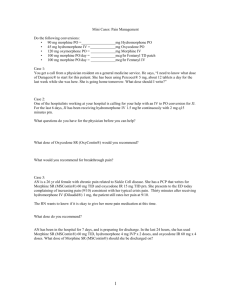
New Concepts in Pain Management
advertisement

New Concepts in Pain Management Melanie Christina, M.D. Presbyterian Hospital Dallas Medical Director, Heartland Hospice Definition: Pain An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage Pain is subjective. There is no neurophysiological or chemical test that can measure pain. INTERNATIONAL ASSOCIATION FOR THE STUDY OF PAIN Prevalence of Pain Over 30 million Americans suffer from chronic nonmalignant pain 20-30% of the American public suffer from acute or chronic pain Over 70% of patients with advanced cancer report having moderate to severe pain Barriers in the treatment of Pain Inadequate assessment Specific populations more likely not to be treated Patient’s reluctance to report pain Patient’s reluctance to take opioids Doctor’s reluctance to prescribe opioids – Fear of regulatory scrutiny – Fear of causing addiction – Lack of knowledge regarding dosing and side effects Important concepts to Understand Addiction – Psychological dependence on substances for their psychic effects and is characterized by compulsive use despite harm. Analgesic Tolerance – The need to increase the dose of opioid to achieve the same level of analgesia. Physical Dependence – A physiologic state of neuroadaptation which is characterized by the emergence of a withdrawal syndrome if drug use is stopped or decreased abruptly, or if an antagonist is administered. Pseudoaddiction – Pattern of drug-seeking behavior of pain patients who are receiving inadequate pain medication. Behavior is mistaken for addiction. Guidelines for the management and treatment of Pain WHO - global initiative on pain management (1986) Texas State Board of Medical Examiners (1993) Federation of State Boards (1998) JCAHO (1999) Governmental guidelines (AHCPR) American Pain Society and many more!!!!!! Texas State Board of Medical Examiners’ Position “Quality medical practice dictates that those citizens of TX who suffer pain and other distressing symptoms should be adequately relieved so that their quality of life is as optimum as can be.” “The TSBME recognizes that opioids and other Scheduled Controlled substances, are indispensable for the treatment of pain…” “It is the position of the board that these drugs be prescribed for the treatment of these symptoms in appropriate and adequate doses…” Texas State Board of Medical Examiners’ Position “The Board recognizes that pain, and many other symptoms are subjective complaints and appropriateness and adequacy of drug and dose will vary from individual to individual.” “The standard will be determined largely by treatment outcome…” Physicians should be diligent in preventing (controlled substances) from being diverted from legitimate to illegitimate use. Standards used by Board when evaluating use of Controlled substances: DOCUMENTATION-Medical records should include: – medical history and physical – diagnostic, therapeutic and laboratory results – evaluations and consultations – treatment objectives – discussion of risks and benefits – treatments – medication (date, type, dosage, quantity) – instructions and agreements – periodic review Joint Commission Standards on Pain Management Patient’s have a right to appropriate assessment and management of pain Pain needs to be assessed, documented and followed for appropriate interventions Policies and procedures should support the appropriate use of pain medications Patients and their families should be educated on pain management Discharge planning should include symptom management Governmental Guidelines www.guidelines.gov 1995 - “Clinical practice guidelines for chronic non-malignant pain syndrome” 1998 - “The management of persistent pain in older persons” 1999 - “Procedure guideline for bone treatment pain” 2000 - “Control of pain in patients with cancer. A national clinical guideline” 