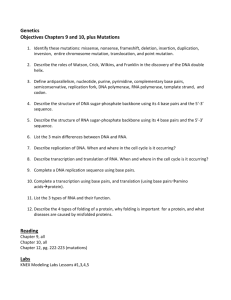
biochem ch 18 [3-12
advertisement

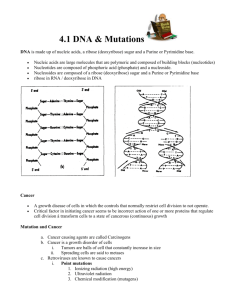
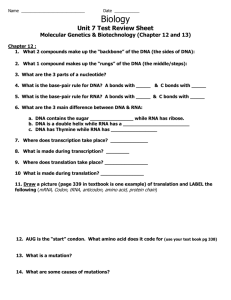
Causes of Cancer Philadelphia chromosome – translocation between chromosomes 9 and 22 (piece of 22 on 9) that gives rise to CML (chronic myelogenous leukemia) Cancer – group of disease where cells no longer respond to normal restraints on growth o Normal cells stop proliferating with cell-cell contact (contact inhibition) o Cancer cells don’t require growth-stimulatory signals and are resistant to growth-inhibitory signals o Have infinite proliferative capacity and don’t become senescent o Lose anchorage dependence (can grow without support of ECM or structural support) Patients with leukemia experience various hemorrhagic manifestations caused by decreased number of platelets o Because of uncontrolled proliferation of WBCs within limited space of marrow, megakaryocytes in marrow squeezed and fail to develop into mature platelets o Number of mature thrombocytes in circulation falls, and thrombocytopenia develops Malignant neoplasms of epithelial cell origin called carcinomas If cancer grows in gland-like pattern, they are adenocarcinomas Melanocarcinoma or melanoma – carcinoma arising from melanocytes Criteria for cells to be classified “transformed” (from benign to cancerous) o Serum in cell culture medium stimulates cell growth Transformed cells have reduced requirement for serum (liquid fraction of clotted blood that contains factors for cell proliferation) o Ability to grow without attachment to supporting matrix (can grow suspended in soft agar mixture) o Ability of cells to form tumors when injected into mice that lack immune system For every gene that causes cancer (oncogene), there is a corresponding cellular gene (proto-oncogene) o Ras oncogene comes from c-ras proto-oncogene; found in bladder carcinoma, lung and colon tumors Common wart is benign tumor formed from slowly expanding mass of cells; nevi are tumors of skin formed by melanocytes that have been transformed from highly dendritic single cells interspersed among other skin to round oval cells that grow in aggregates (nests) Malignant neoplasm is proliferation of rapidly growing cells that progressively infiltrate, invade, and destroy surrounding tissue Tumors develop angiogenic potential Transformation of normal cell to cancer cell begins with damage to DNA; mutations result from damaged DNA not repaired properly or not repaired before replication o When cell with one mutation proliferates, clonal expansion results in substantial population of cells containing this mutation o With each clonal expansion, probability of another transforming mutation increases o Because mutations accumulate in genes that control proliferation, subsequent mutations occur even more rapidly until cells acquire multiple mutations necessary for full transformation Transforming mutations occur in genes that regulate cell proliferation and differentiation (proto-oncogenes), suppress growth (tumor suppressor genes), tell irreparably damaged cells to apoptosis, or repair damaged DNA Damage to DNA Leading to Mutations Alteration in chemical structure of DNA (sequence of bases in gene) absolute requirement for development of cancer; function of DNA depends on presence of polar chemical groups in DNA bases o O and N atoms in DNA bases are targets for various electrophiles Chemical carcinogens generally stable lipophilic compounds that must be activated by metabolism in body to react with DNA o Many chemotherapeutic agents (designed to kill proliferating cells by interacting with DNA) may act as carcinogens and cause new mutations and tumors while eradicating the old Exposure to radiation and UV light causes formation of pyrimidine dimers (can cause all types of skin cancer) o Wavelength of UV light most associated with skin cancer is UVB, which forms pyrimidine dimers o Pyrimidine dimers repaired by nucleotide excision repair pathways that require products of at least 20 genes; excessive exposure to sun, and nucleotide excision repair pathway overwhelmed and some damage remains unrepaired Proto-oncogenes converted to oncogenes by mutations in DNA that cause gain of function o Radiation and chemical carcinogens act by causing mutation in regulatory region of gene, increasing