VCU Medicine-M&M 5.20.2014
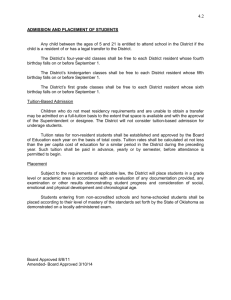
advertisement

VCU INTERNAL MEDICINE MORBIDITY AND MORTALITY May 20 2014 GOALS Discuss systems and individual issues creating barriers to delivery of patient care Help improve patient care Not to place blame or say who was at fault If you were involved with this case, please do not state your involvement in the case FORMAT Identify a case where there was a bad outcome, perhaps related to systems issues or human error. Review the case. Break into groups Small group brainstorm – why did things go wrong? Small groups present their findings in a large group discussion. Important to leave with root causes and possible solutions KEY ISSUES Documentation Review of secondary sources of information and historical documentation Transitions of care Escalation of care in a DNR/DNI pt HISTORY – ADMIT NOTE (TRANSFER) 68 yo man who presented one day prior to transfer to outside hospital from long-term care facility with AMS Per facility – several days AMS “per cousin” – several weeks No hypoglycemia, no acute illness At OSH, 130/70, 84, 16, afebrile Glucose 70-100 Chem notable for bicarb 35, cr 2.2, bun 94 (old) NH4 100 Head CT negative for intracranial hemorrhage CE elevated troponin 0.43, pro-BNP 9000, EKG afib, LAD, RBBB Pt transferred “for further management of ACS” Admission note done by intern #1 senior resident #1 HISTORY On arrival, pt oriented to self, nothing else, able to follow simple commands Note full code at OSH, made DNR/DNI after discussion with senior resident on admission Medical hx 8/13 cath – 60% EF, 8/13 echo EF 55% Afib, anemia, basal cell ca, cellulitis, CKD stage 3, diastolic HF, DM, edema, hyperlipidemia, htn, MRSA leg wounds 2012, obesity, sinusitis, URI HISTORY- PMHX 8/13 cath – 60% EF, 8/13 echo EF 55% Afib Anemia basal cell ca cellulitis CKD stage 3 diastolic HF DM hyperlipidemia HTN MRSA leg wounds Obesity Sinusitis URIs edema HISTORY Meds: Percocet Albuterol nebs and HFA ASA Atorvastatin Ca-Vit D Iron Hydralazine Lantus ISMN Metolazone Warfarin pantoprazole FHx – cousins with CAD, parents deceased SHx – lives in SNF since Nov 2013, no independent ADLs, no substance use, not married, no kids PE ON ADMISSION PE: VS – 36.6, 145/68, 79, 12 NAD, oriented x 1 PERRL, EOMI, anicteric sclera, dry MM, goiter Irreg irreg, no murmurs, 2+ edema Diminished BS bilat, no wheezing, nonlabored Abd – benign Neuro – CN 2-12 grossly intact, follows simple commands Psych - cooperative ADMIT LABS 7.51/36/199/29 Na 148, k 4.0, bicarb 34, bun 97/cr 2.2 Hgb 9, wbc 10.7, plt 264 Alb 2.4, lfts otw unremarkable INR 2.6 Troponin 0.72 to 0.64 overnight Ua with large leuk, pos nitrite, wbc 14, few bacteria A/P - ADMIT AMS – likely secondary to UTI, evaluate for other causes – endocrine, infection, metabolic, consider MRI if not improved Type 2 NSTEMI – secondary to demand ischemia secondary to infection Decompensated diastolic CHF Permanent A fib CKD HTN Admission note done by intern #1, senior resident #1 SPEECH PATHOLOGY NOTE DAY 1 -“Consulted for bedside swallowing eval in setting of AMS -Current diet: NPO; team having difficulty passing NGT due to pt’s inability or unwillingness to flex neck -Pt speaking in 1-2 word utterances, inconsistently responsive, oriented to name, month, date of birth” DAY 2 – ATTENDING NOTE No events overnight Mental status unchanged Not verbal (resident note says unresponsive) SBP 120-130, HR 80s, RR 16, tmax 37.3 No jvd, few rhonchi, irreg irreg, abd benign Labs reviewed – new pos bcx – gpc; no leukocytosis, hgb stable, tsh nl Resident #2 DAY 2 RESIDENT NOTE A/P Mild troponin elevation in setting of CKD and severe HFpEF HFpEF Chronic AF with controlled VR AMS with baseline cognitive decline – per cousin he can speak and eat – with UTI, other w/u neg