F5-I_Edwards_Ralph_final
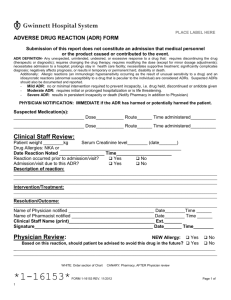
advertisement

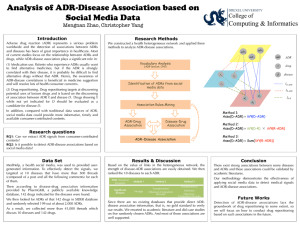
Decision making and communication in the face of uncertainty: the challenge of pharmacovigilance. I Ralph Edwards WHO Foundation Collaborating Centre for International Drug Monitoring A critique of pharmacovigilance Current tools and resources are not used maximally to deliver useful outputs for patient care • Current decision–making processes do not result in public confidence • Current practice underplays several areas of safety importance • Current gaze of regulation is on the control of drugs, not the safety of patients What issues I will cover • Decision making in drug safety • Delays in action (examples) – Outcome research? • Prevention in drug safety – Effectiveness and risk • Comparison between medicines – Risk assessment • Communication and miscommunication – Communication of uncertainty • Patient involvement – Patient, and not drug, safety • An international Programme Decision making in drug safety Items in red are key issues to be tackled Managing a signal ? Public Information 1 Public Information 2 Increasing information and knowledge (also misinformation) A first signal SCARE Media coverage Five broad activities essential to pharmacovigilance: • Suspected ADR signal generation and formation of hypotheses Decisions • Analysis of all issues around the signal, particularly confirmation (or refutation) of hypothesis, estimation of the size of the risk and whether susceptible patients exist Decisions • Consideration of possible effectiveness-to-risk issues in therapy (comparative) – How to do it? – Economics Decisions • Communication of information to health professionals and patients in a useful way. And possible regulatory action. • Consequence evaluation. Decisions Do we really use our tools? • Studies tell us about populations and not individuals – Most ADRs are rare (< 1/1000) • Large numbers of patients and controls needed • Case reports can tell us a huge amount about what concerns individual doctors/h.p’s/consumers – We could get much more information on what happens to people, medication error, interactions, patients at risk, how to diagnose ADRs, etc. Frequently repeated myths?: • Case reports – Cannot prove causality – Under-reporting is a big problem – Bias is unavoidable • Epidemiological studies – Prove/disprove causality – Only, should be used for regulatory action and information • Databases – What actually happens (effectiveness and risk)? Delays in action (examples) Consequences - Outcomes research needed Example of a decision problem to be solved [1] ... Cisapride - heart rhythm disorders • 1986: double blind study “cisapride produced tachycardia” • 1992 WHO Signal published in Br Med J on serious arrhythmia letters to Br Med J “no epidemiological support” • 1995 case report published, Lancet “QT prolongation and tachycardia” Dear Doctor letter in USA by manufacturer Example of a decision problem to be solved [2] ... • Piroxicam is the most GI toxic of the NSAIDS in several comparative studies – GI toxicity is a major cause of morbidity • Why is it still available? Example of a decision problem to be solved ?? [3] ... • . At the WHO Meeting,Tunis ( Oct, 2000) the Netherlands Monitoring Centre (Lareb) presented the first signal of cardiovascular disorders relating to rofecoxib, for 8 cardiovascular ADRs (of 62 total reports) with 4 fatalities and which occurred early in treatment. (ROR 12.4 (4.5-35), all drugs: 12.0 (3.8-38.2), NSAIDS Consequences • Newspaper article showing extensive scars on the legs of a young woman following venous thrombectomy • Cause for thromboses given as Diane (cyprotereone acetate : ethinyloestradiol) used for acne Consequences • Patient given wide media coverage • Many patients reported to stop taking Diane • Dermatologist rings National Monitoring Centre – ' Many patients taking Diane are also taking Roaccutane. The logic is to provide both contraception and an additional (anti-androgenic) therapy for their acne'. – 'They are at risk for malformed fetus, if they stop contraception' Consequences • Since all prescriptions of Roaccutane must be prescribed by a dermatologist – And patients must give informed consent • Notify all dermatologists • Call in patients on Roaccutane • Advise about contraception and relative risks of Diane • Also make a media announcement on the above Consequences • No unwanted pregnancies reported! • By luck and rapid, complete and appropriate action a disaster was anticipated and avoided • But this was a special case! Consequences • Letter: – The 'Dear Doctor' letter on cerivastatin, interaction and rhabdomyolysis • ....do not co-prescribe with .... • Intention: – To change prescribing, to reduce rhabdomyolysis particularly linked with interaction with gemfibrosil • Result: – After 3 letters and 2 years only a 2% reduction in coprescription, BUT more reports sent to the authority • Lesson: – Check response; modify approach; give guidance as well as warning This is only part of the story! • • • • • • Vigilance Signal Hypothesis Analysis Probability Frequency • • • • • • • Epidemiology Signal Hypothesis Analysis Confirmation Probability Frequency Prevention in drug safety Effectiveness and risk Need for comparison between medicines Risk assessment The true balanced concepts • Efficacy (hard data) • Effectiveness • Benefit feels) NO! • Hazard • Risk Yes! (what the patient • Harm (soft data) Size and severity of the ADR problem Meta-analysis • 39 prospective