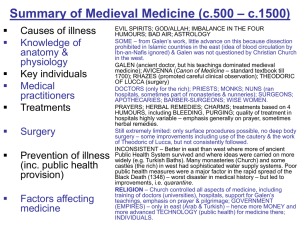
Middle Ages - South Newcastle Trust
advertisement

Medicine Through Time Key Time Periods • Ancient Greece • Ancient Rome • Middle Ages • Renaissance • Industrial Revolution • Twentieth Century to Present Day Key Themes Progress- Change which leads to improvements. Change- When things become different. Regress- Change which leads to decline. Belief- What a person accepts as true, including faith in God. Continuity- When things don’t change. Chance- When something which hasn’t been predicted happens. Factors Affecting Medicine Religion War Chance Communications Individuals Education Government Technology Sometimes, these factors helped the development of medicine and sometimes they hindered it. Greek Medicine 1500BC-200BC • Greek Empire was strong and successful. They took over the Egyptian Empire, gaining the knowledge they had. Beliefs • The beliefs believed in Gods for almost all aspects of life. • Poseidon, the God Of The Sea • Ares, God Of War • Asclepius, God Of Healing Asclepius • Temples were built to him, called Asclepius. • They believed that if sick people went to sleep in an Asclepion, Asclepius and his daughters would visit him in there dreams and cure them- placebo effect? • Asclepions had baths, gyms, libraries and temples to visit the gods. • ‘Simple’ surgeries were performed. Theory Of Four Humours • Aristotle came up with the theory. • Hippocrates developed it further. • It was incorrect but it was used for 2,000 years. • ‘Humours’- Liquids Air Fire Spring Summer Blood Yellow Bile Earth Hippocrates: Who Was He? General Information: • Born c.460BC-c.370BC • Born on the island of Cos. • He worked as a doctor and a teacher of doctors. • However, little else is known about him. The Hippocratic Oath • The Hippocratic Oath was made to give people confidence and trust in doctors. • It makes clear that doctors are not magicians. • It makes sure that doctors keep high standards of treatment, behaviour and work for the benefit of their patients (not to make themselves wealthy). The Hippocratic Collection Of Books • It is thought that Hippocrates probably wrote some of the books known as the Hippocratic Collection. • Many of the books were written by other doctors. • It is an important collection of books because it is the first detailed list of symptoms and treatments. • Doctors continued to use the theories and methods in these books for many centuries. The Four Humours Water Autumn Winter Black Bile Phlegm • People believed that it was an imbalance in humours that made people ill (too much or too little of a humour) • From what we know now, there was confusion between symptoms and causes. • The Theory Of Four Humours was the idea that the body is made up of four humours (liquids)- blood, black bile, yellow bile and phlegm). • They believed that when people were healthy and well, the fours liquids were balanced. • When people were ill, it was thought that it meant that there was an imbalance of the liquids. • When there was an imbalance they believed that certain things happened to the body to get rid of excess liquid: Blood- nose bleed Black Bile & Yellow Bile- sick Phlegm- Coughing, sneezing etc. Observations & Recordings • Hippocrates showed that it was important to observe and record the symptoms and development in diseases. • This had two advantages Doctors were more likely to choose the right cure if they took care to find the cause of problems. Notes could then be used to help with diagnoses and treatment for future patients. Natural Treatment • Hippocrates encouraged doctors to look for natural treatments for illnesses rather than praying to the gods for help. • He believed in giving natural treatments for natural causes. • Many were told to rest and eat healthily and, when the patients were stronger, to do gentle exercise. Keeping Healthy • Hippocrates emphasised the importance of helping people stay healthy. • He recommended a light diet, gentle exercise and rest to keep the body’s humours balanced. Hippocratic Oath “I swear by Apollo, Asclepius and by all the gods that I will carry out this oath. I will use treatment to help the sick according to my ability to and judgment but never with a view to injury of wrongdoing. I will never give poison to anybody. Whatever I see or hear professionally will be kept secret.” Roman Medicine Public Health Why It Was Needed: • They needed a strong, fit, healthy army to defend and expand the empire. • They built forts to house their soldiers away from swamps and marshes. They were also close to water. • Each fort had a bath-house with drains and fresh water. • Army hospitals were also built for the soldiers. • Soldiers got the best treatments possible from trained doctors and surgeons. • They used herbs, simple surgery, rest, diet and exercise“A healthy army means a healthy empire!” • People soon realised that these ideas could then be used in the City Of Rome itself. Benefits Of Public Health • Forts had sewers, a good water supply, a hospital, toilet blocks (latrines). • Fresh water was delivered to towns. • Few had toilets that emptied directly into the sewers- this way they could use pots to empty into the sewers and rivers. • Public health- provided for towns and villas. • Channels travelled through towns to baths and water tanks. Problems With Health Facilities • Disease was easily spread if bath-houses were not kept clean. • Health facilities were only available in towns or larger areas (like cities) and so in other areas families had to sort themselves out. Nothing was organised by local rulers. • Sewers were often open or built close to the surface and this spread disease. • Fort Latrines were only available to soldiers. • There was poor water flow through the sewers if it did not rain. • Lead poisoning (from the pipes). • Sewers- released bad smells and spread diseases. • Stone sewers were better than timber sewers and were often used in the bigger towns. However, the water did not flow through quickly and so left bad smells and spread disease. How Effective Was Public Health In Roman Times? On one hand, public health was effective because it provided many people with facilities where they could clean, drink and find treatment which before public health they could not have had and also paved the way for the facilities available in modern day society. However, due to occasional lack of rain, open sewers and baths that only had clean water in them once a week, there were problems. Many people contracted, and ultimately died from, disease and people who didn’t live in towns or cities were not given these facilities at all. For Britons, the Romans brought new treatments such as bloodletting – if they could afford to see a physician. However, if most people became ill they relied on the old herbal remedies and prayed to their gods to make them well. This meant if you became ill, your chances of recovering were little better than before the Romans arrived. In conclusion, although public health has contributed to modern medicine in a big way and provided some help for people’s health back then, at the time it did not benefit many people. Roman Ideas The Romans also brought one system of government to the whole of their conquered territory in Britain. The Romans had different explanations for disease: • Supernatural reasons – curse or gods • Caused by bad air from swamps or places with bad smells (they realised that hygiene was linked to health, although they didn’t understand why) • Imbalance of a person’s humours. Treatments Very few doctors in Roman Britain, most illnesses treated at home – usually by the father of the family, who would use remedies passed down by his father. People who could afford and had access to a doctor were treated in their own homes too. Some hospitals, mainly in forts that were reserved for soldiers. Often equipped and provideddjdjd excellent training for surgeons and doctors. However, there were few hospitals open to the public, so little impact on ordinary people. Many people visited a temple to make offerings to gods. People also visited public baths as it was believed they had heeling properties. Pregnant women relied on other women to help them. Some became experienced and were used as midwives. The Romans believed that diet, exercise and rest were very important in treating illness and would also use bloodletting and purging, but the Romans would mix these practical remedies with prayers and offerings made to Salus, the god of health. Public Baths Admissions to the baths were not free but it was cheap enough for most people to attend and many visited every day. The baths served a variety of functions: • Social – Place for people to meet, both for business and pleasure. • Hygiene – people could keep clean. • Exercise – they provided places where people could keep fit. The Romans were big fans of being fit and strong. • Medical – They believed the waters had healing powers, so people with illnesses regularly visited the baths. Water and Waste Sanitation was important the Romans built sewage systems which took waste away from public baths, toilets and houses and emptied in rivers away from town. Water and sewers were far better than anything Britain had seen. Many people could stay healthy and did prevent some disease. However, most towns and cities had open drains. Also, when water supply low not enough for the sewers to work properly and waste would build up. Good quality roads made travel and therefore communication easier and quicker. Central control from Rome and regular changes of officials kept Britain up to date with new ideas. Knowledge and ideas spread as people travelled throughout the empire. Who Could You Get Medical Help From? Home Remedies • Most asked mum for help- they had a vast knowledge of medical treatments handed down from one generation to the next. • Many specialised in herbal remedies which were mainly made from plants. Some were made out of animal fats and minerals. • Many remedied helped- otherwise people would not have kept using them. • We now know that honey can kill infections- they used it in many remedies. • Romans brought new plants to Britain to use in medicines. • The wealthy people would go to their father (the head of the household). He would look up treatments in a medical book (such as the huge compendium of herbal cures which was collected by Dioscordes). • Modern scientific tests show that at least 20% of remedies contained ingredients like honey and garlic which helped patients by killing bacteria in infections. • The books might have also advised people on what to do once they had recovered. One medical encyclopaedia was Artes, ‘The Sciences’ by Celsus (a wealthy landowner who built up his knowledge partly through treating family and friends). • Celsus stressed the importance of exercise for avoiding illness. • ‘He who has been busy during the day, whether in domestic or public affairs, ought to put aside some part of the day for the care of the body. The most important way to care for the body is through exercise, which ought to come to an end with sweating.’ • This was only for the wealthy; poor people would probably have needed to get back to work. Gods And Their Priests • When sick, you wouldn’t just take medicine. • You might have worn a charm (to ward of evil spirits). • You would definitely have prayed to your household Gods for good health and cure. • You would also pray to the Gods of healing- the greatest of these being Asclepius. • People who could not get rid of their illness would go to a temple to see the Gods’ priests and to seek help. • Sometimes people would leave small carvings of the sick part of the body. • Some temples had bath-houses, guesthouses, covered courtyards and an abatom where people could sleep and be visited by Gods in their dreams. • The priests also probably encouraged patients to do exercise, cleanse themselves in the baths and to build up strength by eating regular meals and having plenty of rest. Trained Doctors • If mum’s herbal remedies and your prayers did not get rid of the illness, you could see a trained doctor. • This would probably have cost money. However, many towns in the Roman Empire employed doctors to treat the poor- this may have happened in Britain too. • Some of the doctors were women. • Mainly doctors trained by acting as apprentices to experienced doctors. This was not always a good thing. Sometimes, doctors had so many apprentices, that they themselves spread disease and stopped patients from getting better. Having A Baby • Women cared for each other during childbirth. • Many became very experienced and often acted as midwives. • According to medical writer Soranus, the best midwives were intelligent, robust, respectable and literate and experienced in nutrition, pharmacy and surgery. • Handbooks on midwifery emphasised the importance of cleanliness (listing the need for oil and hot water for cleansing, sponges, wool coverings and bandages). • However, midwives had no technical methods of helping if there were problems during birth. • One method was for four people to take hold of the mother and shaker her violently ten times to speed the birth. • Pliny the elder suggested reducing labour pains by hurling a projectile, preferably a cavalry spear, three times over the roof of the house. Galen General • • • • • • • • • Claudius Galen AD129 in Greece (modern day Turkey) He worked as a doctor Started studying medicine at the age of 16 (was a medical student) He studied at the medical school in Alexandria Worked as a surgeon at a gladiators’ school He was doctor to the Roman Emperor from AD162 Was a teacher of doctors Galen- uses Hippocrates theories and anatomy Galen’s Work • • He was most famous for his books. He combined Greek ideas + what he learned from his work in Alexandria. • He also believed in careful observation of patients. • He also developed Hippocrates's idea of the ‘Four Humours’ with his own ideas of ‘Opposites’. • He was interested in dissection and surgery Four Humours + Diagnosis • When it comes to the theory of Four Humours, like Hippocrates, Galen believed that illness was caused by an imbalance of the humours. • Observation- Like Hippocrates, he told doctors to observe and examine patients carefully and record patients’ pulse and make detailed notes. • In AD167, he made detailed notes on the Plague- how his patients had fever, thirst, diarrhoea, skin rashes an spat blood. • His notes were so thorough that the plague became known as ‘Galen’s Plague’. Treatments • Galen followed Hippocrates by giving advice on diet and exercise (to stop illness). • His most common treatment was bleeding patients to restore the balance of the humours. • Used this technique a lot more than Hippocrates did ( Hippocrates preferred to interfere with the body as little as possible). • Galen developed the idea of ‘Opposites’ in order to balance the humours. E.g. If someone had lots of phlegm ( a problem related to the cold) they would be advised to eat something hot (like a chilli pepper) . On the other hand, if it was a heat related issue, Galen would give them a treatment, or tell them to eat something, with something cold in it (like cucumber). Anatomy & Dissection • Hippocrates did not do much work on anatomy and did not say that dissection was important. • Galen disagreed. • He believed that physicians