Data Element Sets
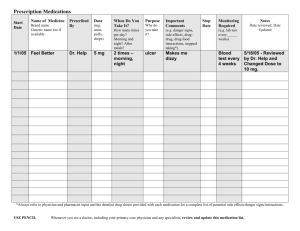
advertisement

Data Element Sets *Notes included for Standards Analysis WG *Note: Privacy and security are important, but out of scope for this WG. *Note: When applicable, data type is designated in front of the element in parentheses – e.g. (PN) for Person Name. When not clear if a data type is sufficient, Structure is used to indicate that a class may be necessary to model the concept. If something is not available within the ISO data types, Gap is used to indicate such an issue. Demographics Patient Information (PN) Name: Last Name, Middle Name, First Name *Note: Accommodate additional names: Given Name/Family Name/Suffix/Prefix (CE) Gender (Administrative) (II or structure + II) Patient Identifiers (everything currently legally used in an MPI algorithm, e.g. Reconciling and Managing EMPI) (PN) Mother’s Maiden Name (CE) Marital Status: Married; Married Polygamous; Civil Union; Single; Divorced; Widowed (TS) Date of Birth: Month, Day, Year Culturally Sensitive Patient Care (CE) Race (value set included, insert coding term) (CE) Ethnicity (value set included, insert coding term) (CE) Religion (value set included, insert coding term) (Structure) Language (value set included, insert coding term) *Note: needs to include level of comprehension (Structure) Disability (value set included, insert coding term) (CE) Educational Level (value set included, insert coding term) Patient Contact Information (indicate the preferred method of communication) (AD) Home Address (TELECOM) Home Phone (Gap) Text Message (Yes or No) (TELECOM) Cell Phone (Gap) Text Message (Yes or No) (TELECOM) Work Phone (Gap) Text Message (Yes or No) (TELECOM) Primary Email Address (TELECOM) Secondary Email Address (TELECOM) DIRECT Address (TELECOM) Patient Portal/PHR URL, if Yes Existence of Advanced Directives *Note: Has an advanced Directive has been signed by the patient, and is contained in records (Yes or No) Data type: BL Primary Care Physician (PCP) and Designated Providers PCP and Designated Providers (PN) Names (Structure) Patient’s Medical Home (where the patient sees their PCP or designated providers) *Note: This is a service delivery location, with the corresponding attributes (Structure) Specialties *Note: Role class with corresponding attributes (II) National Provider Identifiers (NPI) (Structure) Domain of Management (Structure) Contact Information *Note – the same elements as the patient information Support Contacts Emergency Contact (Primary) (PN) Name (Structure + CE) Relationship (Friend, Relative or Other) (Structure) Contact Information *Note – the same elements as the patient information Emergency Contact (Secondary) (PN) Name (Structure + CE) Relationship (Friend, Relative or Other) (Structure) Contact Information *Note – the same elements as the patient information Payer Information (Structure) Insurance (Primary) Information (Structure) Insurance (Secondary) Information Active Medication List **Reconciliation means that the provider who upon completion of their care of the patient sends an active medication list either having reviewed the original active medication list relative to any new prescribed or changes to medications and reconciled the active medication list or not. (provide examples) Assuming reconciliation, discontinued medications would be available separately, not as part of the active medication list. Q. What does it mean for a medication to be active? – clinically relevant medications Active Medications Going Forward List includes: PRN Medication List Active Medications (Held for Period of Time) Medications that patient was exposed to, now discontinued, but still clinically relevant Software need – document the delta (Structure) Active Medication List (BL) Reconciled (Yes/No) (TS) If Yes, Date of Reconciliation (Structure) Reconciled by? Date/Time Stamp (Structure) Discontinued Medication in this encounter (Structure) Changed Medication (CE) Medication Code (coded field that includes text) *Note: Appropriate coding system, not medication (Structure) Dose (must be able to include variable dosages e.g. sliding scales, etc.) (ST) When to take (Sig) (GTD) Frequency (Sig) (CE) Route (Sig) (IVL<TS>) Duration (Sig) (ST) Patient Instructions (Structure) PRN (Sig) (TS) Start Date (TS) Stop Date, if applicable (Structure) Prescriber *Note: See provider structure in Demographics (Structure + CE) Associated Assessment (ICD code, SNOMED) *Note: Reason the provider prescribed the medication Active Problem List *Note: What clinician sending the message has determined to be the patient’s active problems and/or diagnoses or determination of no known problems – this list may be reconciled at each ToC. (CD) Coded Problem(s) or no known problem(s) (TS) Start Date (or date of onset) of Problem (Structure + TS) Clinician who added it to the problem list (include date/time stamp) *Note: See provider structure in Demographics (BL) Reconciled (Yes or No) (Structure + TS) Reconciled by? Date/Time Stamp *Note: See provider structure in Demographics (Structure)Resolved and/or changed problems in this encounter Intolerances including Allergies (Structure) Medication (ingredient or class code, if available) that has been attributed to an allergic reaction or intolerance, or drug code if attribution to ingredient or class is unavailable *Note: Includes medications, biologicals, herbal supplements, OTCs, vaccine, etc. (Structure) Environmental Allergens *Note: Examples of environmental allergens include latex, pollen, animal dander, etc. (Structure) Food Allergens *Note: Examples of food allergens include shellfish, eggs, peanuts, etc. (Structure) Reaction (can have multiples) (Structure) Severity associated with the reaction (TS) Date Identified (Structure + TS) Who Reported (e.g. patient, provider, care taker) *Note: See provider structure in Demographics *Note: Not required for clinician to fill field