so far DMII Speech eval noted hypernatremia Daily note – resident #2 HOSPITAL DAY 3 No significant change in exam or labs except urine cx positive Pseudomonas No significant change in plans except addition of cefepime for Pseudomonas UTI and vanc for gpc in blood Transfer to medicine HOSPITAL DAY #3 Resident #3 (sister team - covering for admitting team) writes transfer note Reviews details to date – no new plans or assessment HOSPITAL DAY #4 Resident #4 (team resident) is of f Intern #2 (med team intern) writes daily note Attending writes addendum AMS - apparently pt has had increasing AMS at nursing facility for several weeks. Etiology of altered mental status is unclear - ? infection (has current UTI as noted below - just started on appropriate abx for sensitivities) vs metabolic (Na on admission elevated, BUN is chronically elevated in 70-100 range, need to check NH4) vs endocrine (note TSH nl, consider cortisol eval) vs primary CNS such as fall and SDH (note neg CT done - does have chronic changes and evidence of chronic small vessel ischemic disease) vs meds/toxins (no clear evidence of specific agent and neg UDS on admission) vs other. At this point, we are treating for infection and hypernatremia and following MS closely. He does have a cough response but needs to be monitored closely. Continue to obtain further hx from family to identify any other possible etiologies - will contact nursing facility to review list of meds again though, per extensive review of medical chart, cannot identify specific offending med at this time. Appears that baseline one year ago was living independently, since admission last summer, has been in SNF but still fairly functional. HOSPITAL DAY #5 Full medicine team present on rounds Middle of rounds – acute respiratory distress Sr Resident (#4)– MRICU consulted, however cancels MRICU consult, states “comfort care only”(Impression per handoff from resident #3) Attending disagrees after chart review night prior – sees potentially reversible causes that should be evaluated and treated – with overall time trial LATER – HOSPITAL DAY #5 Cousin brings in a diary documenting functional status over past six months –pt had done taxes one month prior HOSPITAL DAY #5 Discussion on rounds Evaluation (thorough) of AMS, including EEG, MRI DNR/DNI, no escalation of care (pressors, intubation, hemodialysis, etc) – discussed with family – but aggressive evaluation with time trial of evaluation and therapy HOSPITAL DAY #6 Seen on rounds – no change in exam No new results Identified need for LP Not done that day due to coagulopathy HOSPITAL DAY #7 EEG results called to attending c/w encephalopathy/encephalitis LP attempted – unsuccessful – IR called HOSPITAL DAY 8 LP not done on day 7 - coagulopathy and IR delay Done on day 8 Crypto Ag 1:20, serum crypt Ag – 1:2450 Ampho and flucytosine started ID consulted – agree with plan Over next three days- starts responding with tracking, verbal responses SMALL GROUP DISCUSSIONS Modified Root Cause Analysis KEY ISSUES Documentation Review of secondary sources of information and historical documentation Transitions of care Escalation of care in a DNR/DNI pt LARGE GROUP DISCUSSION Was there a medical error in the adverse event that occurred in today’s discussion? Was that error preventable? What were the health system forces that contributed to the error? How can those systems be changed to prevent a similar adverse event from occurring in the future? LARGE GROUP DISCUSSION Was there a cognitive error that contributed to the error? How would you address the cognitive error? Please recommend one course of action that our institution can take to prevent an event like this in the future. Who else should be involved in this process? What would be the role of the residents and students?