should find out as much as possible about the structure and the workings of the body (and if possible to dissect bodies). • If this was not possible, he advised doctors to dissect apes (because they were more like humans). • • • • • He showed his discoveries about the workings of the nervous system by dissecting a pig. Although he often had to dissect animals, not humans, Galen’s discoveries were important. He proved that the brain (not heart) controlled speech and that the arteries, not just the veins, carried blood around the body. He did make mistakes because the bodies of apes and pigs are not the same as humans. It was well over 1000 years before people dared to challenge his findings. • The dissection of human bodies was not forbidden it was just not done in those days; the Church did not agree with it. Books & Influence/Legacy • He wrote thousands of books covering every aspect of medicine in a detailed and well-organised way. • It included the work of earlier doctors (such as Hippocrates) as well as his own knowledge on treatments, the structure and the workings of the body. • He covered everything and so people believed that his books had all the answers- this was one reason why his books became the basis for medical training for over 1000 years. • Another reason- His ideas fitted in with the ideas of the Christian Church (which controlled education in Europe during the Middle Ages). • Galen was not Christian but he did believe that the human body had been created by God who had made all the parts of the body fit together perfectly- this matched the Christian belief that God had created human beings and so for centuries, Christians did not dare question Galen’s ideas. What Developments Were Made By Galen During Roman Times? Galen made various developments during his time. Firstly, Galen thought that learning about anatomy and doing dissections was very important. He developed his knowledge in this area by dissecting animals (such as apes and pigs). One of his ideas was that the brain, not the heart, controls speech and so proved this by publically dissecting a pig. He also developed the idea that the arteries (not the veins) carry blood around the body. This meant that Galen had proved early ideas to be incorrect and had also been able to develop ideas about various aspects of the body and so widen the knowledge about the entire body. Secondly, Galen wrote over a thousand books which covered every aspect of medicine. As well as using work by earlier doctors, he also included his own work and developments. Because his books covered everything, many people believed him. They also believed him because he developed, and believed in the idea that the human body was created by God. This was what the Christian Church believed in. Because he was able to write so many books, he was able to spread his theories about anatomy; this meant other people could investigate Galen’s ideas and could use his findings to continue developments on their own. Thirdly, Galen came up with the idea of opposites as a treatment or humour imbalances. This meant, for example, giving someone a hot chilly pepper to someone with too much phlegm (as a result of a cold) and giving a heat related imbalance a treatment of something cold (like cucumber). This meant that Galen did not only develop ideas about anatomy but he also developed ideas about treatments and their effects on the body. Middle Ages 400-1500AD Who Treated The Sick? • Looking after the sick was an important role of the Christian Church. • This led to many hospitals being founded by the Church in the Middle Ages. • St. Bartholomew's hospital- in London- was one of the first to be founded. • By 1400, there were over 500 hospitals in England. However, most of them only had 5 or 6 beds. • St. Leonard’s hospital in York was unusually large with 200 beds. • You could not go into hospitals if you had an infectious disease. • Hospitals were sometimes set up for particular cases (e.g. unmarried, pregnant women & for the ‘poor and silly person’.) • Leper houses were built outside of towns in order to separate victims of the disease from the healthy people. • Most hospitals were like modern day care homescaring for the elderly rather than treating the sick. Only 10% actually treated the sick, • Hospitals provided food, rest and prayer. • Nursing care was provided by nuns (and monks) who had a good knowledge of herbal remedies and other remedies taken from books drawn from their libraries. • All except the wealthy, when ill, would go to the woman of the household. • Like Roman Britain, women treated a vast majority of illnesses in the Middle Ages. • Women had a range of remedies. However, sometimes, the local wise women had to be called on to use her skills & knowledge. • Women acted as midwives. • Sometimes, women had to be apprenticed and gained licences through doing this. They were then paid for their work. • Women could also qualify as surgeons through apprenticeships. • Family links and connections contributed to giving women certain opportunities. • Katherine, a surgeon in London in around 1250- her father and brothers were also surgeons. • Women were not allowed to be physicians and they were not allowed to attend university either. Training Of Doctors • Everyone was poor & there were no towns; this meant that there were no trained doctors. • For hundreds of years, people relied on wise women and leeches. Wise women were trained through practice and were probably as good, or even better, as Roman doctors. • Between 1000-1300AD, Landowners started to become rich through the growing of their crops. • Bishops and abbot were the wealthiest and they spent their money on universities and cathedrals. • Universities trained physicians (the highest ranking of all the healers). It was expensive and so not many people did it. However, the pay was very good. • Medical students attended lectures and read books by Galen and other scholars (the works of other medical people like the Arab doctor ‘Ibn Sina/al-Razi’). • They were expected to memorise all of the books then Roger Bacon suggested they do their own research- he was thrown into jail because of this. • They also studies astrology because they believed that the body was affected by the movement of the planets. They though this caused illness. Understanding The Human Body How Did They Try To Stay Healthy? • • It was said to eat light meals, do gentle exercise (didn’t mention about sweating like the Romans did) to relax as often as possible, stay on good terms with neighbours and to send urine samples to the physician. • If they had too much of a humour, you’d either purge (take something to make yourself sick), bleed, bathe in hot water, build your house in a windy location t take away bad smells and avoid stressful noise. • • • • • • Physicians learned about astronomy; they dissected bodies as Galen did but nothing was learned by doing this. They believed that Galen’s books contained everything and so dissections were demonstrations of Galen’s descriptions and so they didn’t investigate further. The Physician was in charge but he did not do the dissection; the surgeon was told what to do. The physician told his assistant which of parts of Galen’s books to read. Students listened to the studies and watched the dissections but were not allowed to touch and do the dissections. Nothing new was learned and people respected traditional ideas and beliefs. Regular dissections were the start of a step forward. One day, someone would use dissection to make a new discovery to challenge Galen. What Did They Think Caused Diseases? • • • • • • • They believed that God or the Devil caused most diseases. Anglo Saxons believed that elves shot arrows (elf shot) and this caused diseases like head aches. They still believed in the Theory Of Four Humours . Universities taught about the Four Humours. Many people blamed things like bad air (miasma) for illnesses. Desperate explanations were made (e.g. outrageous fashion, children disrespecting their elders, minority groups and Jews). In some places, they burned Jews in order to get rid of disease. How Did They Treat The Sick? • Urine charts were used to determine the smell, colours and density of the patients urine. • Physicians may have also tasted it. • Wealthy people sent urine samples to physicians; this method fitted in with the Theory Of Four Humours. • Physicians followed Hippocrates and Galen by making careful observations and finding symptoms. • The Arab doctor al-Razi grouped illnesses. • Physicians needed to know astrology because they believed that parts of the body were linked to the Zodiac and the planets. • A bleeding chart showed where to take blood from; leeches were used to draw blood. • Bleeding was done to restore the balance of the four humours. • Ibn Sina (Avicenna)= famous Arab doctor • In Middle Ages Britain, the quality and development of medicine declines. • In the Arab world, at this time, medical qualities and development increased/improved. Did The Church Help Or Hinder Medicine In The Middle Ages? Help • • • • • Had doctors- people trusted them because they were provided by the Church. Some dissections were allowed to help teach students about anatomy and so discoveries could then be made. 1200 hospitals in England + Wales- many hospitals were founded and built by the Church. Provided medical care for the poor + elderly. They had a rule that said ‘care for the sick stands before all’- like Jesus helping them (doing as he would). Hinder • • • • • Some of their ideas did not work- like carving religious words onto the jaw as a treatment for tooth ache- they were wrong. They put Roger Bacon in prison (he challenged the Church’s medical ideas/theories. Dissections were frowned upon- the Church carried them out instead of doctors. This meant that discoveries made were limited. Dissections were based on Galen’s ideas which were incorrect. Only 10% of hospitals actually treated the sick or provided actual medical care. Judgement • I think that the Church did help medicine at this time because some dissections were allowed. However, for the most part, I think that the Church hindered medicine. I think this because most dissections weren’t allowed and, when they were allowed, they were carried out by the Church and not doctors. Also, out of all the hospitals they built, only 10% actually treated the sick. Furthermore, there was a general lack of understanding when it came to natural medicine. The Black Death What Was The Black Death? • The pestilence that caused it was the Bubonic Plague. • Bubonic Plague- carried by rats and spread by fleas. Fleas became infected when it bit an infected rat then it passed the disease onto other rats then to humans when they were bitten by the rats. • Symptoms- Sudden feeling of cold and tiredness. Then the discovery of painful swellings (buboes) on the armpit and groin. Blisters appeared all over the body followed by a high fever, severe head aches, unconsciousness for several days and then death. • Second disease- Pneumonic Plague. • This disease was spread by people coughing over others. • Victims coughed up blood because the disease attacked their lungs causing breathing problems. • Victims died more quickly- a day or two at most. What People Thought Caused It? • The pestilence comes from a privy toilet next to a chamber or some other thing that corrupts the air. • Sometimes comes from dead flesh or standing water in ditches. • Religious blame- God + Sins • England is struck by the pestilence because of the increasing pride and numberless sins of people’. • Unbalanced humours. • Jews- they were burnt in many countries. Jews were said to have poisoned water supplies. • Astrology- Movement and position of the planets. How Did People Try To Treat It? • Flagellants- Walked through towns as the plague spread, whipping themselves to show God that they had repented their sins and asking God to be merciful. • Advice- Avoid too much eating and drinking + avoid baths which open the pores. • In cold/rainy weather, light fires in your room. • Foggy or windy weather= inhale perfume every morning. • If the Plague arrived in hot weather- eat cold, drink more than you eat. Cucumber, fennel and spinach. • Stinking air- surround self with a terrible smell to ward off the bad air that carried pestilence. E.g. head in a bucket of waste from toilet and breath in the fumes for ½ hour. • King Edward III of England + bishops- ordered services and possessions to be held in every church at least once a day- In which people prayed for forgiveness + asked God to put and end to the disease. • Some went further- made candles their own height and lit them in Church as offering to God. E.g. Barcelonacitizens made a 7km trail of candles to encircle the city with the hopes of protecting the city. Why Did Public Health Deteriorate In The Middle Ages? Public Health 500AD- 1000AD General •Conditions did start to improve by 1200, houses (in London + York) were built on stone foundations. Some made entirely of stone. Cesspits were lined with brick or stone and so they were less likely to leak into the water supplies. • • • • • • • • • 1948- Pestilence arrived in Dorset. 