Indicator Organisms

Water Microbiology/Microbial
Contaminants
Gwy-Am Shin
Office: Suite 2335, 4225 Roosevelt
Phone: 206-543-9026
Email: gwyam@u.washington.edu
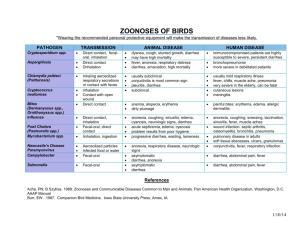
Microbiological Contaminants
• Most benign, “normal”
• Some are frank pathogens
• Microbial pathogens usually are not “normal flora” of humans; Oppurtunisitic pathogens
– Some are “normal flora” of animals:
• Salmonella enteriditis and Campylobacter jejuni in poultry
– “Normal flora” for local populations may be pathogenic for visitors and transient populations:
• “Traveller’s diarrhea” due to local strains of E. coli
– Some “normal flora” are pathogenic for sensitive populations, such as immunocompromised persons
Occurrence of Enteric Microbial Pathogens in
Humans and Pathogen Shedding
• Enteric (gastrointestinal) illnesses are second only to respiratory illnesses in the population
• Most people get 1 enteric illness per year:
– Annual illness rates are even higher in infants, children, the elderly, child caregivers, health professionals, the poor, male homosexuals and other high risk groups
• Not all enteric infections produce illness (asymptomatic or sub-clinical infections)
– So, rates of infection are even higher (by perhaps 2 to 100 times)
• People (and animals) with enteric infections fecally excrete high concentrations of pathogens for days, weeks, months or longer.
• Pathogen concentrations can be >10 6 to >10 9 per gram of feces.
• Community pathogen shedding is often 1-10% at any time.
Transmission of enteric pathogens
Incidence and concentration of enteric pathogens in feces (USA)
Pathogen
Enteric virus
Hepatitis A
Rotavirus
Salmonella
Giardia
Cryptosporidium
Incidence (%) Concentration(/gram)
10-40 10 3 -10 8
0.1
10-29
0.5
3.8
18-54
0.6-20
27-50
10 8
10 10 -10 12
10 4 -10 10
10 6
10 6
10 6 -10 7
10 6 -10 7
Viruses: smallest (0.020.3 µm diameter); simplest: nucleic acid + protein coat (+ lipoprotein envelope)
Bacteria: 0.52.0 µm diameter; prokaryotes; cellular; simple internal organization; binary fission.
Protozoa: most >2 µm- 2 mm; eucaryotic; uni-cellular; non-photosynthetic; flexible cell membrane; no cell wall; wide range of sizes and shapes; hardy cysts
Groups: flagellates, amoebae, ciliates, sporozoans
(complex life cycle) and microsporidia.
, rigid cell wall, most eukaryotic Algae: wide range of sizes and shapes; photosynthetic.
Helminths (Worms): multicellular animals; some are parasites; eggs are small enough (25150 µm) to pose health risks from human and animal wastes in water.
THE MICROBIAL WORLD:
SIZES OF MICROBES
Parasites are visible by light microscopy
Viruses
• Smallest (0.02 – 0.3
µ m)
• Simplest
– Nucleic acids (DNA or
RNA)
– Protein capsid
Human enteric viruses
Bacteria
• Size: 0.5 –2.0 µ m
• Simple internal organization
• Envelope: cytoplasmic membrane, cell wall, and capsule
• Appendages: flagella and/or pili
• Spores: environmentally resistant form
Human pathogenic bacteria
Human pathogenic bacteria
Procaryotic Cell (left) and Eucaryotic Cell (right)
Protozoa
• Size: 2 – 2000 µ m
• Complex internal organization (nucleus, mitochondria, etc)
• Very complex life cycle
(inside and outside of their hosts)
• Flagellates, amoeba, ciliates, and sporozoans
• (Oo)cysts: environmentally resistant form
Human protozoan parasites
• Photosynthetic
• Rigid cell wall
• Wide range of sizes and shapes
– 2 micrometers and larger
Algae
Nostoc
Anabaena and Aphanocapsa
Helminths (Worms)
• Multicellular animals
• Some are human and/or animal parasites
• Eggs are small enough to pose environmental health problems from human and animal excreta in water, food, soil, etc.