studies from US hospitals • Overall incidence of serious ADRs = 6.7% • Overall incidence of fatal ADRs = 0.32% (106 000 individuals) • 4th - 6th leading cause of death Lazarou et al JAMA 1998;279: 1200 - 1205 6.7% of hospital patients have serious adverse drug reactions (medication error excluded) Lazarou J. Pomeranz BH, Corey PN. JAMA 1998;279:1200-5 16.2% of hospital admissions are drug-related Therapeutic failure 54.8% Adverse reactions 32.9% Overdose 12.3% Avoidable 49.3% Nelson KM, Talbert RL. Pharmacotherapy 1996;16:701-7 Pirmohamed M JS, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ 2004;329(7456):15-19. • ….identifies the main drug culprits in a large hospital based study. They are old drug groups (low dose aspirin, diuretics, warfarin, and non-steroidal anti-inflammatory drugs other than aspirin: the most common reaction being gastrointestinal bleeding) on which we have much information…… Proposed risk assessment Eliminating risk (not possible!) • Risk specification • Risk plan – Milestones • Risk minimisation • Start early and continue • High potency, high risk products – Tripartite involvement: • Prescriber • Dispenser • Patient How do the new compare with the old? Some new challenges • Medication error • ADR diagnosis • Therapy adherence – ‘Intelligent non-compliance’ • Lack of effect – Sub-standard and counterfeit drugs • Interactions • Herbals • Public health programmes – incl. Vaccines • Comparisons of therapies – UK NICE – Data mining Communication and miscommunication Communication of uncertainty Effectiveness/risk communication • • • • The correct message To the right audience By the right medium Consequences – – – – Message received? Message understood? Followed up? Acted upon appropriately? Warning and communication of risk -now • SPC – Use of PSUR – Legal v. Communication – Which section of SPC • Contra indication, warning – When changed? – Design ? • ‘Dear Health Professional‘ communication – Web – Design – Repeated • Media • Bulletins Warning and communication of risk • Players may have competing interests in communication even if public health is a common aim • Media – Dramatic news a priority – Internet • No control • Wide range of issues possible – Difficult to predict response – Prepare for rapid and intense communication Warning and communication of risk – the future • Outcomes – Follow up? • Questionnaires – General – Specific – Need more information on outcomes – Better public education – Less paternalism • Better view of us! • Openness – Constructive law & media interaction The Erice Declaration on Communicating Drug Safety Information • The following declaration was drawn up at the International Conference on Developing Effective Communications in Pharmacovigilance, Erice, Sicily, 24-27 September 1997. It was attended by health professionals, researchers, academics, media writers, representatives of the pharmaceutical industry, drug regulators, patients, lawyers, consumers and international health organisations. The Erice Declaration • 1. Drug safety information must serve the health of the public. Such information should be ethically and effectively communicated in terms of both content and method. Facts, hypotheses and conclusions should be distinguished, uncertainty acknowledged, and information provided in ways that meet both general and individual needs. The Erice Declaration • 2. Education in the appropriate use of drugs, including interpretation of safety information, is essential for the public at large, as well as for patients and health-care providers. Such education requires special commitment and resources. Drug information directed to the public in whatever form should be balanced with respect to risks and benefits. The Erice Declaration • 3. All the evidence needed to assess and understand risks and benefits must be openly available. Constraints, on communication participants, which hinder their ability to meet this goal must be recognised and overcome. Managing a signal: the future Public Information 2 Public Information 1 A first signal Pre-marketing risk management Increasing information and knowledge (also misinformation) Media coverage Patient involvement Patient, and not drug, safety Patient involvement • Patients need more general information about drugs and their effectiveness and risk • VERY IMPORTANT – We need much more information about what risks patients are prepared to take for what benefit to them. Until we know this we will continue to ‘second-guess’ about what is acceptable or not Measuring true effectiveness and risk • Needs knowledge finding in patient care databases – E.g Data mining in IMS Health database of 2 million patients • Can show comparative effectiveness and risk – Data quality Fluoxetine Amitrityline (One Year) Suicidality An international Programme WHO Programme for International Drug Monitoring plus Global Alliance for Patient Safety Functions • Collection and processing of international ADR data – > 3.5 million concerns about drugs from HPs and patients since 1968 • Signal detection and analysis – Available free • Tools – WHO DD and terminologies are world standards • Research – Data mining of patient care databases • Information and feedback • Education and support • Harmonisation Conclusions • Think less about drug safety: more about patient safety • Think less about regulating and automating data input: more about useful information output • Think more about impact and consequences of decisions and non-decisions • Think more about global cooperation: not competition