rate of production of proto-oncogene protein, or by producing mutation in coding portion of oncogene that results in synthesis of protein of slightly different amino acid composition capable of transforming o Entire proto-oncogene or portion of it may be transposed or translocated; in new location, protooncogene may be under control of promoter that is regulated differently, allowing the gene to be expressed in tissue where it is not normally expressed or at higher-than-normal levels of expression If only portion of proto-oncogene translocated, it may be expressed as truncated protein with altered properties or may fuse with another gene and produce a fusion protein Truncated or fusion protein may be hyperactive and cause inappropriate cell growth o Proto-oncogene may be amplified so multiple copies of gene produced in single cell; if more genes active, more proto-oncogene protein will be produced, increasing growth rate of cells Oncogene N-myc (cell proliferation transcription factor related to c-myc) amplified in some neuroblastomas Amplification of erb-b2 oncogene (growth factor receptor) seen in several breast cancers o If oncogenic virus infects cell, its oncogene may integrate into host cell genome, permitting production of abnormal oncogene protein; cell may be transformed and exhibit abnormal pattern of growth Virus can insert strong promoter into host cell genome, which may cause increased or untimely expression of normal proto-oncogene Burkitt lymphoma – general name for several types of B-cell malignancies; results form translocation between chromosomes 8 and 14; translocation moves proto-oncogene transcription factor c-myc to chromosome 14, where it becomes under control of promoter region for immunoglobulin heavy-chain gene, which leads to inappropriate and overexpression of c-myc o Results in uncontrolled cell proliferation and tumor development o All subtypes contain this translocation o Epstein-Barr virus infection of B cells associated with certain types of Burkitt lymphoma Errors repaired before replication don’t become mutagenic (thank you, DNA repair enzymes) Inherited mutations in tumor suppressor genes BRCA1 and BRCA2 predispose women to development of breast cancer; protein products of these genes play roles in DNA repair, recombination and regulation of transcription HNPCC (hereditary nonpolyposis colorectal cancer) results from inherited mutations in enzymes involved in DNA mismatch repair systems Philadelphia chromosome creates fusion protein that contains N-terminal region of Bcr protein from chromosome 22 and C-terminal region of Abl protein from chromosome 9 o Abl is proto-oncogene, and resulting Bcr-Abl loses regulatory region and is constitutively active, resulting in deregulated tyrosine kinase activity o When active Abl stimulates Ras pathway of signal transduction, leading to cell proliferation Oncogenes Proto-oncogenes encode proteins that are growth factors, growth factor receptors, signal transduction proteins, transcription factors, cell cycle regulators, and regulators of apoptosis Nomenclature – oncogene is lowercase and italics (myc) while protein product is capitalized only (Myc) Mutations in oncogenes that give rise to transformation usually gain-of-function mutations miRNAs can behave as oncogenes if overexpressed (increased function) if its target (which would exhibit reduced expression) is protein involved in inhibiting cell proliferation Growth factors bind to cellular receptors on PM and stimulate signal transduction pathway that activates transcription of certain genes; if too much growth factor or growth factor receptor, target cells respond by proliferating inappropriately o Growth factor receptors may become oncogenic through translocation or point mutations in domains that affect binding of growth factor, dimerization, kinase activity, or some other aspect of signal transmission; receptor transmits proliferative signal even without normal ligand o Gene for human epidermal growth factor receptor overexpressed in 10-20% of breast cancer cases; prognosis poor because patients display shorter disease-free intervals, increased risks for metastasis, and resistance to therapy Herceptin – monoclonal antibody with specificity for HER2 protein on receptor; blocks receptor’s action; not all tumors responsive to herceptin Genes