• Several major groups:
– Nematodes (roundworms): ex. Ascaris
– Trematodes (flukes; flatworms): ex. Schistosomes
– Cestodes (tapeworms): pork and beef tapeworms
Helminths
• Multicellualr animals
• Size: up to 30 cm
• Highly differentiated structures
• Very complex life cycle
(inside and outside of their hosts)
• Nematodes,
Trematodes, and
Cestodes
• Eggs: environmentally resistant form
Human helminth parasites
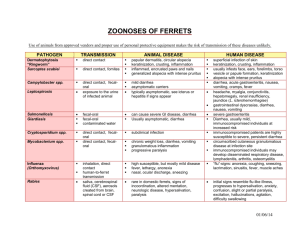
Bacteria
Shigella spp.
• Elongated and straight rods
• Size: 0.5-1 µm
• Four species: dysenteriae, flexneri , sonnei , and boydii
• Watery or bloody diarrhea, abdominal pain, fever, and malaise
• fatality may be as high as
10-15% with some strains
Shigella spp.: Epidemiology
• Involved in 44 drinking water outbreaks with 9,196 cases and 34 recreational water outbreaks with 2,329 cases in USA (1971-2000)
• Incidence
– 14,000 (lab-confirmed) and 448,240 (estimated) cases in USA
– 164.7 million (estimated) case (163.2 in developing countries and 1.5 in developed countries) and 1.1 million death worldwide
– 580,000 cases in travelers
• Reservoirs: humans and primates
• Infectious dose: ~ 10 cells
• Incubation period: typically 1-3 days
• Duration of illness: 2-7 days
• Mode of transmission: Direct (person-to-person) and indirect
(fomites, water, and food)
Escherichia coli O157: H7
• Elongated and straight rods
• Size: 0.5-1 µm
• ~8,000 serotypes
• Acute bloody diarrhea and abdominal cramps with little or no fever
• 3-5% fatality.
Escherichia coli O157: H7 :
Epidemiology
• Involved in 11 drinking water outbreaks with 529 cases and 15 recreational water outbreaks with 387 cases in USA (1971-2000)
• Incidence
– 730,000 (estimated) cases (USA)
– 210 million cases and 300,000 deaths worldwide
– Many different serotypes: enterotoxigenic (ETEC); enteropathogenic
(EPEC); enteroinvasive (EIEC); and enteroaggregative (EAgg EC)
– All pathogenic E. coli : 1.5 billion (estimated) case and 3 million death worldwide
• Reservoirs: humans and animals ( cattle, goats, sheep, deer, ….)
• Infectious dose: ~ 100 cells
• Incubation period: typically 1-3 days
• Duration of illness: 2-12 days
• Mode of transmission: Direct (person-to-person) and indirect
(fomites, water, and food)
Salmonella spp.
• Elongated and straight rods
• >2,000 serotypes
• Diarrhea, fever, headache, constipation, malaise, chills, and myalgia
• 12% - 30% mortality
Salmonella spp.
: Epidemiology
• Involved in 12 drinking water outbreaks with 2,370 cases in USA (1971-1992)
• Incidence
– An estimated1.4 million cases with 500 death in the United
States
– An estimated 21 million cases of typhoid fever and 200,000 deaths occur worldwide.
• Reservoirs: humans and animals (cattle, chicken, turkey…)
• Infectious dose: ~100 cells
• Incubation period: typically 1-3 days
• Duration of illness: 2-7 days
• Mode of transmission: Direct (person-to-person) and indirect (fomites, water, and food)
Vibrio cholerae
• Straight or curved rods
• Motile with flagella
• 0.5-0.8 µ m in width and
1.4-2.6 µ m in length
• Serogroup O1 or O139
• Profuse watery diarrhea, vomiting, circulatory collapse and shock.
• 40 - 60 % of typical cases are fatal if untreated
Vibrio spp.
: Epidemiology
• Involved in 2 drinking water outbreaks with 28 cases in the USA
(1971-2000)
• Incidence
– 0-5 cases per year in the United States.
– A major cause of epidemic diarrhea throughout the developing world.
– Ongoing global pandemic in Asia, Africa and Latin America for the last four decades.
• Reservoirs: humans, environmental reservoirs - waters may be associated with copepods or other zooplankton
• Infectious dose: ~100 cells
• Incubation period: a few hours to 5 days; usually 2-3 days
• Duration of illness: several days
• Mode of transmission: Indirect (water and food)
Campylobacter spp.
• Curved rod
• Size: 1.5-3 microns
• C. jejuni and C. coli
• fever, nausea, abdominal cramps,
(seldom) vomiting, and bloody diarrhea
Campylobacter spp.
: Epidemiology
• Involved in 16 drinking water outbreaks with 5473 cases in the USA (1971-2000)
• Incidence
– An estimated 2.4 million persons are affected each year.