1947- Europe arrival. Originated in China- from the rats on the ships. Estimated 40% population died from the disease. Dorset, Devon, Somerset- then to Bristol- very few people were left alive. Then it travelled north- leaving not a town or village or even, except rarely, a house without killing all/most of the people there. Shortage of people- not enough living to bury the dead. Bubonic Plague spread by fleas carried by rats. The disease began in China- then India- Then Europe. • Towns dirtier than Roman towns. • York was especially filthy. • Water (drink + cook) was collected from rivers and storage pits which were next to cess pits (sewage storage). • Pigs & chickens roamed the street. • Rats, mice and hawks scavenged. • Fish bones, animal dung, food waste and human faeces. • Animals were a big problem. • Horses were used as transport. • Cattle, sheep, geese constantly arrived for butchering. • The problems were, however, greater than the solutions • Medieval towns were dirtier than Roman towns. • Romans had army engineers with good technological knowledge. • Romans- wealth to afford aqueducts + public baths and slaves to do the building. • Even so, Romans had been no better at stopping the plague than then people in the Middle Ages. Problems • King collected taxes for the war instead of for cleaning the streets and building sewers. • There were not enough officials to punish all of those who broke laws. • Many Londoners did not pay the taxes required. • God sends the disease we suffer- what has illness got to do with dirty streets. Monasteries • • • • • • • • • • • • Best public health facilities were in the monasteries because they could afford it. Monks were better fed, did less physical work and had advantages. Water came to the Abbey through tanks. Water from the fish ponds flushed the latrines- which drained into the town ditches. Latrines were attached to the Monks’ dormitories. If the main water supply failed, there was a backup supply. Reservoirs stored water coming from the piping system. Drains took rain water and waste away. Pipes bringing water to supply the washroom, bakery, brew house, kitchen and fish pond. Roman Abbeys were a little like Roman forts- The water supply only benefited a small group of people- They couldn’t stop the plague. Middle Ages- Could use the facilities if they had the money. There were not animals this time but thousands of people were creating litter + waste all day everyday. Judgement: Which was better In The Improvement Of Medicine? The Romans Or The Middle Ages? Roman Britain was better Public health- MA had one to only a limited number of people Treatments + ideas about the causes of disease + training of doctors + methods of keeping healthy Hospitals for soldiers They were similar Medieval Britain was better Renaissance 1500- 1750 What Was The Renaissance? • Dissections- Were used in order to gain knowledge of the body. Through doing this, they were able to find out more about how the body worked. Students could go onto learn by watching and people could see and investigate first hand how the body worked and how it was made up. • Printing press- Clearer pictures and writing (books etc.) were available and so more people could learn more about anatomy without the need of doing/watching a dissection because the books could be sold all over the place and published in different languages. • Microscope- People could use them to see tiny things and so could look and study the body closely and precisely in order to learn more about it. Some Common Ideas • A cross on the front door- ward off plague • ‘New Herbal’ book- tummy ache • ‘Good Illustrations of Anatomy’ by Vesalius- popular book • Microscopes- To see detail you can not see with the naked eye • Bleeding- 4 humours • God sends plague down to punish our souls • Rhubarb Plague struck in 1665. The mayor of London ordered watch men to guard houses to make sure that the sick and their families stayed shut up. House owners were ordered to sweep the streets outside their homes. Taverns and theatres were closed to stop plague from spreading. William Harvey Medicine Before Harvey • Galen had said: 1) New blood was constantly being manufactured in the liver to replace blood burned up in the body just like wood is burnt by a fire. 2) Blood passed from one side of the heart to the other through invisible holes in the spectrum. This had been challenged by Ibn-Al-Nafis and Vesalius but neither could provide any alternative explanation. • Two other doctors had made discoveries that paved the way for Harvey: Realdo Colombo (1516-1559) said that blood moved along veins and arteries. Fabricus (1533-1619), Harvey’s tutor at Padua proved that there are valves in the veins. • Despite these pieces of knowledge, no body could explain how blood moved around the body. Fact File • • • • William Harvey (1578- 1657) He studied medicine at Cambridge and Padua then worked as a doctor in London. He published his book ‘An Anatomical Account of The Motion of The Heart and Blood’ in 1628, which described how the blood circulates around the body. He became doctor to King Charles 1st. Factors Which Helped Him • • • • Tech- Mechanical water pumps in London may have given Harvey the idea that the heart is pumping blood. Attitudes- Harvey’s discoveries were the result of careful dissection, observation of detail and experiment. Individual genius- Harvey was exceptionally thorough in his work, spending many hours repeating experiments and going over every detail. Communication- Harvey had read the work of earlier doctors and was able to use it to build up his theory. Factors Which Hindered • He could not explain everything about the circulation of the blood. • He did not know how blood moves from the arteries to the veins. Short-term Impact • Harvey proved that Vesalius was right about the importance of dissection. He wrote ‘I prefer to learn and teach anatomy not from books but from dissections’. Long-term Impact • His discovery laid the ground work for future investigation of the blood and physiology) the workings of the body. • Many aspects of medicine depends on understanding the blood system. Surgery, for example, could not develop until after Harvey’s discoveries. Limitations • Still much more to discover about the blood- no blood transfusions until 1901 when blood groups were discovered. • His ideas were only gradually accepted – some doctors ignored them while others said he was wrong (because it went against Galen). It was nearly 50 years before his ideas were taught at the University Of Padua. • His discoveries did not make anyone better. Achievements • Proved that the heart acts as a pump- pumping blood around the body. • Went onto dissecting animals because their hearts beat more slowly and so he could see the movements of the muscles. • Dissecting human bodies to build up detailed knowledge of the heart. • He proved that the body had a one-way system for blood. He tried to pump liquid past the valves in the veins but he could not do so. Andreas Vesalius Medicine Before Vesalius • Doctors believed that Galen had given a fully correct description of anatomy. • Dissections were carried out to show that Galen was right (not to check or challenge him) even though Galen had said it was important to learn by dissection. • He used human bodies but sometimes used animal bodies because human bodies sometimes/often were not available. Fact File • • • Born in Belgium (1514-1564). His father was a doctor. Studied medicine in Paris and Padua and then became a professor of surgery in Padua. • Wrote ‘The Fabric of The Human Body’ (1543)- a detailed, and fully illustrated description of human anatomy. Factors Which Helped Him • Tech- made use of new inventions of printing. Supervised printing & engraving so that everything came out the sameif he hadn’t printed/published his work, he’d have had less impact because printing meant that he could distribute thousands of copies which were sent all around the world. • Individual genius- He was inventive and determined. He once stole a criminal’s body to dissect it. In Padua, he encouraged dissections and insisted on making sure every detail in his books was printed correctly. • Art- In Italy, many artists were already interested in dissection to improve their own work. Vesalius used these to illustrate his books. • Attitudes/ Enquiry- Vesalius respected Galen but believed it to be vital to ask questions and challenge traditional ideas by carrying out as many dissections as possible. Factors Which Hindered His Work • Many doctors refused to accept that Galen could be wrong. Some said that Vesalius’s work only showed that the body had changed since Galen’s time. Heavy criticism lead Vesalius to leave Padua and instead work for Emperor Charles 5th. Limitations • Nobody was healthier as a result of Vesalius's work. His work was only the start. Many more discoveries were needed before people would live longer, healthier, lives. Short-term Impact • Vesalius's insistence on enquiry began to change attitudes and encourage others to follow his example. • Doctors realised there was more to be learned- Galen had not discovered everything about anatomy nor had he got everything right. Long-term Impact • Improved medicine and health. • Accurate knowledge of anatomy was vital for the building up of medical knowledge and so paving the way to better treatment later on. How Do You Think The Changes In Science Would Affect Medicine? The changes in science affected medicine a lot. For example, the Royal Society explored new ideas and so the findings could be published t for then to be used in medicine. Furthermore, new methods in science were being used. Ideas were looked into more deeply and more observations were made. They were likely to be more accurate and correct and so the medical science would have been more developed. In the end, the changes in science affected medicine a lot. There were short-term and long-term results which all affected medicine. Doctors and Training Improved technology, e.g. thermometers, microscopes, etc. Improved knowledge of anatomy and physiology through books such as those by Vesalius and Harvey. Growing acceptance that physicians should do the dissections of the human body for themselves. Introductions of some medical schools and teaching hospitals. Growing importance of a scientific approach – observation of symptoms and experiment with treatments. Improved Training More physicians travelled to universities in Europe or Edinburgh for medical training. Training took a more practical role, observing and examining patients, rather than just reading books. Students began to take part in dissections themselves. Some even began to set up their own medical schools. John Hunter S Trained in the new Renaissance methodology and his later carrer shows the impact of these ideas on medicine and training. His lectures on anatomy helped to develop a more professional approach to medical training. He emphasised the importance of observation and experiment. His students included Edward Jenner who followed his methods when investigating cowpox. Employed a secretary to write up his notes and paid an artist to draw the discoveries that he had made by dissection. Published several important works, including one about the changes that occurred in pregnancy. John and his elder brother William, set up their own medical school in London where Physicians received intense training. Intensely curious man and a workaholic. Studied many aspects of anatomy, using specimens to show the medical problems like arthritis and stages of a disease. Carries out various experiments as part of a study on the sexually transmitted infections. How did London get Clean Water? In the 13h century, lead pipes were laid to bring water from the river Tyburn to London, and people would go to the pool of water at the end of the channel to collect water. There were also water sellers who came through the streets, but the water was usually taken from a polluted river so most people drank ale rather than water. Although London’s council recognised the need for clean water, it could not decide what to do about it because it knew people would oppose any increases in their local taxes. Luckily two men were prepared to use their own money to improve the situation. 1602 Edmund Colthurst suggested constructing artificial river to bring water to London over a 38 miles journey. The project relied on gravity to get the water to London, route had to be carefully planned to ensure the channels always led downwards and the water kept flowing. Colthurst only managed to complete 2 miles due to money problems. Sir Hugh Myddleton revived the idea in 1609 and offered to pay himself. There were many protests from landowners along the route. Myddleton had King James I support and James even paid the costs. Project was finished in 1613. The project’s completion meant that fresh water was available in parts of north-east London, but the supply could not keep up with the growing population. By 1750 most water was supplied by private companies, either piped to the house or available at standpipes on street corners, which were turned on at certain times. Sanitation: chamber pots and water closets There was little recognition to improve sanitation. This created health risks, especially when sewage polluted the water. In medieval towns, toilets were usually wooden seats above a cesspit, and people wiped themselves with leaves or moss. Several families might share 1 cesspit and ashes might be scattered over the sewage to keep out the smell – but they needed to be cleaned regularly. These toilets were called earth closets. In the house most people used chamber pots, that were emptied into the drain in the middle of the street or sometimes the contents were just thrown into the streets from an upstairs window. It wasn’t much better for the rich. The king had a ‘close stool’, which was a padded seat over a large bucket, and the most important job within Henry VIII’s private rooms was the Groom of the Stool – the man in charge of his chamber pot and he had to S wipe his bottom. Sir John Harrington invented a water closet in 1596, using water to flush away the sewage, Queen Elizabeth I liked the idea so much that she had a WC installed at Richmond Palace but many people ridiculed the idea and the WC did not develop proplerly until 200 years later. The Great Plague 1665 The plague killed about a quarter of its population in London. This was the bubonic plague. However, this time there were major differences in how the outbreak was dealt with. In 1348, people tried to prevent the plague from spreading; in 1665, there was a lot of pressure on the town authorities to take on this role. Laws were passed to try and contain the disease. Many of them were ineffective and many people including King Charles II, left the city. Even isolation and quarantine did not work because the disease was not spread by human contact but was carried by the fleas on the rats. Until Pasteur’s work led to a better understanding of disease in the 19th century, neither doctors nor governments could deal effectively with infectious diseases such as the plague. The problem of gin The government were important because they had the power to pass laws to bring about changes. There was a public concern in the 18th century that cheap gin was having a bad effect on the poor. In 1750 the government passed laws that made gin more expensive. This was partly to try and improve the standard of health among the poor but also because the government was concerned about losing money if people were too drunk to work. The increase in price also helped to reduce the death rate from excessive drinking. S Did Hospitals And Treatment Change During The Renaissance? Hospitals (Middle Ages) • Hospitals were run by monks and nuns. They provided warmth, food and prayer for the poor. • There were hundreds of small hospitals but they did not admit people with infectious diseases in case the disease spread among residents. • 1660s- St Bartholomew's had 12 wards and 300 beds Hospitals (Renaissance) • • • • • • • • • • Many hospitals were closed because Henry VIII closed the monasteries. Some were taken over by town councils. Most of them were then used to look after the elderly. 1700s- Many new hospitals were opened. They were paid for by local people + charities + town councils. Nearly all of them still cared for the poor. If you were wealthy, you could pay for home care. Many hospitals still did not admit those with infectious diseases. However, this was beginning to change in some hospitals. Doctors trained in universities and carried on their training in hospitals to practice on the poor. There were nurse helpers- carried out heavy, manual work: washing, cleaning, food prep. They didn’t have any medical training. 