that encode proteins involved in growth factor signal transduction cascades may be proto-oncogenes o Binding of growth factor leads to activation of Ras; when Ras binds GTP, it is active, but Ras slowly inactivates itself by hydrolyzing bound GTP to GDP and Pi, controlling length of time Ras active Ras, when active, activates Raf (MAP kinase kinase kinase), which activates MEK (MAP kinase kinase), which activates MAP kinase Activation of MAP kinase results in phosphorylation of cytoplasmic and nuclear proteins, followed by increased transcription of transcription factor proto-oncogenes myc and fos Mutations in genes for any proteins that regulate MAP kinase activity, as well as proteins induced by MAP kinase activation, can lead to uncontrolled cell proliferation Many transcription factors (Myc and Fos) are proto-oncoproteins (products of proto-oncogenes) o MAP kinase induces myc and fos as well as directly activates AP-1 transcription factor through phosphorylation o AP-1 is heterodimer formed by protein products of fos and jun families of proto-oncogenes o Targets of AP-1 activation are genes involved in cellular proliferation and progression through cell cycle (as are targets of myc transcription factor) o Synthesis of transcription factor C-myc tightly regulated in normal cells; expressed only during S phase of cell cycle In large numbers of tumor types, regulated expression lost, and c-myc becomes inappropriately expressed or overexpressed throughout cell cycle, driving cells to continuously proliferate o Net result of alterations in transcription factors is increased production of proteins that carry out processes required for proliferation Activators of DNA replication and cell division work through cyclins and cyclin-dependent kinases (CDKs) that control progression from one phase of cycle to another o CDKs made constantly throughout cell cycle but require binding of specific cyclin to be active o Different cyclins made at different times in cell cycle control each transition (G1/S, S/G2, G2/M) o Activity of cyclin-CDK complex regulated through phosphorylation and inhibitory proteins (CKIs) CKIs slow cell cycle progression by binding and inhibiting cyclin-CDK complexes o CDKs controlled through activating phosphorylation by CAKs and inhibitory hyperphosphorylation kinases At G1/S checkpoint – because cell committed to DNA replication and division once it enters S phase, multiple regulatory proteins involved in determining whether cell ready to pass this checkpoint o In quiescent cells, Rb (retinoblastoma gene product) complexed with E2F (group of transcription factors collectively called this), resulting in inhibition of E2F family o Upon growth factor stimulation, cyclin Ds induced and bind to cdk4 and cdk6 (produced throughout cell cycle), converting them to active protein kinases) o One of targets of cyclin/CDK phosphorylation is Rb protein, which releases it from E2F, and E2F free to activate transcription of genes required for entry into S Rb protein is tumor suppressor gene o Proteins induced by E2F include cyclin E, cyclin A, cdc25A (activating protein phosphatase), and proteins required to bind at origins of replication to initiate DNA synthesis Synthesis of cyclin E allows it to complex with cdk2, which hyperphosphorylates Rb protein, keeping Rb in inactive state Cyclin A complexes with Cdk2, which phosphorylates and inactivates E2F family, ensuring signals not present for extended periods of time o Progression through cell cycle opposed by CKIs CKIs regulating cyclin/CDK expression in G1 phase are either in Cip/Kip family or INK4 family Cip/Kip family members have broad specificity and inhibit all cyclin-CDK complexes INK4 family specific for cyclin D-cdk4/6 family of complexes Some CKIs induced by DNA damage to cell and halt cell cycle progression until damage can be repaired (CKI p21 responds to specific signals to block cell proliferation) If damage can’t be repaired, cell undergoes apoptosis Tumor Suppressor Genes Tumor suppressor genes encode proteins that inhibit proliferation in response to certain signals (DNA damage) o Signal removed when cell fully equipped to proliferate o Can affect cell cycle regulation, signal transduction, transcription, and cell adhesion o Products frequently modulate pathways activated by products of proto-oncogenes