• Reservoirs: humans and animals (cattle, chicken, birds, …)
• Infectious dose: ~100 cells
• Incubation period: 3-5 days
• Duration of illness: 2-10 days
• Mode of transmission: Direct (animal contact) and indirect
(food and water)
Other Important Bacterial
Pathogens
• Fecal origin
– Aeromonas spp.
– Plesomonas spp.
– Yersinia spp.
• Environmental origin
– Legionella spp. (esp. L. pneumophila )
– Pseudomonas spp. (esp. P. aeruginosa )
– Mycobacterium Avium Complex (MAC)
Nuisance Bacteria
• Acintomycetes/Streptomycetes
– Thin filamentous, gram postive rods
– Taste and odor
• Iron Bacteria
– E.g. Leptothrix, Thiobacillus, Clonothrix, Sphaerotilus, Caulobacter,
Hyphomicrobium
– Main corrosion
– Increase oxidant demand
• Sulfur Bacteria
– E.g. Desulfovibrio, Thiothrix, Chlorobium, Chromatium, Thiobacillus
– Formation of tubercles; pipe corrosion; increase oxidant demand
– Reduce Sulfur compounds to H
2
Sa
• Nitrifying bacteria
– E.g. Nitrosomonas, Nitrobacter, Nitrospira, Nitrococcus
– Increased oxygen demand (Nitrite);
Protozoan Pathogens
Waterborne Outbreaks in the
United States, 1989-1994
Etiologic Agent No. Outbreaks
Acute GI (unknown)
Cryptosporidium parvum
44
8
Giardia lamblia 16
No. Cases
16,264
406,822
1,205
Hepatitis A virus
Norwalk-like viruses
E. coli O157:H7
Cyclospora cayatenensis
Shigella spp.
Salmonella sp.
1
Vibrio cholerae (non-01) 1
Chemicals:
Pb, NO
3
, F and Cu 13
1
1
4
1
7
81
900
243
21
570
625
11
394
TOTAL 87 427,256
Protozoa
• Size
– Usually 10-50 µm
• smallest: 1-10 µm, largest: 150 µm ( Balantidium coli )
• Many organells
– Nucleus (or nuclei)
– Cytosome (cell mouth), food vacuoles, contractile vacuoles (osmoregulation), Golgi apparatus, mitochondria, lysosomes,…
– Locomotive structures: pseudopodia, flagella, cilia
• Cell cycle and reproduction
– Asexual (binary fission) and sexual (various life stages)
Prokaryotic Cell (left) and Eukaryotic Cell (right)
Enteric Protozoans: Taxonomy
Protozoans (single-celled):
• Sarcodina: Amoebas: ex.: Entamoeba histolytica
• Mastigophora: Flagellates: ex.: Giardia lamblia
• Sporozoa: Coccidians: Cryptosporidium parvum
• Ciliophora: Ciliates: ex.: Balantidium coli
• Microsporidia: ex.: Enterocytozoon beinusi
Entamoeba histolytica
• Ameba
• Cyst
– 10-20 μm
– 4 nuclei
– chromatoidal bars
• Trophozoite
– 12-50 μm
– 1 nucleus
– actively mobile
• Mild GI symptoms (abdominal pain, cramps, colitis and diarrhea), bloody diarrhea
(amoebic dysentery)
Entamoeba histolytica: Epidemiology
• Involved in 1 drinking water outbreaks with 4 cases and 40 recreational water outbreaks with 11,707 cases in USA (1971-2000)
• Incidence
– 4 % prevalence in USA
– 50 % prevalence with 100,000 deaths per year worldwide
• Reservoir: human is the only host
• Infectious dose: unknown; however, theoretically, the ingestion of one viable cyst can cause infection
• Incubation period: 1-4 weeks
• Transmission: Direct transmission (sexually transmission), fecal-oral route, waterborne, foodborne
• High risk groups: travelers, recent immigrants, male homosexuals, institutioned populations
Giardia lamblia
•
Flagellate
•
Cyst
– 8-14 μm
– 2-4 nuclei
– thick oocyst wall (0.3 μm)
• Trophozoite
– Heart-shaped, symmetric
– 10-18 μm long, 6-8 μm wide
– 2 nuclei
– 8 flagella
• abdominal cramps, nausea, vomiting, anorexia, low-grade fever, flu-like headache, general malaise, weakness, weight loss, distension, and profuse, greasy, bulky and foul-smelling diarrhea
Giardia lamblia
:
Epidemiology
• Involved in 126 drinking water outbreaks with 28,426 cases and 16 recreational water outbreaks with 684 cases in USA (1971-2000)
• 500,000 estimated cases (200 millions?) worldwide
• Reservoir: Human and animals (dogs, beaver, muskrat, elk, deer, voles, mice, horses, sheep, …)
• Infectious dose: ~10 cysts
• Incubation period: 1-14 days