46 hospitals in Britain in the 1700s. Treatments (Middle Ages) • • • • • • Remedies were made up of herbs, minerals and animal parts. Treatments included prayers, charms and rhymes. Bleeding, purging and other methods to restore the balance of the four humours- this followed the methods of Galen. Treatments included rest, exercise and a good diet. Many home remedies were used, especially herbal. Girls learned how to mix them up- honey and orange juice were often used. • Home remedies were handed down through generations •Bleeding was also used to prevent illness- all to do with the four humours being out of balance. • Rhubarb was used to purge the bowels. Treatments (Renaissance) • Patients were kept clean and warm and were fed regularly. • The sick were given herbal remedies or they were bled. • Simple surgery was done- e.g. to set fractured limbs. • Some desperate surgery too- amputation as a last resort. • All treatments were free but people were still expected to pray for their recovery. Judgement • From the Middle Ages to the Renaissance, there was little, but some change, in treatments and hospitals. This is because it seems small details were changed. For example, in the Middle Ages, monks and nuns ran hospitals providing warmth, food and prayer where as in the Renaissance, doctors, along with nurses, ran them instead and provided cleanliness, warmth and food. Although there was change, there wasn’t any dramatic changes but just a slight transition. Why Did The Discoveries Of The Renaissance Period Have So Little Impact On Medical Treatments In Britain Between 1500 and 1750? Structure Tip Answer Plan/Grid Factor Evidence Explanation Link Attitudes No-one challenged Galen; they did not accept other ideas. The Church still had authority. It was frowned upon to challenge. Galen was wrong. Doctors with treatments based on his idea. Noone challenged it and so nothing changed. Conservative attitudes of people at the time Many treatments, such as bleeding, continued to be based on the idea of balancing the four humours. Most people continued to follow Galen’s ideas. The Christian Church supported Galen’s ideas and so they should not question. The Church controlled universities and medical training. Doctors discouraged research and developing new ideas concerning treatment. People didn’t want to challenge Galen. People continued to use Galen based treatment. Beliefs Most people continued to believe Middle Ages causes for illness- e.g. four humours and evil spirits. Harvey’s discovery hadn’t discovered an actual treatment. No treatments were newly discovered and so medicine continued to follow Middle Ages ideas. Government People continued to support Galen because the Church frowned upon opposition. Church still had authority. It supported Galen and so told people what to believe. No body opposed and so no-one tried to make any other medical developments. There were not advances. • Factor • Evidence + Explanation • Link to the question Answer Example • Attitudes- People were very supportive of Galen’s work. They did not think he could be wrong and so weren’t ready to accept other ideas. • Explanation- The church were also supportive of Galen’s ideas; it was frowned upon to accept other work/doubt Galen’s. For example, Roger Bacon was put into prison for challenging Galen’s ideas/work. • Link- this meant that doctors did not develop their own work/treatments but continued to base their work on Galen’s ideas which were wrong. No-one challenged this. Ancient World Ideas about the causes of disease Middle Ages Renaissance/ Scientific Revolution Gods & Spirits Four Humours Bad air Planets + Stars Treatments New herbs from over seas Herbal Remedies Prayers Bleeding + Purging Rest + Exercise Methods of avoiding illness Charms + Prayers Exercise + Diet Bleeding + Purging Training and hospitals Uni training of physicians Knowledge passed through generations Hand written books Printed books Hospitals run by monks + nuns Individuals Hippocrates Galen Arab docs- Ibn Sina Al-Razi Building of hospitals Fewer hospitals Versalius Harvey Industrial Revolution 1750-1900 Who Was Edward Jenner & Why Was He Significant? Fact file • • Age 13- Had an apprenticeship with a surgeon for 6 years. Age 21- Studied with John Hunter in London. He was the greatest surgeon of all time. He taught students to observe carefully and make their own experiments to increase medical knowledge instead of relying on books. • Age 23 (1772)- Began work in Berkeley, Gloucestershire, as a country doctor but kept in touch with John Hunter about medical developments. • 1798- Published his book, An Enquiry Into The Causes and Effects of Variola Vaccine (known by the name of cow pox). This showed that vaccination could save people from smallpox. • HE CREATED THE VACCINATION FOR SMALLPOX. Background • Smallpox killed more children than any of her disease in the 1700s- survivors were often left disfigured by scars and scabs formed. • Lady Montague watched inoculation in Turkey- spreading puss from smallpox into the cut of a healthy person. If they were lucky, they got a bit but then never again. During the smallpox epidemic in England, she had her daughter inoculated in front of important doctors- the method then became popular. • Inoculation became a big business. People became wealthy through carrying out thousands of inoculations. • However, there were problems with inoculation; inoculated people could die from too big of a dose + the inoculated people could spread/pass on small pox to someone else + most people couldn’t even afford to be inoculated and so could not be protected. What Happened? • Some doctors realised that milk maids who caught cow pox didn’t get small pox. • Some doctors got the disease on purpose and spread it but hadn’t made the method widely known or even properly, scientifically tested it. • Jenner knew the theory; he kept thinking about it and thinking about how to test it and prove it. • In 1790s, he carried out experiments observing and recording all the details. • 1798: He published his book which described vaccination + presenting evidence- describing 23 different cases to prove the theory. • He called his method ‘vaccination’ which came from the Latin ‘Vacca’ which means cow. • Edward Jenner’s discovery saved thousands of people’s lives in Britain and millions worldwide. Factors • Attitudes & Enquiry- Jenner, following Hunter’s advice, tested the connection between cowpox and smallpox in experiments collecting evidence carefully as proof that catching cowpox realy did protect against smallpox. • Government- (1802 + 1807) Parliament gave Jenner £30,000 to develop his work on vaccination. 50 years on, in 1852, vaccination was made compulsory in Britain and this helped to cause the huge drop in the number of cases of smallpox cases. • Individuals- Jenner had the insight to realise that the link between cowpox and smallpox was important and had the determination to carry on and publish his research despite opposition and criticism. • Communications- 1798: Jenner published his own account of his discovery to spread the details of his method worldwide. Ideas about disease 1750-1900 During the Renaissance there had been a growing interest in science. This affected people’s ideas about the causes of disease, and by the 18th century they were less likely to blame disease on supernatural causes or umbalanced Humours. People had always been aware that disease spread quickly in dirty, smelly and unhygienic conditions, and so the search for a new explanation of illness based on natural causes now developed into 2 main theories. • Miasma –disease was caused by bad air that was filled with poisonous fumes from rotting matter. • Spontaneous generation – disease was caused by germs that were produced by flesh and vegetables as they rotted. During the Industrial Revolution, in the late 18th and early 19th centuries, the population grew rapidly. Housing for workers was of poor quality and many families could only afford to live in a single room. In these conditions, disease spread rapidly, especially as there was poor sanitation and limited access to water. Killer Diseases Disease How it spread Effects Cholera Bacteria passed on through food and water that have been contaminated by the excreta of another person. Sickness and severe diarrhoea; dies from dehydration, often within 24 hours. Up to two-thirds of sufferers died. Diphtheria Through tiny droplets when coughing and sneezing or through contact with the soiled clothing of an infected person. Bleeding, sometimes paralysis; suffocation from a blocked throat often leads to death. Death rate 1 in 10 but particularly hit children and took a long time to recover. S Smallpox By touch, or tiny droplets when coughing or sneezing. A rash turns into blisters filled with pus; the blisters become crusted and fall off, leaving deep scars. About a third of sufferers died. TB Tuberculosis Tiny droplets when coughing and sneezing. Coughing heavily, brings up blood, chest pains severe, weight loss. Nearly half died. Typhoid Bacteria passed on through food and water that is contaminated by the excreta of a person or food infected by Headaches, fever, constipation, severe diarrhoea. One-third of sufferers dies. Affected the old, weak and Stepping Stones Why Was Their Opposition? • • It went against God’s law to give people an animal disease. • Smallpox was seen as a punishment for sin- the only cure was prayer and living a Godly life. • It would cost the inoculators their jobs and profits. • Royal Society- said that the ideas was too revolutionary. They refused to publish Jenner’s book. • Vaccinations were viewed as clumsy- they were done in a rush and didn’t always work. • People had enough to worry about, like finding work and food. They didn’t have time to have their kids vaccinated. • The Government shouldn’t interfere . They had no right to force people who didn’t get their children vaccinated. Vaccination is a good example of experiment and enquiry. It showed that the killer disease could be beaten. This encouraged other doctors and scientists to solve medical problems. • Vaccination was widely used in Britain. It was made compulsory in 1852 which lead to a significant reduction in the number of deaths from smallpox. Factors like public health reforms also played a part in this. • Vaccination was soon used globally. By 1803, it was being used in USA and in 1805, Napoleon had all of the French army vaccinated. Ironically, it was fighting a war against Britain. In 1812, Jenner’s work was translated into Arabic and Turkish. • In 1980, World Health Organisation declared that smallpox had been eradicated from the world. But • Vaccination only dealt with one disease. There were many more infectious diseases (Cholera, Typhoid etc. killed thousands in epidemics). • Pasteur didn’t publish his Germ Theory until 1859 and so Edward Jenner did not know that bacteria caused disease and so he could not figure out exactly how his vaccination worked. Therefore, it was not possible to learn from this discovery about how to prevent the spread of other diseases. • Many people opposed vaccination. An ‘Anti-vaccine League’ was formed in 1896. • The Government could not decide whether they wished to force people to vaccinate their children. The law kept changing. Why Did The Discovery Of A Vaccination For Smallpox in 1796 Not Lead To More Preventative Treatments? (12) • • • Didn’t know about germs People opposed him Government were unsure about whether to back it Answer Firstly, one of the reasons is that Pasteur’s book about his Germ Theory was not published until 1859. Already, Jenner did not understand exactly why his vaccination worked and so, because he couldn’t learn from Pasteur’s theory yet, Jenner could not use his little understanding and knowledge about his vaccination in order to develop it to help prevent other infectious diseases. Secondly, Jenner had a lot of opposition surrounding the vaccination. He wasn’t very well known; he was just a country doctor and many had created a bad image of him This meant that he did not receive support of his ideas and so was limited in the help he could use to develop his ideas. This also meant that people were reluctant to be vaccinated which meant Jenner couldn’t research and investigate as much as he could have done with volunteers. Furthermore, the Government kept changing the laws on whether to back Jenner, and make vaccinations compulsory, or not. Lack of Government backing would have also affected the public’s trust of Jenner as well as giving Jenner little support (like facilities and funding etc.) which all meant that Jenner’s ability to develop vaccination was limited. In 1896, the Anti-Vaccine League was set up which opposed the compulsory vaccine, particularly against smallpox. The organisation influenced a huge proportion of people in Britain and so left Jenner with little backing and few to actually use the vaccine on. As a result, he could not develop the vaccination enough to gain knowledge and develop other preventative treatments. What Was The ‘Germ Theory’? Before 1750 • God caused disease to punish people for their sins • Bad air (like bad smells) caused miasma • Theory Of The Four Humours Spontaneous Generation • This was the latest theory. • It was developed when microscopes picked up bacteria on decaying matter. Scientists thought that germs were spontaneously (automatically) generated (created) by the decay and then spread the disease further. Louis Pasteur • A French scientist (chemist) in the late 1850s. • He was asked by a brewery company to investigate why their alcohol was going sour. He thought it was because of germs and proved that germs in the air were causing the decay (not the other way around). • Investigation- He took two flasks- he heated a liquid in one of the flaks to kill the germs and make it sterile. He drove the air out of it so that no more bacteria could grow. He then sealed the flasks with some more liquid inside. Later on, approximately 100 years, the cleaned flask was still sterile- there were no germs in the flask. The other flask was full of bacteria. • This was the start of ‘pasteurisation’. The method of heating and sterilising liquids. • Many foods today are pasteurised- e.g. milk. The method also paved the way for air-tight food storage, vacuum packing, airtight jars, tins and cans etc. • He was then asked to investigate diseases in silkworms and proved that bacteria was spreading the disease and so linked germs to disease (in animals). • Then- proved that germs caused disease in other animals too… • He accidentally injected a chicken with some old chicken cholera germs- the chicken did not die. He then injected it with fresh germs and the chicken still didn’t die. He had proved Jenner’s vaccination worked. • He now wanted to prove that germs caused human diseases too. • There is a link between him and Jenner but were not exactly the same. • • He then wanted to prove germs caused human diseases too. There is a link between Louis Pasteur and Jenner but they aren’t exactly the same. Who Was Robert Koch? Fact File • Born in Germany (1843-1910) • He was a doctor who read Pasteur’s work • He was especially great at lab work; he had a team of assistants • There was a rivalry between Pasteur and Koch especially at the time of the Franco-Prussian War (1870-71) What He Did • • • • • Koch set out to find the specific microbe/bacteria causing individual diseases- Jenner didn’t know how to develop his vaccination to do this; he didn’t know about specific germs etc. Koch was the first to identify specific microbe that caused an individual disease. Koch did this for TB (1882) and Cholera (1883). Koch discovered how to stain and grow bacteria in a Petri dish. This meant that by staining each bacteria, he could identify what bacteria caused a disease. He went about doing all of this using a method that other scientists could easily copy and follow. Also At The Time • • Also, at the time, a number of other disease causing bacteria were identified: 1882- Typhoid 1886- Pneumonia 1887- Meningitis 1894- Plague Koch was important because he was able to identify specific bacteria which caused those horrible epidemics. Why Was Robert Koch Important?