Tumor suppressor genes contribute to development of cancer when both copies of gene inactivated (different from proto-oncogenes and miRNAs because only one of them needs to be mutated to initiate transformation) o miRNAs can be either oncogenes (overexpression) or tumor suppressors (loss of function) depending on genes they regulate Rb functions in transition from G1 to S phase and regulates activation of E2F; if person inherits mutated copy of rb allele, that person will develop retinoblastoma because of high probability that second allele of rb will gain mutation (familial retinoblastoma) o Those who develop rb mutation on their own have sporadic retinoblastoma and acquire 2 specific mutations during their lifetime p53 protein – transcription factor that regulates cell cycle and apoptosis; p53 halts replication in cells that have suffered DNA damage and targets unrepaired cells for apoptosis o In response to DNA-damaging mutagen, level of p53 rises and stimulates transcription of p21 (member of Cip/Kip family of CKIs); p21 gene product inhibits cyclin-CDK complexes, preventing phosphorylation of Rb and release of E2F proteins, preventing cell from entering S phase o p53 stimulates transcription of DNA repair enzymes (i.e., GADD45) o If DNA successfully repaired, p53 induces its own downregulation through activation of mdm2 gene; if DNA repair not successful, p53 activates Bax and IGF-BP3, involved in apoptosis IGF-BP3 protein product binds receptor for insulinlike growth factor, which induces apoptosis by blocking antiapoptotic signaling by growth factors, and cell enters growth factor deprivation o Inheritance of mutation in p53 leads to Li-Fraumeni syndrome (characterized by multiple types of tumors) Mutations in p53 present in more than half tumors, which are secondary mutations within cell If p53 mutated, overall rate of cellular mutation will increase because there is no p53 to check for DNA damage, initiate repair of damaged DNA, or initiate apoptosis if damage not repaired Ras family of proteins involved in signal transduction for many hormones and growth factors; activity of pathways interrupted by GAPs, which vary among cell types o Neurofibromin (product of tumor suppressor gene NF-1) is nervous system-specific GAP that regulates activity of Ras in neuronal tissues; growth signal transmitted so long as Ras protein binds GTP Binding of NF-1 to Ras activates GTPase domain of Ras, which hydrolyzes GTP to GDP, inactivating it Without functional neurofibromin molecule, Ras perpetually active o Inherited mutation in NF-1 can lead to neurofibromatosis (disease primarily of numerous benign painful tumors of nervous system) Patched and smoothened coreceptor genes encode receptor for hedgehog class of signaling peptides o Coreceptors normally function to control growth during embryogenesis o Patched receptor protein inhibits smoothened (its coreceptor protein) o Binding of hedgehog ligand to patched releases inhibition of smoothened, which transmits activating signal to nucleus, stimulating new gene transcription o Smoothened is proto-oncogene, and patched is tumor suppressor gene o If patched loses function, smoothened can signal cell to proliferate, even in absence of hedgehog o If smoothened undergoes gain-of-function mutation, it can signal in absence of hedgehog signal, even in presence of patched o Inherited mutations in either will lead to increased incidence of basal cell carcinoma Cadherin family of glycoproteins mediates calcium-dependent cell-cell adhesion; form intercellular complexes o Anchored intracellularly by catenins, which bind to actin filaments o Loss of E-cadherin expression contributes to ability of cancer cells to detach and migrate (metastasis) Individuals who inherit mutation in E-cadherin (CDH1) predisposed to developing diffuse-type gastric cancer o Catenin proteins also act as transcription factors o β-catenin binds to complex that contains regulatory protein (APC), activating it for degradation When appropriate signal inactivates APC, β-catenin levels increase, and it travels to nucleus where it activates myc or cyclin D1 transcription, leading to cell proliferation o APC is tumor suppressor gene; if inactivated, it can’t bind β-catenin and inhibit cell proliferation Mutations in APC or proteins that interact with it found in most sporadic