2002 - “Clinical practice guideline for the diagnosis, treatment and management of reflex sympathetic dystrophy/complex regional pain syndrome” Current Legal Climate Undertreatment of Pain Landmark case in California with a family suing the doctor for inadequate pain control in their dying, 85 year old father during the last week of his life. Jury trial awarded family 1.5 million claiming the physicians lack of attention to pain was “reckless negligence” and constituted elder abuse. Tips for Physicians to protect themselves from charges of Undertreatment of pain: Review your practice against JCAHO standards Improve knowledge in pain assessment and treatment Utilize local consultation resources Improve knowledge and skills in assessing substance abuse; utilize local resources for substance abuse referrals and treatment TYPES OF PAIN Pathophysiologic categorization NOCICEPTIVE – SOMATIC Stimulation of the somatic nervous system skin, soft tissue, muscle, bone easily localized – VISCERAL stimulation of the autonomic nervous system GI and GU tracts, cardiac, lung difficult to describe and localize NEUROPATHIC – PERIPHERAL PROCESSES (neuroma) – CNS PROCESSES (phantom pain) – COMPLEX REGIONAL PAIN Classification of Pain Based on clinical course Acute pain Chronic pain (non-cancer) Cancer pain Post-surgical pain Assessment of Pain “ABCDE” Mnemonic Ask about pain regularly; Assess pain systematically Believe the patient and family in their reports of pain and what relieves it Choose pain control options appropriate for the patient, family and setting Deliver interventions in a timely, logical and coordinated fashion Empower patients and their families; Enable them to control their course to the greatest AHCPR 1994 extent possible Describing Pain: “PQRST” Mnemonic Provoking or Palliative factors Quality of pain Radiation Severity Temporal Goals in the treatment of pain Improve quality of life Encourage mobility Reduce hospitalizations and ER admissions Improve job performance Impact function in a family unit Prevent depression/suicide Step 3, Severe Pain Morphine Hydromorphone Methadone Fentanyl Oxycodone + Nonopioid analgesics + Adjuvants WHO 3-STEP LADDER Step 2, Moderate Pain Combination opioids Tramadol + Adjuvants Step 1, Mild Pain Aspirin Acetaminophen Nonsteroidal anti-inflammatory drugs + Adjuvants Utilization of Opioids: Chronic Pain Dose around the clock - achieve blood levels in the therapeutic range and avoid blood levels falling below pain threshold Rescue dosing - 10% of total 24 hour dose Dose titration: – mild pain: increase dose by 10% – moderate pain: increase dose by 25-50% – severe pain: increase dose by 100% Routes of Administration Oral - preferred Buccal/sublingual Rectal Transdermal Subcutaneous Intravenous Intramuscular - CONTRAINDICATED Intrathecal Equianalgesic Conversion Table ANALGESIC ORAL DOSE PARENTERAL DURATION DOSE OF ACTION (HOURS) HALF-LIFE (HOURS) ORAL: PO PARENTERAL MORPHINE RATIO :ANALGESIC RATIO Morphine 30mg 10mg 4-6hr 2-4hr 3:1 Oxycodone 20mg 3-5hr 4-5hr Hydromorphone 7.5mg 1.5mg 3-4hr 2-3hr 5:1 4:1 Methadone 20mg 15-50h 2:1 3:1 Codeine 200mg 130mg 4-6hr 3hr 1:7 Hydrocodone 30mg 3-6 hr 3-4hr Meperidine 300mg 75mg 2-4hr 10mg 4-6hr 2-3hr 1:1 1.5:1 1.5:1 1:1 4:1 1:10 Variables in Considering Equianalgesic Doses Pain intensity Prior opioid exposure Incomplete cross tolerance Age of Patient Route of administration Level of Consciousness Preexisting conditions Common Side Effects and treatments Constipation - All patients on opioids need a regular bowel program. Nausea - quickly develop tolerance to this Pruritus - may need to switch opioids Sedation - if tolerance doesn’t occur can use stimulants Respiratory depression - most feared yet rare side effect if proper dosing followed Fear of Respiratory Depression from Opioid Use Patients develop tolerance to the respiratory depressant effects