- Plan • Koch used methods that were easy to follow and copy. This meant that other scientists could do their own investigation and so knowledge of the field would expand. It also meant that these laboratory techniques can still be used today. • Koch identified bacteria for different diseases. This proved how Jenner’s method of vaccination worked and so it could all be put together to then form vaccinations for other diseases. • He was the first to stain bacteria. This was a very innovative method and was vital in identifying bacteria. He was inventive and was the first to use many methods that would go on to be used for years to come. The importance of research teams Pasteur and Koch’s breakthroughs are good examples of how important research teams were (and are) for scientific research. Pasteur and Koch were both hugely important individuals but they led, and were part of, large teams of researchers who received government funding – they did not work individually. By the end of the 19th century, scientific research was usually carried out by a team rather than an individual. A team was more likely to have funding and be able to afford expensive new technology, such as more powerful microscopes. Also, working in a team made it easier to check each other’s work and carry out large-scale testing. Furthermore, different members of a team could offer knowledge of different specialisms, for example, medicine, biology and chemistry. Who Was More Important? Pasteur Or Koch? (12) Pasteur Koch • Pasteur disproved ‘Spontaneous Generation’. • Pasteur proved that germs caused decay and not the other way around • Without his work, Koch could not have started his own work. • Pasteur invented ‘Pasteurisation’. • Pasteur proved that/ how Jenner’s vaccination worked. • Pasteur paved the way for air-tight food storage, vacuum packing, air-tight jars, cans and tins. Made food safer and so less people got ill. • Koch read Pasteur’s work. • Pasteur found the vaccination for ‘Anthrax’- an animal disease. • Thought of the ‘Germ Theory’. • Koch paved the way for other scientists to develop further ideas; he made it easy for them. • Koch discovered germs for specific diseases- e.g. TB and Anthrax. • Koch started to stain bacteria in order to identify them. • Koch worked with a team. This meant that more ideas could be thought up and there were developments were made more quickly. • Koch realised that if he could stain bacteria, he could kill them. • In conclusion, I think that Pasteur was the most important because his discoveries paved the way for Koch. Pasteur’s ideas, especially the Germ Theory and how it worked, it would have taken Koch a lot longer to do what he did. Pasteur’s Pasteurisation made food a lot safer to eat and this saved many lives. Explain Why Pasteur’s Germ Theory Was Important In Improving Our Understanding Of The Cause Of Disease (9) Tips • Don’t talk about the treatment • Stick to the 1860s Point Explanation/ Evidence Link to question Pasteur proved that bacteria was spreading disease- not the other way around Flasks- the sterile flask did not get germs in it- it stayed clean. Disproved ‘Spontaneous Generation’ Was able to focus on the correct science. His work progressed as he went on Alcohol- SilkwormChicken This meant that constantly he was gaining in knowledge in different areas and could then apply it to humans which was a bigger understanding. Robert Koch read Pasteur’s work (The Germ Theory). Robert Koch was able to continue work to gain a wider understanding Robert Koch identified specific disease- Huge development/ new understanding. Answer • Firstly, Pasteur proved that bacteria was spreading disease and that germs caused decay as part of his Germ Theory, not the other way around (Spontaneous Generation). His important experiment to prove this was his flask experiment. This involved heating two flasks containing a liquid (to sterilise them) and found that that the flask that had a straight neck contained bacteria when he later checked it where as the flask with an ‘S’ shaped neck was still clean. He concluded that bacteria from the air got trapped in the neck and so couldn’t reach the flask. This proved that bacteria/germs came from the air and was the cause of disease- he know knew the correct theory and could disregard incorrect ideas. • Secondly, Pasteur’s work progressed a lot throughout time. He started off investigating why beer was going sour then the diseases in silkworms and continued on to investigating the causes of disease in humans. All his work in developing ideas about disease gave him a wider understanding about disease because he made it relevant to various things and he was then able to apply his discoveries to humans • Finally, Pasteur’s Germ Theory was vital for the work of Robert Koch who read Pasteur’s work. This meant that Robert Koch could use the findings to start his own work concerning disease. As a result, he was able to go on to identifying specific bacteria which caused specific diseases. This also paved the way for other scientists to study exactly how bacteria worked and caused disease which meant even more developments could be made. Who Was Florence Nightingale? Fact File • 1820- Born in Florence. • Florence and her sister were educated by a governess and then by her father. • She enjoyed her education, especially reading and speaking Latin. She loved maths and even taught younger children. • She was strong and outspoken. She firmly believed in God. She believed that she was chosen by God for a special purpose but just did not know what that was. • 1840s- She had an interest in social conditions of people and wished to work in hospitals. • Her family were against her wish to become a nurse- it was not a suitable job for a well educated woman- at that time, they were coarse, ignorant and often drunk. • When she got home from a tour of Europe with friends, she studied in different hospitals. Against the wishes of her family, she started training to be a nurse- she trained in Alexandria, Egypt then in London (1853). She took an unpaid role as a ‘Superintendent’ at the ‘Establishment for Gentle Women During Illness’. • March 1854- Worked in Britain, France, Turkey during the war on Russia during the Crimean War (which started in 1854). • A Times News article reported bad medical facilities. Shortly after, Florence got a letter from a friend who invited her to become the Superintendent of the Female Nursing Establishment of the English General Hospital in Turkey. • The main aim was to introduce nurses into military hospitals. In November 1854, she got to Scutari hospital with 38 nurses. • Because she was female, she constantly had to fight military authorities every step of the way in a quest to reform military hospitals. • Conditions in the hospitals were poor. Injured men had to lie on the floor which was extremely dirty and full of vermin. Operations were performed in unhygienic conditions- unsurprisingly, more men died from Typhus and Cholera than injuries. • • • • • • • • • • She used her maths skills to collect data and recorded statistics and made calculations. Her results showed that the mortality rate of patients would improve if sanitation improved. By February 6th 1855, mortality rate decreased from 60% to 42%. She established a fresh water supply and bought fresh fruit and vegetables for men with her own money. By Spring 1855, the mortality rate had dropped to 2.2%. Deaths in British field hospitals hit its peak in January 1955, with 3,168 deaths. Considering the man power they had for that month and the mortality rate, if this had continued and troops had not been replaced frequently enough, diseases alone would have killed the entire British army in Crimea. When she returned to England- after the end of the war- she discovered that the mortality rate for soldiers in military hospitals during peace time was double that of civilians. Using her statistics, she pressed a need for reform in all military hospitals. May 1857, a Royal Commission on the Health of the Army was set in to investigate military hospitals. While in the Crimea, people donated money to Florence in a quest to improve the hospitals. 1860- she used the money to establish the ‘Nightingale Training School and Home for Nurses’ based at St Thomas’s hospital in London. She opened with 10 students and this group was the 1 st of many who’d benefit from the principles of 1) nurses should have practical training in hospitals organised for specific purposes 2) Nurses should live in a home fit to form a moral life with discipline. This made nursing a suitable career for respectable women. Florence acted as the Government Advisor on army medical care in Canada and also advised the US Government on army medical care during the Civil War (1861-1865). For much of her later life, from illness she had contracted from the Crimea, she was bedridden but she continued to work to improve the standards of hygiene in hospitals but publishing over 200 books and pamphlets- ‘Notes on Nursing (1860) was the first text book written specifically for the training of nurses and was published in various languages. • 1883- Florence was awarded the ‘Royal Red Cross’ for her work and, in 1907, became the first woman to be awarded the ‘Order Of Merit’. Did Florence Nightingale Revolutionise Nursing & Hospitals Single-Handed? Other Factors Which Improved Hospitals • Better engineering (Industrial Revolution) • Government laws to improve public health- 1848 and 1875 • More complex surgery- better trained nurses • Germ Theory- Had impact on all medical areas. Including surgery and so changed the way nurses carried out their work. What Had Changed In Nursing & Hospitals By 1920? • 1850- 1920 • Hospitals etc.- got bigger and so the number of patients being admitted increased. • Hygiene improved- and so did surgery and dressings • Nurses started to be trained • Wards got bigger- ventilation • Bad sanitation- now good sanitation • Sewage- now toilets • Lack of cleanliness- now cleanliness • Nurses now wore proper uniforms. Government action and other factors in development of Government Action hospital care Starting in London in 1867 but spreading throughout the country, it was ordered that Poor Law Unions should join together to build infirmaries that were separate from the workhouses and that had a fulltime doctor appointed to them. They were to be paid for by local rate-payers. New asylums for people with mental health issues and fever houses for people with infectious diseases were also built. These changes were an improvement but didn’t completely separate the workhouse and medical treatment for the poor: in 1887 the Birmingham Poor Law Union built a new infirmary with 1,100 beds, but 1,5000 old people were still housed in the workhouse 3 years later. However, by 1900 the Poor Law infirmaries and the fever hospitals and asylums run by local authorities death with far more patients than the voluntary hospitals, and these new infirmaries often went on to become major general hospitals with specialist doctors. S Reasons Why Hospitals & Nursing Changed 18501920 Florence Nightingale’s work in the Crimea Money raised for the Nightingale fund She set up training schools for nurses. These nurses showed their value, increasing respect for nurses and leading to women becoming nurses Florence Nightingale’s books influenced training and the design of hospitals The discovery that bacteria cause diseases Increased public awareness of the need for clean hospitals and qualified nurses Improvements in engineering and public health Developments in surgery, such as the use of anaesthetics and antiseptics- wider range of surgery Better hospitals and qualified nurses. Essentially- Nightingale + Germ Theory + Government + Other Factors = Cleaner facilities + better nurses (trained , more professional/respectable, not drunk) How Did The Training Of Doctors Change in the 19th Century? 1860 (Dr Smith, male) 1930 (Dr Jones, male) 2009 (Dr Brown, female) Training • Training was decided by university tutors, teachers and private tuition. • Government played no role in regulating the education of doctors. • Training at uni consisted of reading books, lectures and practical training. They were also trained to observe, to think for themselves and were trained in scientific method. • Training was decided by university teachers + Royal Colleges could strike off failing doctors. • Government played no role in helping. • Training at uni consisted of reading books, lectures and practical training. They were trained in scientific method (like Dr Smith). • Training decided by university teachers and Royal Colleges. • Government now play a part in regulation. • Same as Dr Jones but now also read scientific journals. Understanding the cause of illness • Believed in ‘Spontaneous Generation’. • Knows infectious diseases caused by bacteria but many illnesses could not be explained- e.g. illnesses babies were born with. • Knows infectious diseases caused by bacteria but knows many illnesses have genetic causes stemming from the DNA of the person too. Equipment for the diagnosis of illness • Little equipment to help. • Had a thermometer and one of the NEW stethoscopes. • Had a thermometer and stethoscope. • Can carry out blood tests. • Can send patients to X-Ray but has no charge. • Has a thermometer and stethoscope. • Can carry out blood tests and may have an X-Ray at their office. • Can send people for X-Ray and scans and some GPs can carry out minor surgery. Ability to treat the less well-off • Held surgery for the poor in a local dispensary but there were still charges for medicine. • Does some charity work for the poor. • Still charges a small fee for the medicine. • NHS provides free healthcare. Treatments • Medicines made from herbs. • May have needed to bleed patients. • Recommended changes in diet and exercise. • Could offer vaccinations against some dangerous diseases and Sulphonamide drugs were introduced. • Common illnesses were treated with diet, exercise and rest. • Treatments for genetic diseases was developing. • Provided vaccinations and could remind parents to have their children vaccinated. • A wide range of antibiotic drugs for common illnesses. • Does prevention work and gives advice on diet, smoking, exercise and weight. Method of payment • Payments from patients. • Payments for visits. • Payments for medicines he mixed. • Payments for patients. • Payments for visits and medicines he mixed. • Employed a debt collector to collect payments. • 1/5 of patients could not afford to pay. • Paid by the Government directly through the NHS trust or GP partnership she works at. Public Health In The Early 1800s? • • • • • • Food- Fresh food was difficult to get in many towns because it had to be brought in by horse and cart and was expensive. Food was often adulterated- mixed with other things (chalk in bread, sand in sugar and sawdust in flour)- by shopkeepers to increase its weight and so make more money from sales. Working conditions- Working conditions were at least as bad as home conditions. Workers in mines, workshops and factories had long hours and very short breaks. Their toilet