colon cancers Inherited mutations lead to familial adenomatous polyposis (FAP) Cancer and Apoptosis After apoptosis, phosphatidylserine (lipid on inner leaflet of PM) exposed on external surface of apoptotic vesicles and is one of phagocytic markers recognized by macrophages and other nearby phagocytic cells Apoptosis divided into initiation phase, signal integration phase, and execution phase o Can be initiated by death receptors (TNF), deprivation of growth hormones, mitochondrial damage, and irreparably damaged DNA o Signal integration phase balances proapoptotic signals against antiapoptotic cell survival signals by members of Bcl-1 family of proteins o Execution phase carried out by caspases Caspases present in cell as procaspases; divided into initiator caspases (specifically cleave other procaspases) and execution caspases (cleave other cellular proteins involved in maintaining cellular integrity) o Initiator caspases activated through death receptor pathway and mitochondrial integrity pathway; activate execution caspases, which cleave protein kinases involved in cell adhesion, lamins that form inner lining of nuclear envelope, actin and other cell structure proteins, and DNA repair enzymes o Cleave inhibitor protein of endonuclease CAD, activating it to initiate degradation of cellular DNA o With destruction of nuclear envelope, Ca2+ and Mg2+-dependent endonucleases also activated Death receptors subset of TNF-1 receptors that includes Fas/CD95, TNF-R1, and DR3 o Receptors form trimer that binds TNF-1 or another death ligand on external domain and binds adaptor proteins to intracellular domain o Activated TNF-receptor complex forms scaffold binding 2 molecules of procaspase 8 (or procaspase 10), which autocatalytically cleave each other to form active caspase Caspases 8 and 10 are initiator caspases that activate execution caspases 3, 6, and 7 o Caspase 3 also cleaves Bcl-2 protein (Bid) to form that activates mitochondrial integrity pathway Growth factor withdrawal, cell injury, release of certain steroids, and inability to maintain low levels of intracellular Ca2+ all lead to release of cytochrome c from mitochondria o Cytochrome c loosely bound to outside of inner mitochondrial membrane; release initiates apoptosis o In cytosol, cytochrome c binds Apaf; Apaf/cytochrome c complex binds caspase 9 (initiator) to form active apoptosome complex, which activates execution caspases (3, 6, and 7) by zymogen cleavage Bcl-2 family members decision makers that integrate pro-death and anti-death signals to determine whether cell should undergo apoptosis; both pro-apoptotic and anti-apoptotic members of Bcl-2 family exist o Anti-apoptotic factors contain all 4 domains (BH1-BH4), channel-forming pro-apoptotic factors contain BH1-BH3, and prop-apoptotic BH3-only family members o Anti-apoptotic Bcl-2-type proteins (Bcl-2, Bcl-L, and Bcl-w) can either insert into outer mitochondrial membrane to antagonize channel-forming pro-apoptotic factors (decreasing cytochrome c release) or can bind cytoplasmic Apaf so it can’t form apoptosome complex o Ion channel-forming members (such as Bax) don’t contain binding factor for Apaf, so when they dimerize with BH3-only members in outer mitochondrial membrane, they form ion channel that promotes cytochrome c release rather than inhibiting it o BH3-only proteins (Bim and Bid) contain only structural domain that allows them to bind other Bcl-2 family members and not domains for binding to membrane, forming ion channels, or binding to Apaf Binding activates pro-death family members and inactivates anti-apoptotic members o When cell receives signal from pro-death agonist, BH3 protein (like Bid) activated, which then activates Bax (ion-channel-forming), which stimulates release of cytochrome c At same time Bid is activating Bax, it binds Bcl-2, disrupting Bcl-2/Apaf complex, freeing Apaf to bind to released cytochrome c to form apoptosome o When Bcl-2 mutated, it is usually overexpressed (i.e., in follicular lymphoma or CML); overexpression disrupts normal regulation of pro-apoptotic and anti-apoptotic factors in favor of anti-apoptotics, leading to inability to destroy cells with damaged DNA Bcl-2 is multidrug-resistant transport protein and, if overexpressed, will block induction of apoptosis by antitumor agents by rapidly removing them