early in course of therapy Patients with COPD have been shown to experience improvement in exercise tolerance and decreased SOB Terminally ill patients required 1.5-2.5 times their regular dose of analgesia to control breathlessness; without effect on O2 saturation or respiratory rate Annals Internal Medicine 119: 906, 1993 Fentanyl Transdermal System Medication is absorbed into the subcutaneous tissue; then absorbed into systemic circulation via capillaries May take 18-24 hours before effect of medication therefore not idea for acute pain management Continue previous medicine for 18-24hr after placing the patch Use short-acting opioid for rescue dosing Adjust dose no sooner than every 6 days Once removing patch the effect may persist for up to 24 hours Duragesic: Oral Morphine Equianalgesic Table Morphine dose in 24hr Duragesic Patch Strenth 90mg (range 45-134mg) 25ug/hr 180 (range 135-224mg) 50ug/hr 270 (range 225-314mg) 75ug/hr 360 (range 315-404mg) 100ug/hr For each additional 90mg (range 45-134mg) Add 25ug/hr GOOD RULE OF THUMB: 2 X DURAGESIC DOSE = 24 HOUR Steps in Changing Opioids Calculate 24 hour dose of current opioids Use equianalgesic table - convert dose of current drugs to equivalent new drug Adjust the dose of new drug to accommodate patient variability and incomplete cross tolerance Determine dosing intervals according to duration of action of new opioid Calculate rescue dose Example: Mr. Kaye is receiving 8mg Dilaudid po q 3h, and his physician would like to change the patient to a sustained release morphine product for patient convenience. Calculate the 24 hour dose of Dilaudid – 8mg x 8 = 64mg Dilaudid Using the morphine:Dilaudid ratio figure the 24 hour equianalgesic dose morphine – Morphine: Dilaudid (4:1) – Multiply 64 by 4 = 256mg morphine equivalent Divide the 24 hour dose by 12 for the long-acting morphine dose – 256 divided by 2 = 128 or rounded up to MS Contin 130mg q 12hour On the same patient, figure what the rescue dose of short-acting morphine would be? Figure the total 24 hour dose of routine medication being given – 260mg morphine per day 10% of that can be given every 1-2 hours as needed for breakthrough pain – 10% of 260 = 26mg – can give morphine immediate release tablets (30mg) q 1-2 h or morphine liquid (20mg/ml) 1.25 ml q 1-2 hour On the same patient, if he were to stop swallowing what could be done? Switch to IV therapy – Figure the total dose of morphine given (260mg) – Use the equianalgesic chart to figure oral:parenteral ratio (3:1) – Divide 260mg by 3 = 87mg IV morphine/day – Decide the route (subcutaneous or IV) – Divide 87mg/24hour = 3.6mg/hour – Have boluses of 25-50% total hourly dose available q 15-30mins (1-2mg) Use MS Contin rectally at the same dose and give the rescue dose as a sublingual medication Use sublingual medication on a q 4 hour schedule On the same patient, if Mr. Kaye stopped swallowing tablets but had an extended prognosis? Consider switching to Duragesic Patch – Total Morphine dose 260mg – Duragesic patch dose (per table) is 75ug/h – Via 2x rule: 260/2=130 or 125ug/h – Same breakthrough medication is appropriate Stop the previous routine medication 18-24 hours after the patch is placed Bone Pain from Metastasis NSAID Steroids Bisphosphonates Radiopharmaceuticals Radiation Therapy Neuropathic pain Definition: Arising directly from central and peripheral damage by injury, disease or medical treatment. A pathological pain that serves no adaptive purpose. Frequently becomes chronic and may escalate over time Challenging to diagnose and treat Afferent Pain Pathways Termination in THALAMUS with afferent fibers projecting rostrally to the somatosensory CORTEX and LIMBIC SYSTEM Nociceptive signals ascend in the ANTEROLATERAL WHITE MATTER Nociceptors terminate in the DORSAL HORN and synapse in the Rexed Laminae SPINOTHALAMIC TRACTS send transmission rostrally after