and washing machines were very poor, with many people sharing one privy and only a pipe to wash at. Many people also fell ill from the work itself, swallowing coal and textile dust, which caused lung disease. Patient fees- Doctors were not paid by the Government and so had to charge fees to their patients. Therefore, the poor could not afford to go to a doctor. Government- Governments were still not expected to play a major part in improving the living and working conditions of the people. There were no pensions or help for the sick and unemployed from governments. The first income tax was collected in 1798 and stayed low in the 1800s. Houses- Towns had grown very fast. Landlords made profits from renting out houses and so wanted them to be built quickly. Railways- Railways were not built to take people in and out of town centres in large numbers until the 1850s and later. Workers, therefore, had to live close to their places of work. How Important Was Edwin Chadwick? How important was the role of Edwin Chadwick in improving public health services in towns in the nineteenth century? (16) • Positive impact of Chadwick’s work • Limitations of Chadwick’s work • Weigh up Chadwick’s work against other factors and individuals. Plan Importance Of Chadwick • Report- Chadwick realised that the poor were living in bad conditions- this lead to illness- which meant that they couldn’t work- and so others had to pay higher taxes to help them. In his report, he came up with a solution= improve drainage and sewage + remove waste from the streets + introduce clean water supplies and appoint medical officers in each area. • He was hard working and so managed to gather lots of evidence. • His report’s recommendations were the basis for 1848 Public Health Act. His report influenced the Government and persuade people that reform was needed- in 1900, people were living longer- towns were cleaner. Limitations Of Chadwick • 1842 report- did not lead to immediate reform- the Public Health Act was only introduced in 848. • 1848 act did not force councils to reform public health- nothing was compulsory. • Personality- Antagonised/ annoyed/ irritated people and so he did not win much support for his cause. He was arrogant- when the Germ Theory was published, he refused to accept it; he still believed in miasma. • His influence faded in the 1850s. • He had quite a lot of opposition- For example, many local tax payers did not want to pay more for the improvements + the Government were not happy because local councils didn’t want the Government interfering. Other Individuals • William Farr- Used information from birth, deaths and marriage registers (after they were made compulsory in 1837) to build and accurate picture of where the death rate was particularly high and what the causes of death were. He proved the link between unhealthy living conditions. He shamed some towns into improving public health conditions. Evidence put pressure on local and national Government to make changes. • John Snow- He was a pioneer in surgery, public health, improving medical conditions and the use of evidence to challenge old theories. In 1849, he published a book says that Cholera was being spread through water- not ‘bad air’. His suggestions were mocked by many. In 1854, there was another outbreak and this gave Snow a chance to prove his theory that water was spreading Cholera (from using it for things like drinking and washing). Public Health Act 1848 In 1848, another serious outbreak of cholera finally prompted the government to take action on Chadwick’s ideas. The Public Health Act in 1848 set up a General Board of Health, with Chadwick as one of the 3 commissioners. It allowed towns to: • Set up their own local Board of Health • Appoint a local medical officer • Organise the removal of rubbish • Build a sewer system But it did not force councils to do this, unless the local death rate passed 23 per thousand living. Only one-third of towns set up a Board of Health and even fewer appointed a medical officer. Meanwhile, the terms of the Act were only temporary so that, in 1854, the 3 commissioners had to resign and the General Board of Health was abolished in 1858. Chadwick was not appointed to any other official position. Parliaments slowly became convinced during the 1850s and 1860s that they should take further action and that measures should be compulsory. • Snow’s work proved there was a link between water and cholera. • Pasteur’s germ theory showed disease spread and why hygiene was important. • Snow also showed the death rates varied according to water sources and the company. Another outbreak of Cholera in 1866 least affected those towns where there had already been some improvements. This reinforced the link between hygiene and health. Working class men when given the vote in 1867, were putting more pressure on the government to take action. Public health Act 1875 • 1866 Sanitary Act forced all towns to appoint inspectors to check water supplies and drainage. • 1875 Artisans Dwelling Act gave local authorities the power to buy and demolish slum housing. • These led to the 1875 Public Health Act – which made local councils responsible for ensuring that the following were provided: 1. Clean water 2. Public toilets 3. Rubbish removal 4. Sewers and drains • The act also made towns appoint Health and Sanitary Inspectors and a Medical Officer of Health. • In the years after 1875, local councils also became responsible for: 1. Checking the quality of food in shops 2. Ensuring that the quality of new housing was improved 3. Enforcing a new law againstSpolluting water supplies such as rivers and streams. • Despite this, in many towns, basic services such as water, lighting and paving were still in the hands of private companies and individuals. The Great Stink and Joseph Bazalgette Plans were already being made for a new sewer system in London in 1858. However, the extremely hot weather meant the level of the River Thames was low and the smell of the exposed sewage along its bank was so great that parliament could not meet, even though sheets soaked in disinfectant were hung at the windows to cover up the smell. The ‘Great Stink’ combined with outbreaks of cholera, and the work of people such as Chadwick and Snow, to convince the authorities that more public health reform was needed. Josephy Bazalgette The Metropolitan Board of Works agreed to the expensive ideas being put forward by Joseph Bazalgette for a new sewer system in London. He was an engineer who had worked on large-scale sewage and drainage projects. He designed a complex sewerage system for London that took into consideration future population growth as well as the needs of the time. It included 1,300 miles of sewrs, plus pumping stations and embankments besides the River Thames to house the stations. It took Bazalgette and his huge team of engineers and construction workers over 7 years to complete. Role of industry and technology There was a lot of planning and engineering that went into London’s new underground sewer system. Although the Industrial Revolution led to many public health problems, it also provided some of the solutions. Through designing and building machinery for farms and factories, and the development of the railway and canal systems, people had learned the best ways of building pipelines, tunnels and embankments and how to harness the power of steam to run engines. The pumping station was installed in 1865 London. The engine was one of four engines used to pump water through London's sewers. They worked tirelessly until they were replaced by a more modern system in the 1950s! Machines and systems such as this would have been impossible to achieve before the technological developments of the Industrial Revolution. S Life expectancy 20th century At the start of the 20th century, photographs, film, electricity, the bicycle and the motor car had all been invented but many people continued to live in cramped and unhygienic conditions, using oil lamps or gas lighting. Despite advances, many people would still not be able to afford a doctor and the average life expectancy was 47. Pasteur’s germ theory had led to a range of vaccinations being developed but there had been little progress in the search for a way to cure diseases and most medicines were still based on mixtures of ingredients such as plants and spices. The 20th century was a story of huge improvements in the treatment of illness. Most people in the UK now have better living standards than in the 19th century, and often better diets as a result of increased prosperity. Pasteur’s germ theory in 1861 was an important breakthrough in understanding how disease is spread. It led to Koch’s work in identifying the different microbes that cause disease. The technique to prevent people from catching a disease was developed and applied to more and more diseases. The government also began to intervene more in people’s lives. They first encouraged and then later insisted that all children were vaccinated. First and second magic bullet • Emil von Behring developed Koch’s work to isolate the antitoxins used by the body to fight diphtheria – then found a way to inject them and cure the disease. • Paul Ehrlich (a member of Koch’s team) now set up his own research team to build on this work. Ehlrich knew certain dyes stained specific microbes (Koch’s work) and antitoxins only attacked the disease microbes (Behring’s work) • Ehrlich tried to combine a dye with other chemicals to find a cure for syphilis – a ‘magic bullet’ that would only target the disease microbe and not harm the rest of the body. • Ehrlich researched for several years (this was only possible because he received German funds). • In 1909 Dr Sahachiro Hata joined the team from Japan and reviewed some previous experiments. He discovered a mistake – the 606th compound that they had tested and dismissed was actually effective! This treatment was called S Salvarsan 606. • Second Magic Bullet • The use of chemical drugs to target and cure illness was an important breakthrough. However, it was not until 1932 that a second magic bullet was found, when Gerhard Domagk discovered that a particular red dye was effective against some cases of blood poisoning and he developed the drug Prontosil. Many people died after simple cuts or scratches became infected, so this cure for blood poisoning could save many lives. • Research showed the key ingredient in Prontosil (sulphonamide) which led to other developments in drugs that could cure pneumonia, scarlet fever and meningitis. Discoveries were important because medicine could now cure many of the infections and diseases that had in the past, led to death. At first, treatment was injections, then late 19 th century it was mass produced pills. Antibiotics • Alexander Flemming was a chemist working at St Mary’s hospital in London. In 1928 he noticed that bacteria growing in a Petri dish was being attacked and killed by an unknown mould growing in the same dish. • This ruined his experiment but he decided to research the mystery killer mould before throwing it away. He discovered that it was an excellent antibiotic, penicillin. • Flemming published his findings in 1929 but he was unable to get funding to develop his work. • It was difficult to produce pure penicillin and so it did not seem practical to try and use it in medicine. However, Howard Florey and Ernst Chain, 2 scientists working in Oxford , read about Flemming’s research and in 1939 they set up a research team to develop penicillin. • In 1940 they tested it on mice, and in 1941 they conducted tests on a patient. The test showed that penicillin wads like a miracle drug on people who were dying from infection. Unfortunately there was only a small amount of penicillin available and the patient died when the penicillin ran out. • Florey was determined to develop the mass production of penicillin. The mould had to grow. This meant that they had to use a collection of containers, including baths, bedpans, milk churns and food tins, and had to hire 6 assistants just to deal with this stage of the work. No British firm was able to create the technology needed to mass produce penicillin – partly because many factories were being damaged by the bombing raids during WW2 or were already working to full capacity producing other drugs needed during the war. • In June 1941 Florey and Norman Heatley (another member of the team) went to the USA to see if pharmaceutical companies there would fund their research. • At first they were unsuccessful but in December 1941 the USA entered WW2 and the US government was now prepared to fund the mass production of penicllin. • They knew that in war many soldiers were likely to die from infection rather than from actual injuries and so mass-produced penicillin could save many lives. This injection of money allowed the pharmaceutical companies to invest in large-scale. • Florey had discovered that dying the mould at low temperatures was the most successful method of purifying penicillin. Scientists at the chemical company Pfizer, in New York, used an old ice-cream freezer to develop a method of freeze-drying that was eventually used for large scale production in 1944. S What Problems Remained In The 1930s? • Unemployment was still high- over 3 million. All the unemployed were outside the National Insurance Scheme. • Those in work could not afford to pay and so they could not get free medical help. The system of 1911 was failing. The death rate of under 1 year olds was high. The Setting Up Of The NHS • There was great opposition- Doctors were worried about losing money. • Minister of Health (Aneurin ‘Nye’ Bevan) agreed that doctors could treat patients privately as well as working for the NHS as a result. Reason For Opposition The Beverige Report What Did It Suggest? • Setting up the NHS- free for all, paid from taxes, staff were Government employees and so they were paid through them. This would mean that they didn’t need to charge patients to produce a wage. • All people in work would pay National Insurance out of their wages (This would pay benefits- sick pay, pension, unemployment pay) to all whether working or not (ill). • ‘Cradle to grave plan’. General • • His report was greeted with enthusiasm. Sir William Beverige was a civil servant who was asked to write a report on what should be done to improve lives. He had previously played a part in organising 1911 National Insurance Scheme- he helped set it up at the time. This meant that he had lots of experience of problems and solutions. WW2 Change In Attitudes • Evacuation- Middle-class were left shocked at children’s condition: dirty, unhealthy and under-nourished. • After all the suffering in the war, people wanted a better future and better health care was part of this. • During the war, many did not get free care to keep them fit in the war effort. • • Losing money & freedom (doctors) Some thought that the sick only got sick through laziness and so did not think that the poor should be helped. • Charities and councils ran hospitals and so did not want to hand them over to the Government. • Some thought that people would grow lazy because they’d be getting ‘something for nothing’ and so it would make people less likely to bother working. The Role Of Bevan • • • • Speaker Idealist Working-class background Won doctors over