from cell Activation of growth factor-dependent signaling pathways that inhibit apoptotsis, such as PDGF/Akt/BAD pathway can cause apoptosis-resistance in cancer cells o Nonphosphorylated BAD acts like Bid in promoting apoptosis; binding of PDGF to receptor activates PI-3 kinase, which phosphorylates and activates serine-threonine kinase Akt o Activation of Akt results in phosphorylation of pro-apoptotic BH3-only protein BAD, which inactivates it o One of features of neoplastic transformation is loss of growth factor dependence for survival o MAP kinase pathway sends cell survival signals o MAP kinase kinase phosphorylates and activates RSK, which phosphorylates BAD and inhibits its activity o Gain-of-function mutations in genes that control these pathways (such as ras) create apoptosis-resistant cells Bcl-2 levels regulated by miRNAs (miR-15 and miR-16); if expression of these miRNAs altered, Bcl-2 levels altered, promoting either apoptosis (if Bcl-2 levels decrease) or cell proliferation (if Bcl-2 levels increase) o Loss of both miRNAs found in majority of chronic lymphocytic leukemia (CLL) cells o Loss of miR-15 and miR-16 expression leads to increase in Bcl-2 levels, favoring cell proliferation miR-21 regulates expression of PDCD4, which is upregulated during apoptosis and blocks translation o Loss of miR-21 activity leads to cell death (PDCD4 would be overexpressed) o Overexpression of miR-21 would be anti-apoptotic (PDCD4 expression ablated) miR-17 cluster regulates PKB/akt pathway by regulating levels of PTEN (enzyme that converts PIP3 to PIP2), as well as levels of E2F family o Upregulation of miR-17 would decrease PTEN levels, and cellular proliferation favored because of constant activation of akt pathway Cancer Requires Multiple Mutations Single change in one oncogene or tumor suppressor gene not adequate for transformation o If cells derived from biopsy specimens of normal cells not immortalized (able to grow in culture indefinitely), addition of ras oncogene to cells not sufficient for transformation; additional mutations in combination of oncogenes (ras and myc together) can result in transformation o 4-7 mutations required for normal cells to be transformed Cells accumulate multiple mutations through clonal expansion; when DNA damage occurs in normally proliferative cell, population of cells with that mutation produced; expansion of mutated population increases probability of second mutation in cell containing first mutation o After one or more mutations in proto-oncogenes or tumor suppressor genes, cell may proliferate more rapidly in presence of growth stimuli and further mutations grow autonomously (independent of normal growth controls) o Enhanced growth increases probability of further mutations At the Molecular Level, Cancer is Many Different Diseases Particular type of cancer can arise in multiple ways (patched and smoothened are receptor and coreceptor for signaling peptide sonic hedgehog; mutation of smoothened or inactivation of patched can give rise to basal cell carcinoma) TGF-β and its signal transduction proteins Smad4/DPC part of same growth-inhibiting pathway; either may be absent in colon cancer Treatments successful in some patients may not work in others because of these types of variations Treatment for CML – fusion protein Bcr-Abl found only in transformed cells that express Philadelphia chromosome and not in normal cells o Gleevec – drug designed to specifically bind to and inhibit only active site of fusion protein, not normal proteins; stops cell proliferation, and induces apoptosis in some cells o Some patients suffered relapses and Bcr-Abl proteins in these patients had single amino acid substitution near active site that prevented Gleevec from binding to protein o Other tyrosine kinase inhibitors (dasatinib and nilotinib) can be used in treating CML if resistance to Gleevec encountered Viruses and Human Cancer HTLV-1, HIV, and hepatitis C – retroviruses associated with development of cancer Hepatitis B, Epstein-Barr virus (EBV), HPV, and herpes (HHV-8) – DNA viruses associated with cancer HTLV-1 causes adult T-cell leukemia; HTLV-1 genome encodes protein Tax, which is a transcriptional coactivator o Cellular proto-oncogenes c-sis and c-fos activated by Tax, altering normal controls on cellular proliferation and leading to