• Duration of illness: 1-3 weeks
• Transmission: Fomites, waterborne, foodborne
• High risk groups: children (in day-care centers), immunosuppressed people, and institutioned populations
Cryptosporidium parvum
• Coccidia
• Oocyst
– 4 - 6 m
– 4 sporozoites
– Thick oocyst wall
• Sporozoite
– No locomotive structure
• Immunocompetent people: similar to giardiasis
• Immunocompromised people: lifethreating
• Fluid loss: 2-6liter/day (17 liters/day)
• Extra-intestinal infection: respiratory cryptosporidiosis
(intestitial pneumonia)
Cryptosporidium parvum
:
Epidemiology
• Involved in 15 drinking water outbreaks with 421,473 cases and 40 recreational water outbreaks with 11,707 cases in USA(1971-2000)
• Incidence
– 1 – 3 % prevalence in USA
– 5 % (Asia) and 10 % (Africa) prevalence
• Reservoir: Human and animals (calves, lambs, goats,horses, pigs, deer, squirrel, beaver, muskrat,woodchuck,rabbit, dogs, fox, cat, skunk, raccon, bear, …)
• Infectious dose: < 10 cysts
• Incubation period: 7 days
• Duration of illness: 1-4 weeks
• Transmission: Fomites, waterborne, foodborne
• High risk groups: children, immunosuppressed people, institutioned populations
Emerging Protozoan Parasites
• Toxoplasma gondii
• Microsporidia spp.
Toxoplasma gondii (oocysts)
• Apicomplexa (Coccidia)
• Oocyst
– Two phases
•
A: unsporulated
•
B: sporulated
– 10 – 13 m
– two sporocysts
– four sporozoites
– distinctive cell walls
• two or three layers
• scatter UV
• highly persistent in the environment
– soil (months)
– moist conditions
(years)
Toxoplasma gondii (other infectious forms)
• Tachyzoite
– Crescent-shaped
– 2X6
m
– Rapidly multiflying
– Transmitted through placenta
• Bradyzoite
– Slowly multiplying
– Tissues in intermediate hosts
• Reproduction
– Both asexual (intermediate hosts) and sexual (definitive hosts: cats)
Transmission of Toxoplasma gondii
Toxoplasma gondii
:
Epidemiology
•
Worldwide
– 22.5 % prevalence (general population) in USA between 1988-1994
– Half billion people in the world
• Unusually high prevalence in France (65-85%): raw or undercooked meat
• High prevalence in Central America: large number of stray cats
• Symptoms
– Immunocompetent people: mostly asymptomatic, some flu-like symptoms (swollen lymph glands, muscle aches and pains)
– Immunocompromised people: life-threating
• central nerve system disease (encephalitis)
• blindness, myocarditis, pneumonia
– Congenital infected children
• impaired vision and mental retardation
• Reservoir: Definitive hosts are cats; intermediate hosts are sheep, goats, rodents, swine, cattle, chicken, and birds
• Infectious dose: Not known
•
Incubation period: 10-23 days
•
Transmission: Indirect (water and food) and transplacental
• High risk groups: infants born to infected mothers, immunosuppressed people
Microsporidia spp.
• New Phylum
– 143 genera, >1200 species
– 14 identified human pathogens
• Produce very resistant spores
– Usuaually small (1-4
m)
• A unique organalle (polar tubule)
– Coiled inside the spores
– Inject infective spore contents into the host cells
Life cycle of Microsporidia spp.
Microsporidia spp.
:
Epidemiology
• Worldwide
– Both developed and developing countries
• Symptoms:
– Immunocompetent people: asymptomatic or self-limiting diarrhea
– Immunocompromised people:
• Chronic diarrhea
• Disseminated diseases (keraconjunctivitis, bronchitis, pnuemonia, hepatitis,
…)
• Reservoirs: human and animals (rabbits, mice, dogs, pigs, cats, cattle, wild birds (parrots), insects?)
• Infectious dose: Not known
• Incubation period: Not known
• Transmission: uncertain
– Airborne transmission?
– Waterborne transmission??
– Transplacental transmission? ( Encephalitozoon spp.)
Other Important Protozoa
• Trypanosomes- Sleeping Sickness
– African (Tsetse flies)
– American (kissing bugs) “Chaga’s”