The End Result • Effectiveness- Yes, life expectancy increased from the year 1919 to 1992. • The NHS offered many services: midwifery, after-care, dentists, hospitals, medical research, teaching hospitals, vaccination and ambulances. Why Was The Discovery Of DNA Important? What To Think About: • • The causes of how DNA structure was important. The significance of why these discoveries are so important. To Begin With: • 1800: scientists knew that DNA existed and somehow controlled what we are like but did not know how though. Discovery • • A series of discoveries over a long time. First step- 1953, two scientists in Cambridge (Francis Crick and James Watson) discovered the structure of DNA. • They proved that DNA is in every human cell- this showed how DNA passes on information from parents to children. • Their discovery was the launch pad for other discoveries. Mapping The Human Genome • • • • • • 1986: The Human Genome Project was set up in order to identify the exact purpose of each of the genes in the human body- they compiled a map of human DNA. The task was completed in 2001- 15 years after the project had begun. The project involved teamed from 18 different countries such as USA, UK, France and Japan etc. Each team studied a different part of DNA. It required computers- TECHNOLOGY WAS IMPORTANT!! The information found through the project filled 80,000 text books but was passed worldwide instantly via internet. Crick & Watson • Were very adventurous in their ideas. They tried out methods which other scientists did not try. • They did not work alone; they worked with a team with a wide range of skills and knowledge: Maurice Williams (expert in X-ray photography and Rosalind Franklin who developed techniques to photograph a single strand of DNA an was the first person to take X-ray photos of DNA). • They had the latest and best equipment. New technologiessuch as X-ray photography and improved microscopes and built on new knowledge in other sciences (like genetics and biochemistry). • Their research was very expensive because of the complex equipment and the number of highly skilled people involved. • Most of the money came from the Government while industries also made a contribution. Why Is DNA So Important? • DNA has lead to work on stem cell research. • E.g. Christopher Reeve (paralysis) campaigned for stem-cell research. • At this stage (now), we do not know a lot because we are just at the start of the DNA Revolution; it has not yet lead to any treatments. We do not know how much it will effect medicine in the future but there are various possibilities… Understanding DNA Could Lead To: • Gene therapy- Using genes from a healthy person to cure the sick. • Customised drugs- Creating drugs to cure one person’s particular heath problems. • Genetic engineering- Choosing the nature of a child- like genetically modifying plans- (e.g. gender, appearance and intelligence). • Genetic screening or testing- Identifying the illness people could suffer from and preventing it as a result. E.g. identifying if a person is more likely to get cancer or possible conditions in unborn babies. Positives Of The Discovery • Could lead to treatments and further medical discoveries. Limitations Of The Discovery • The discovery has not yet lead to any treatments. Double Heelix During the 20th century, scientists could take photographs of human cells through 2 improvements in tech. – electron microscopes and X-rays. It became known that each cell in the body contains DNA, which is a set of codes controlling the genes that decide eyes and hair colour, height etc. Francis Crick and James Watson worked together to investigate the structure of DNA. Crick was a physicist and Watson a chemist. Research into genetic conditions requires very specialised knowledge and expensive, high-tech equipment. DNA Table 1953 Crick and Watson discovered the structure of DNA. 1990 The Human Genome Project mapped the location of every single one of the 30,000-35,000 genes in the 23 chromosomes in every cell of the body. The project involved hundreds of scientists working in 18 teams. The first draft was produced in 2000. Scientists have identified certain genes that pass on specific hereditary conditions. The result? There are new techniques for skin grafts, better production of S insulin for diabetics and better vaccines. Better understanding of conditions such as Down’s Syndrome and leukaemia, and whether people are more likely to develop certain forms of cancer. There has been further research to develop techniques to alter faulty genes within the body and prevent genetic illnesses from developing. The discovery has been made that stem cells (found in the bone marrow and the pelvis) can transform into various types of cells used around the body – which offers a chance of replacing faulty cells with healthy ones. NHS & Public Health Since 1948 • • • • • Prevention of illness is not a major part of the NHS. 5th July 1948- First day of NHS Early 1960s- Old hospitals were replaced 1970s- Health care campaigns were introduced 1992- ‘Health of the nation’ initiative helped/s prevent and reduce death from cancer, heart disease, HIV and AIDS. • 1998- NHS Direct began (telephone line). What Was The Big Picture Of Public Health Changes After 1800? 1) Government had a laissez- faire attitude (that the Government should intervene as little as possible). 2) Governments encouraged councils to improve public health. 3) Governments forced councils to improve public health. 4) Governments passed laws to improve public health- mainly for the poor. 5) Governments passed laws in improving public health for everyone. Timeline 1831- Cholera killed thousands 1842- Chadwick Report was published 1848- Public Health Act was passed 1858- The Great Stink! 1875- Another Public Health Act 1901- Rowntree Report 1901- Boer War began 1907- Bring out your babies! 1911- Nations Insurance Act was passed 1920s- Home for Heroes! 1942- Allied victory at El-Alamein 1948- Free health care for all! Role of science and technology In the 20th century, scientific research and knowledge has led to: • Chemical treatment of disease (magic bullets) • Antibitoics, which used living organisms to fight disease. • More vaccines to prevent the spread of disease. • A better understanding of genetics: genetic changes that cause problems and genetic changes that can help/ • Treatemtns being developed for conditions, such as diabetes, which were previously incurable. Blood Transfusions Most attempts in the past had led to death. But in 1901 Karl Landsteiner discovered that there were 4 different blood groups, and transfusions were only successful if the donor’s and patient's blood groups were the same. This meant that: 1. People who might die from losing a lot of blood could now be kept alive. 2. People with blood disorders (such as anaemia) could receive treatment. The problem was that blood could not be stored (it clotted), so the donor and the patient had to be together, for the transfusion to be carried out. The high number of injuries during WW1 sped up the search for a solution. In 1915, it was discovered that adding sodium citrate prevented blood from clotting, but the blood cells soon deteriorated. In 1916, new scientific techniques made it possible to establish blood banks. X-ray machines – discovered by scientist Wilhelm Roentgen in 1895. Used to diagnose broken bones and some diseases. Used during WW1. Radiotherapy and chemotherapy – By 1902, scientists used Roentgen’s discovery to make another one – x-rays could be used to ‘burn’ and shrink tumours. This led to techniques called radiotherapy and chemotherapy which are used to treat types of cancer. X-ray crystallography – Developed in 1st half of the 20th century, allowed scientists to take powerful images of human cells. (This played a role in the discovery of the structure of DNA) Microscopes – Electron microscope invented in 1931. Used in medical research and in diagnosis. Scans – Not just X-rays but ultrasound and MRI, which are used to scan a patient and diagnose internal problems. Endoscope – Flexible tube containing a camera which can be passed inside the body so doctors can see what is happening without the need of surgery. Nuclear Medicine – radioactiveSelements can be injected into the bloodstream to help track ad diagnose what is happening inside the body. Pacemakers – These are used to help people’s hearts work properly. Dialysis machines – These keep people alive when their kidneys are not functioning properly. Dispensing instruments – Hypodermic needles and intravenous drips help to give a precise dose of medicine. Care of the sick c1900-1948 At the start of the 20th century, it was still women in the family who were mainly responsible for treating most illnesses and caring for the sick. Because doctors had to be paid for every visit, people would only use doctors if they were really ill., so most illnesses were treated with preparations bought from a chemist. Traditional ‘folk remedies’ continued to be used, such as red cloth to help you recover from a cold or influenza and a sweaty sock tied around the neck to help a sore throat. Minor surgery, such as taking out tonsils, was often done by a doctor on the kitchen table. A GP might also do some surgery in a local cottage hospital but anything serious would be referred to a specialist in a big hospital. Charitable Hospitals Many hospitals offered only basic care for the sick rather than the range of treatments we now expect, some were aimed at specific groups of people. Sanatoriums (medical facility) were built to provide a healthy diet, fresh air and hygienic conditions, which patients with TB needed to recover. Effective fundraising was important because many hospitals were set up through charity. In 1912, Queen Alexandra started a national Rose Day, volunteers sold them to make money for hospitals. The first day, the equivalent of £2 million was collected in today’s money. S Access to healthcare • Standard of living among the poor was still very low. Surveys showing how difficult it was for the poor to afford decent housing and food were carried out by Charles BOOTH AND Seebohm Rowntree. Their work showed that the main reasons for poverty were ill-health and unemployment. • The Liberal government that was elected in 1905 began to pass laws that they hoped would improve health among the poor. The 1911 National Insurance Act was particularly important. Every worker earning less that £160 a year was expected to join the scheme, in which contributions by the worker, employer and government were made to fund: • Free medical treatment and medicine • Sick pay for up to six months and support payment while unemployed for up to 15 weeks. • In 1919 the Ministry of Health was set up, which gave the government an overview of health care provision in the whole country. This was an important step in the government taking more responsibility for health, but actual provision continued to be a mixture of people paying for private care, local authorities providing some support and many hospitals relying on funding from charity. • An epidemic of influenza in 1918-1919 showed that there were not enough free hospital places. • Women and children were not covered by the National Insurance scheme and so they often delayed getting treatment because they could not afford to pay for a doctor. • Average life expectancy by 1931 had risen to 58 for males and 62 for females, and the government was doing much more to help improve the health of the nation. • Secondary school pupils received medical inspections • Free milk for poor primary schoolchildren was introduced in 1934 • Health clinics gave vaccinations and sold baby food cheaply. • Range of private health insurance schmes that could provide treatment for women, children and those men not covered by the government scheme. • A better understanding of disease, development in vaccinations and better treatment for disease meant that people were more willing to accept government interaction. • The death of 3,000 children from diphtheria in 1938 shocked the government and led to a vaccination programme offering free immunisation. The effects of WW2 • WW2 had a major effect on people’s awareness of the effects of poverty on health. People were shocked to find out that many children evacuated were not used to running water or proper toilets and that they often had nits, lice and skin infections. This was an important factor in creating the desire for a higher standard of health after the war and the setting up of the NHS. The war also had an effect on people’s diets. Food was rationed and fats and sugar were in short supply, S to eat more vegetables, so while people were encouraged their health was actually getting better than they had been. Education and prevention • The government now accepted that it had a role to play in educating and encouraging people to stay healthy. The government was starting to take more of a role in trying to prevent illness. • Developments in vaccinations, such as Jonas Salk’s polio vaccine in the mid-1950s, and the introduction of a vaccine in 2008 against cervical cancer • Government promotion of healthy diets • Better disposal of rubbish and treatment of sewage • Laws to reduce air and water pollution, for example the 1956 Clean Air Act, which health with the problem of smog (a mixture of fog and smoke from coal fires, industry and car fumes) • Laws to improve people’s working conditions, for example health and safety regulations about asbestos in the workplace. • Provision or environmental health officers to inspect restaurants, cafes and bars. • Strict laws on food safety in 1990 after outbreaks of salmonella, E. coli poisoning, and BSE in cattle. • Public health and private companies • Private companies are increasingly involved in public health. For example, the responsibility for the provision of water has now been passed to private companies but the fact that many of the pipes are over 100 years old and need repairs or to be replaced causes problems for the water companies, who are reluctant to carry out the repairs because of the cost. Government action – smoking, communication and private companies • Smoking proved very popular in the mid-20th century when cigarettes became very cheap. However, in the mid-1960s it became clear that there were links between smoking and cancer, heart disease and many other health issues. • In 1962 the Royal College of Physicians called a ban on tobacco advertising. • The government began taxing cigarettes heavily. • Since 1971 packets of cigarettes have carried a health warning. • In 2004 it was reported that over half a million admissions to hospital and 1 in 6 deaths were a result of smoking. S • In 2005 a ban was placed on most forms of tobacco advertising. • Smoking in public places was banned in 2006 in Scotland and in 2007 in England and Wales. Communication • Communication has played an important role in the government campaign, with messages on the products, posters and television campaigns to raise awareness of the effects. • When HIV/AIDS wsa recognised as a significant risk to health in the 1980s, the government funded a national information campaign. Pharmaceutical industry Cost of medicine and private health care The late 19th century saw the beginnings of this industry as companies such as Beecham