decussating in spinal cord NOCICEPTORS react to noxious stimuli (heat, chemical, mechanical) A-delta fibers C fibers Mechanism and Mediators of Pain Painful stimuli causes depolarization of A-DELTA (thinly myelinated) and C-FIBER (unmyelinated) Inflammation from chemical messengers released from damaged tissue (AMP, Protein), mast cells (Prostaglandin), macrophages (cytokines) This leads to lowering of activation threshold and ectopic discharges = Peripheral sensitization Neuron itself releases substance P which turns on messengers of immune cells Positive feedback loop Increase input into Dorsal Horn Peripheral Sensitization Lowering of the nociceptor depolarization threshold and increase in ectopic discharges Due to altered expression and distribution of sodium channels at the level of injured nociceptor and Dorsal Root Ganglion Mechanisms of Pain in the Dorsal Horn Depolarized Nociceptors release Glutamate at the terminal end Glutamate normally binds to AMPA receptor causing depolarization of DH cells With peripheral sensitization and increase input, the NMDA receptor becomes exposed and Glutamate binds NMDA and AMPA. (wind-up) This sensitizes central nervous system such that subthreshold input depolarize neurons Central Sensitization Lowering of the threshold of spinal horn neurons, with an increase magnitude and duration of response to stimulation Expansion in size of receptive field Release of tachykinins (substance P and neurokinin A) – These bind to neurokinin receptor and increase intracellular calcium – Increases NMDA receptor up regulation – Increase in Nitrous oxide synthetase Importance of NMDA Receptor The NMDA Receptor is involved in the propagation of neuropathic pain Tolerance is also related to this receptor When the NMDA Receptor is activated, there is Central Sensitization The opioid receptor, mu receptor, is less responsive to opioids NEUROPATHIC PAIN Nerve Blocks Local Anesthetics Surgical Management Decompression Medical Management Membrane stabilizing Agents STEROIDS Drugs that enhance dorsal horn inhibition GABA-B agonists Baclofen ANTIARRHYTHMICS Lidocaine Mexilitine ANTIEPILEPTICS Oxcarbazepine Clonazepam Gabapentin NMDA Receptor Antagonist ANTIEPILEPTICS Carbamazepine Oxcarbazepine Phenytoin Valproate Ketamine Dextromethoraphan Methadone Amantadine ANTIDEPRESSANTS Amitriptyline Desipramine Imipramine Nortriptyline Most commonly used adjunctive treatments Amitryptilline Carbamazepine Gabapentin Corticosteroids Methadone A Mu agonist and noncompetitive NMDA receptor antagonist No neuroactive metabolites Elimination is independent of renal function Less constipating Good oral bioavailability Extremely low cost Conversion to Methadone Daily oral morphine dose equivalents < 100mg Conversion ratio of oral morphine to methadone 3:1 (ie. 3mg morphine:1mg methadone) 101-300mg 5:1 301-600mg 10:1 601-800mg 12:1 801-1000mg 15:1 > 1000mg 20:1 Interesting Case: 65yr old Anesthesiologist with Diabetic Peripheral neuropathy Mr. C. has stocking-glove distribution neuropathy. He had excruciating pain (10/10) while on Norco (10/325mg) 6-8 per day. Neurontin was not well tolerated Elavil was contraindicated due to cardiac history and conduction system disorder Mr. C. was depressed and didn’t think life was worth living with this pain Neuropathic pain due to Diabetes After discussion with patient and family, we initiated a course of Methadone His current dose of Hydrocodone was 60-80mg daily or the equivalent of 6080mg morphine My conversion with Methadone at low dose morphine is 5:1 I started Mr. C on Methadone 5 mg q 8 ATC with 2.5mg q 3 hours prn Methadone for neuropathic pain Patient tolerated Methadone well Within 24 hours his 10/10 pain was rated at 3/10 Within 1 week, his pain was gone (0/10); Precaution using Methadone: Slow accumulation, varied half-life, needs to be adjusted upward slowly (about q 7 days)