side of upper body Eventually empties into left subclavian vein Lymphatic vessels Right lymphatic duct drains the right half of the body superior to the diaphragm Empties into the right subclavian vein