and Boots began making and selling prepared mixtures and pills. Few of these first pills did any good (and some harmed) but as progress in science led to discoveries of first magic bullets and then antibiotics which successfully cured disease, pharmaceutical companies began to play an increasingly important role they: • Employed and financed scientists and researchers to find other cures and remedies. • Used and developed technology and industry to massproduce remedies. • Used advertising to make people aware of their products and buy them. Through financial backing and providing scientists with equipment needed, the industry has played an important role in finding new cures and treatments and making them available. However, the industry also created some problems. The industry expects to make a profit, therefore, many companies produce different versions of the same basic pill. Although each new drug is tested before it is licensed for sale, there can be problems during the tests or unforeseen sideeffects. For example, in the 1960s, a new drug called thalidomide was used to prevent morning sickness in pregnant women but it was found that it affected the growth of the unborn baby and the development of their arms and legs. Ethical Questions There is a lot of debate about whether scientists should ‘play God’ and use their knowledge of genetics to change people’s bodies. Some research depends on experiments with human embryos; others combine animal and human cells together; cloning has already been used on animals. Many people object to these things on religious and moral grounds or from fear of the side effects. The rising cost of the NHS soon became a problem for the government. This was because: • As people live longer, they are more likely to develop problems needing treatment. • Improvements in medicine mean people expect a greater range of treatment. • New drugs can help many conditions, but the cost can be very high. • Treatment is more complex and equipment more expensive, with new technology such as MRI scans. • Staff costs are high because of increased traning for doctors and nurses. Return to private healthcare? • Long waiting lists for treatment developed in the late S th 20 century, with rising demand for treatment from a growing, aging population, and many people’s conditions deteriorated before they could get specialist help. • As a result, private companies grew. • Many GPs and consultants now offer private health care. • GPs are encourage dot offer a wide range of care. However, because the way GPs are funded by the state it has meant that few of them now offer an emergency service. • In 2008, the NHS celebrated its 60th anniversary, but there is much discussion about whether it should continue in its current form or if there should be radical changes. Anaesthetics (use sheet) James Simpson • Simpson started his own experiments. He decided to use Ether as a base and mix it with other substances. He tried a mixture of Hydrochloric Acid and Ether (later to be called CHLOROFORM). At dinner one night he sniffed it in from of the family and immediately passed out. He passed his exams for the Royal College of Surgeons and in 1836 became a doctor at an Edinburgh hospital. In 1840 he became Professor of midwifery at Edinburgh. • He reorganised the teaching of the subjects, and made it an essential part of every medical student’s training. Over the years he became more and more concerned about the suffering endured by women during childbirth. • Simpson started his own experiments. He decided to use Ether as a base and mix it with other substances. He tried a mixture of Hydrochloric Acid and Ether (later to be called CHLOROFORM). At dinner one night he sniffed it in from of the family and immediately passed out. On November 4th 1847 he conducted an experiment to test the usefulness of chloroform. • Within fourteen days Simpson completed 50 successful operations using Chloroform. It was first given by a sponge soaked in the liquid pressed to the patient’s nose. Later special inhalers were developed. In 1852 Queen Victoria used it during the birth of Prince Leopold and it soon became completely accepted. Twenty years after it was first tired it was used throughout Europe and in 1866 Simpson was knighted. He died in 1870. Chloroform remained the chief method of anaesthesia well into the Twentieth Century. Not everyone welcomed the use of anaesthetics: • Victorians were very religious and some people felt interfering with pain interfering with God’s plan. • Some people didn’t trust the,. • Some doctors felt it was easier for patients to die if they had been made unconscious that if they remained awake and struggling. • Number of patients that died after their operations, increased when anaesthetics were used. • The effects of both chloroform and ether tended to remain in the body for some time. It was found that cocaine was effective for pain relief, but was addictive. Understanding infection When the patient was conscious surgeons would have to produce the operation quickly. Anaesthetics meant that they could take longer. This meant that they did more difficult operations. They did not understand germs so many people died after their operation from things like gangrene. Doctors used S to keep wounds clean for liquids such as wine and vinegar centuries but before Pasteur’s Germ Theory, no-one knew what was causing infection. That was why surgeons did things that seem obviously dangerous today. They reused bandages, spreading gangrene and skin infections from patient to patient. They did not wash their hands before an operation, nor did they sterilise their equipment, and some operated wearing pus stained clothes. Early attempts to control infection Ignaz Semmelweiss worked at Vienna general hospital He was concerned about women dying in childbirth and that more women were dying at home than in the hospital. He found that making the students wash their hands using a solution reduced the death rate. Many doctors made fun of his ideas and he was sacked. Joseph Lister and antiseptics Another man working to defeat infection was Joseph Lister. Lister was an outstanding surgeon who had researched infections thoroughly. He wanted to apply his scientific methods to solving the problem. Lister had seen carbolic spray used to treat sewage. He experimented and he found that a thin mist of carbolic acid sprayed over the wound during surgery could reduce infection. If the wound was then carefully bandaged in clean material, it would prevent infection setting in after an operation. In 1877, Lister moved to London to train surgeons under his own supervision. When, in 1878 Koch found the bacterium for Septicaemia (blood poisoning) which both Semmelweiss and Lister had tried to tackle, Lister’s work suddenly seemed even more important. People paid more attention to his methods. Other doctors and patients realised that the spray wasn’t useless but killed real germs and prevented common diseases. Lister didn’t stop there. By the late 1890s Lister had improved his technique. He was now able to remove all possible germs from the operating theatre, not just the wound. This lead to several measures to ensure cleanliness being introduced: Operating theatres and hospitals were cleaned thoroughly From 1887 all instruments were sterilised In 1894, sterilised rubber gloves were introduced for the first time Now that pain and infection had been limited in operations, more and more complex procedures could be attempted. The first operation to remove an appendix occurred in the 1880s and the first heart operation was carried out in 1896. However, even after Lister’s careful research, some people were still reluctant to use antiseptics. Firstly, the carbolic spray reduced the speed of operations. It also required extra work and expense and made everything smell, even cracking the surgeon’s skin. Moreover, when some surgeons tried to copy Lister’s work, they often got different results because they did not copy his routine exactly. Many doctors simply could not believe that it was possible for fewer patients to die, and were disbelieving and defensive. Finally, Lister failed to present his ideas well. When he gave talks, he seemed cold and aloof. Blood Loss Bleeding was another great problem. It was not possible to replace blood by transfusion although blood vessels could be tied with ligatures to stop the blood loss. The usual way to deal with wounds or amputations was to seal the blood vessels by placing a hot iron onto the wound or puring hot oil over it. In the 16th century a French surgeon (Amroise Pare) developed metal clips to place on arteries during an operation. He also tried to use silk thread to tie the blood vessels after an amputation instead of using heat to seal them. This was before Pasteur’s germ theory so there was no understanding of dirty hands inside a wound increasing the chance of infection. S Problems with Blood Transfusion Blundell was specialised in women and their care through pregnancy and giving birth. He found that a transfusion of human blood could sometimes stop the mother from dying: • Clotting – a scab forms, blood starts to clot. Blood clots the transfusion tubes. • Availability – clotting also meant that blood couldn’t be stored. They could only be done with a donor attached to the patient. • Immune response – transfusing blood from an animal into a human seemed to destroy human blood cells, often leading to death. Blood Types – 1901 Karl Lansteiner suggested there were different blood groups A,B and O. AB was then added. He identified some types were incompatible, could not be mixed. They had to be the same type. This breakthrough did not increase the number of transfusions because the donor still needed to be present to provide the blood whenever it was needed. This was not practical. • • • • • Blood Transfusions Blood transfusion was used effectively for the first time after blood types were discovered in 1900. Methods of storing blood and transporting it were improved. In 1915 an American doctor Richard Lewisohn found that adding sodium citrate stopped the blood from clotting. This meant that the donor did not have to be present. Richard Weil found that this could then be stored in refrigerated conditions. 1916 Francis Rous and James Turner found adding a citrate glucose allowed for it to be stored longer. Geoffrey Keynes, developed a portable machine that could store blood. First blood depot established in 1917. • After WW1 • Further improvements in blood transfusions. Including better ways to store blood and the introduction of donations of blood from civilians. • Bllod groups sometimes got confused: dif. Classification systems and mix-ups. • Bottles that blood was stored in not always free from bacteria. This could cause infection. • Type O worked for everyone but that meant hospitals only targeted type O people for donations. As giving blood also involved a big cut into the vein, it became difficult to find donors. • Doctors and surgeons were reluctant to change. Science and Technology Chemistry played an important part in developing anaesthetics and antiseptics. Surgeons were more willing to try complex operations, for example, removing tumours. They also began to deal with internal obstructions , such as hard ‘stones’ inside the gall bladder. In the 1880s operations to remove gallstones and the gall bladder became routine as a result of anaesthetics and antiseptics. Infection was controlled by using Lister’s carbolic spray, steralising the instruments, wearing rubber gloves and using sterilised catgut for ligatures. The discovery of X-rays in 1895 made surgeons more confident about internal operations. The London Royal Hospital had its first X-ray machine in 1896. X-rays also made it possible for surgeons to extract bullets and shrapnel without having to dig around in the wound. The importance was quickly recognised by surgeons, and mobile X-ray units were developed. Carbolic spray, the steam S steriliser, the X-ray machine and the hypodermic needle used in blood transfusions were also important. War and developments in surgery • In WW1, surgeons treated soldiers close to front line and they gained a lot of experience in a wide range of injuries and sometimes had to improvise new techniques. In this way, war can be said to accelerate their training. • New developments – explosive weapons meant people suffered deep wounds that caused infection. Surgeons found that cutting away infected tissue and soaking the wound in salt was the best way. Before WW1, most surgeons stayed away from working on the brain – too complicated. Surgeons did know that they needed to try something. • Harold Gillies asked for permissions to set up a plastic surgery unit in the British army. He began to work on ways of reconstructing facial injuries and paid attention to the attempt to create a normal appearance. He developed a new techniques of pedicle tubes. A narrow layer of skin was lifted up from the body and stitched into a tube at one end. The other end was still attached to the body and this meant blood continued to circulate and helped healthy skin to develop. When the tube had grown long enough, the free end was attached to the new site. Once the skin graft was in place, the pedicle tube could be cut free at the base. • Prosthetic limbs – between 1914 and 1921 over 41,000 men in the British armed forces lost a limb. Advances meant that the use of light metal alloys and new mechanisms, but there were long waiting lists for these to be fitted and patients then needed training to use them properly. Communications Journals – development of surgery depended on effective communication of findings, evidence and techniques. Surgeons had to convince others that their new methods were worth trying. Reports of new discoveries in medical journals, such as the one produce by the Royal College of Surgeons were important because: Most surgeons read the same journals Journals only published information that they though was based on good science. Pasteur published his germ theory that microbes in the air caused decay and infection, and Lister applied this idea to his attempts to reduce infection. Lister was able to build on Pasteur's work and communication helped surgery advance. Overcoming obstacles – journals also communicated problems with new techniques and criticisms of new ideas. The spread of ideas was an automatic process. Ideas were initially rejected or only accepted gradually. Remember when Semmelweiss tried to S improve hygiene, he was unsuccessful. Lister’s ideas were accepted more readily because Pasteur had published his germ theory. Some of the developments would probably have happened anyway. Ether had been such a breakthrough in surgery that when people realised the problems in using it they didn’t want to abandon anaesthetics but find a better one. Nevertheless, communication was not always effective. The spread of new ideas was sometimes restricted when people protected their new ideas from being copied. Newspapers – Public were interested in the developments of surgery. Newspapers reported on anaesthetics, Queen Victoria use of chloroform. These make useful sources for historians, but opinion was also important. Remember religious factors on using anaesthetics. The Lancet paper was very critical of the Queen having chloroform.