malignancy, making tax a viral oncogene HIV infection leads to immunosuppression, and consequently, loss of immune-mediated tumor surveillance o HIV-infected individuals predisposed to non-Hodgkin lymphoma, which results from overproduction of T-cell lymphocytes o HIV genome encodes Tat (transcription factor that activates transcription of IL-6 and IL-10 genes in infected T cells o IL-6 and IL-10 are growth factors that promote proliferation of T cells, and their increased production contributes to development of non-Hodgkin lymphoma o Tat can be released from infected cells and act as angiogenic growth factor, contributing to development of Kaposi sarcoma Chronic hepatitis B infections lead to hepatocellular carcinoma EBV associated with B-cell and T-cell lymphomas, Hodgkin disease, and other tumors o EBV encodes Bcl-2 protein that restricts apoptosis of infected cell HHV-8 associated with Kaposi sarcoma Biochemical Comments TNM system standardizes classification of tumors: T (stage of tumor; the higher the number, the worse the prognosis), N (number of lymph nodes affected by tumor), and M (presence of metastasis; 0 for none, 1 for presence of metastatic cells) Mutations associated with malignant melanomas include ras (gain of function in growth signal transduction oncogene), p53 (loss of function of tumor suppressor gene, p16 (loss of function in Cdk inhibitor tumor suppressor gene), Cdk4 (gain of function in cell cycle progression oncogene), and cadherin/ β-catenin regulation (loss of regulation that requires attachment) HNPCC and hereditary breast cancer both result from inherited mutations in genes involved in DNA repair o HNPCC can be caused by any of 5 mutations in genes that play role in DNA mismatch repair (all act as tumor suppressors, so loss of function required for tumor to develop) Lack of DNA mismatch repair enzyme doesn’t directly lead to cancer (such as activating mutation in myc would) o Lack of functional mismatch repair system increases frequency at which new mutations introduced into somatic cells (particularly rapidly proliferating cells such as colonic epithelium), such that eventually mutation will result in gene necessary for proper growth control Familial breast cancer traced to inherited mutations of BRCA1 and BRCA2 o BRCA1 acts as tumor suppressor; biochemical function is to participate in response to DNA damage Phosphorylated by various kinases, each of which activated by different form of DNA damage Primarily involved in repairing double-strand breaks in DNA and transcription-coupled repair Once BRCA1 phosphorylated, it signals for cell cycle arrest to allow DNA damage to be repaired Women with BRCA1 mutation have 80% risk of developing breast cancer and 40% risk of developing ovarian cancer; men with BRCA1 mutation don’t develop breast cancer o BRCA2 required for DNA double-strand break repair, usually caused by ionizing radiation Loss of activity required for cancer to develop (tumor suppressor) Required for homologous recombination between sister chromatids during meiosis and mitosis Linked to increased incidence of breast cancer in both men and women; increased ovarian cancer in women PARP-1 inhibitors being tested to be used for treatment of BRCA1 and BRCA2-induced breast cancers o Double-strand break repair occurs either by homologous recombination (requiring activities of BRCA1 and BRCA2 proteins) or through non-homologous end-joining (NHEJ; error-prone process caused by trimming of DNA ends before ligation) o Single-strand breaks in DNA more common than double-strand breaks; cellular repair mechanism dependent on PARP-1, which produces large branched chains of poly (ADP-ribose) (derived from NAD+) at site of damage, which acts as docking station for proteins involved in repairing single-strand break Inhibiting PARP-1 leads to accumulation of single-strand breaks in DNA o o PARP-1 inhibitors effective in killing BRCA1 or BCRA2 mutated cells in that when single-strand breaks not repaired, they’re often converted to double-strand breaks when replisome tries to replicate through break; in cell lacking BRCA1 or BCRA2 activity, only way DNA can be repaired is by NHEJ, which is errorprone process, leading to cells accumulating large number of mutations, eventually leading to cell death Cells with functional BRCA1 and BRCA2 activity don’t die