Parkinson's Plus Syndromes: MSA, PSP, LBD, CBD Overview
advertisement
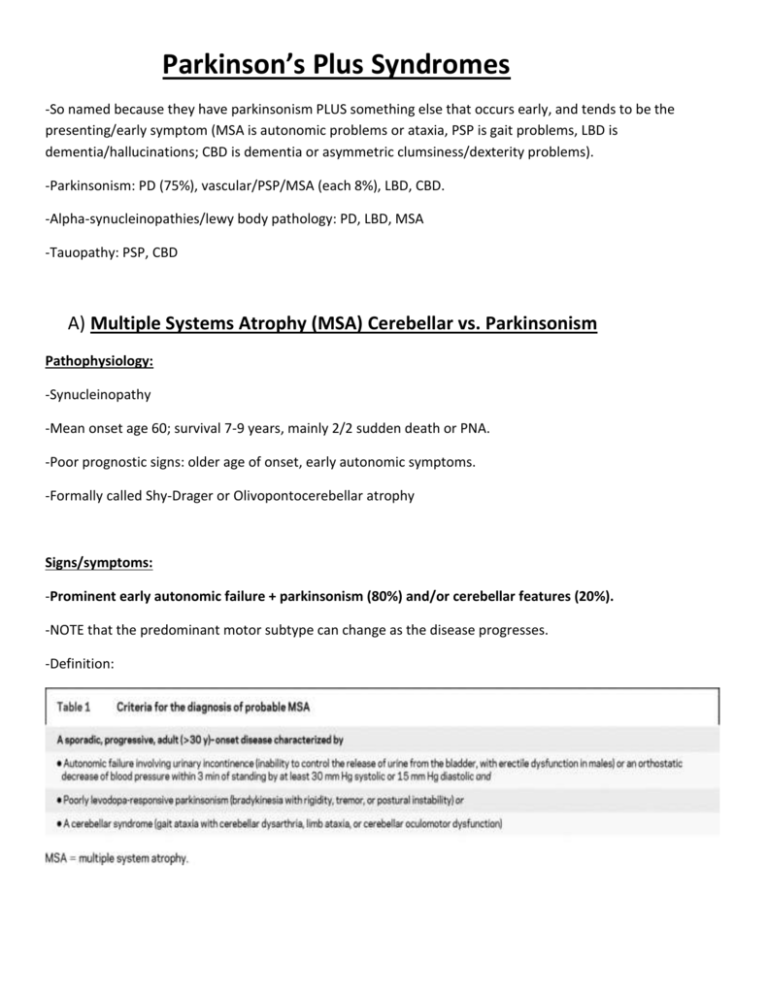
Parkinson’s Plus Syndromes -So named because they have parkinsonism PLUS something else that occurs early, and tends to be the presenting/early symptom (MSA is autonomic problems or ataxia, PSP is gait problems, LBD is dementia/hallucinations; CBD is dementia or asymmetric clumsiness/dexterity problems). -Parkinsonism: PD (75%), vascular/PSP/MSA (each 8%), LBD, CBD. -Alpha-synucleinopathies/lewy body pathology: PD, LBD, MSA -Tauopathy: PSP, CBD A) Multiple Systems Atrophy (MSA) Cerebellar vs. Parkinsonism Pathophysiology: -Synucleinopathy -Mean onset age 60; survival 7-9 years, mainly 2/2 sudden death or PNA. -Poor prognostic signs: older age of onset, early autonomic symptoms. -Formally called Shy-Drager or Olivopontocerebellar atrophy Signs/symptoms: -Prominent early autonomic failure + parkinsonism (80%) and/or cerebellar features (20%). -NOTE that the predominant motor subtype can change as the disease progresses. -Definition: -Autonomic features: Urinary retention OR incontinence, orthostasis, erectile dysfunction, OSA, stridor (SCARY sign, could suggest impending respiratory failure), constipation, trouble with sweating, gastroparesis, early satiety. -Supportive features: Early instability (within 5 years), rapid progression, abnormal postures (leaning laterally or frontally, anterocollus), bulbar dysfunction (dysphagia, high pitched dysarthria and dysphonia), respiratory dysfunction (sighing/stridor), pseudobulbar affect, myoclonic jerky action tremor, Raynaud’s, RBD, OSA, poor response levodopa (1/3 respond to it; many get early dyskinesia), oro-facial dystonia. Can sometimes get executive dysfuntion. -NOT supportive: dementia, family history, rest tremor Dx: -Clinical diagnosis -Sweat test/autonomic testing showing no sweating can be helpful. -Urodynamic studies to document urinary retention. -MRI brain: “hot cross bun” sign on T2 (hyperintensity in pons/midbrain and middle cerebellar peduncle). Also can see strip of hyperintensity along striatum on T2 imaging. -FDG PET: reduced glucose metabolism in putamen, cerebellum, thalamus, brainstem. -Pathology: Glial cytoplasmic inclusions are classic. -DDx: Neuropathy/peripheral cause of autonomic failure (ie, POTS or severe neuropathy, Meige Syndrome, etc) Tx: -Orthostasis: fluids/salt, avoid anti-HTNs, compression stockings, elevate head of bed (wedge pillow), take time getting up, midodrine (7.5mg divided TID, uptitrated to max of 10mg TID daily with last dose no later than 6PM), or fiorinef (0.1mg daily increased by 0.1mg per week until max of 0.5 mg per day, titrated to trace pedal edema) or maybe droxidopa (200-2000mg daily). If get supine HTN, do reverse trenbelenburg, nighttime nitro, clonidine patches, pyridostigmine. -Constipation: Miralax, senna, etc. -Urinary retention: Tamsulosin, ? straight cath, consider urology referral. -CPAP for OSA; trach if stridor can reduce risk of sudden death. -Most patients dead by 10 years after diagnosis -30% respond to sinemet, though start slow and watch for worsening orthostasis. Review article: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2676993/ B) Progressive Supranuclear Palsy (PSP) Pathophysiology: -Tau-opathy -Onset age >40, average around 65. Signs/symptoms: -Early postural instability (freezing, stiff gait, knees extended, pivots WITHOUT en bloc turning, slump into the chair, toe walking, lack of insight) - Vertical gaze palsy (namely downgaze; supranuclear, in that it can be overcome with oculocephalics, though later becomes nuclear late in disease; can ALSO only lose vertical saccades early on). Can present as diplopia. -Axial rigidity -Dysarthria (growling, pallialia, moaning, monotonous, sometimes ataxic)/dysphonia -Dysphagia -Square wave jerks -frontal subcortical dementia (apathy, executive dysfunction) -Lack of any real response to levodopa - Pseudobulbar affect -Astonished/worried facial expression -frontal signs (grasp, perseveration with hand clapping 3 times, head lags behind body) -Cervical dystonia (retrocollis), assymetric limb dystonia, apraxia of eyelid opening -No rest tremor Dx: Imaging: -MRI brain: midbrain atrophy, dilatation of aquaduct with normal pons (on saggital view; called “hummingbird sign”). Measure anterior/posterior distance of pons and midbrain. -FDG PET: hypometabolism in brainstem and midline frontal cortex. Tx: -Symptomatic (PT, opthy eval for prisms if diplopia, SLP). -Consider Gtube if significant aspirations, or significant weight loss. -Poorer prognosis: older age at onset (>63), early dysphagia or cognitive decline. Death is usually from aspiration/pneumonia. C) Lewy Body Dementia: 1) Signs/symptoms: -Dementia starting before or around the same time (ie, within a year or so) as parkinsonism. Classically with early formed visual hallucinations (usually people/children) and fluctuations in attention. -50% have RBD; almost no patients with AD have RBD. -Fluctuations in attention may be mistaken for seizures, symptoms of OSA, result of poor sleep, or medication effects/delerium. -It is likely that PD and LBD are the same alpha- synuclein disease, just on a spectrum: with PD the pathology starts subcortically and spreads cortically (thus early parkinsonism with late dementia), while LBD the pathology starts cortically and spreads subcortically (early dementia with later parkinsonism). 2) Diagnostic criteria: -Probable LBD: Progressive cognitive decline + 2 of the following MAJOR criteria: fluctuating attention/alertness, visual hallucinations, motor parkinsonism. OR Progressive cognitive decline + 1 of the MAJOR criteria + one of the following MINOR criteria: REM sleep behavior disorder, severe neuroleptic sensitivity, or suggestive PET scan. 3) Tx: -Cognitive: Aricept significant improvements lasting at least 12 weeks and reducing caregiver burden. Anecdotally, it can be quite helpful. -Avoid antipsychotics and sedative-hypnotics if possible; if needed, prefer quetiapine or clozapine as less likely to worsen parkinsonism or cause paradoxical confusion. LBD patients are often “more sensitive” to medication side effects. -Parkinsonism: Sinemet can often be effective, but need to balance with risk of worsening cognitive symptoms. Avoid dopamine agonists due to high risk of side effects in this population. 4) Prognosis: -Average survival from time of diagnosis is 8 years. D) Corticobasilar Degeneration: -Tauopathy -Mean age of onset in 60’s (none <45 have been pathologically confirmed) -CLASSIC SYMPTOMS: “Persistent asymmetric neurologic findings” is the classic feature. Also get limb apraxia, UMN signs, painful asymmetric rigidity and atrophy, stimulus-induced myoclonus, primary progressive aphasia, alien hand/limb, visuospatial dysfunction, graphesia/cortical sensory problems, high amplitude action and rest tremor, “holding hands”, insidiously progressive parkinsonism. -90% will have bradykinesia, rigidity, and apraxia in first 3 years. -Dementia is the most common initial symptom; first motor symptom is limb clumsiness/dexterity problems. -Can often have overlap with PSP, FTD. -Diagnostic criteria: 1) All of the following: insidious onset, gradual progression for >1 year, age of onset >50, no response to sinemet AND 2 of the following: 2) Akinetic rigidity syndrome, limb apraxia, or speech and language impairment. AND 2 of the following: 3) Myoclonus, assyemtric dystonia, alien limb phenomenon, cortical sensory loss (graphesia) or dyscalculia, frontal executive dysfunction, or visuospatial defects -MRI brain: Asymmetric volume loss/atrophy is classic; most useful with serial studies. -PET will show assymetric global reduction in metabolism, correlating with body areas most affected. -DAT scan abnormal most of time. Tx: -DOES NOT respond to sinemet (25% response at best), other PD drugs tend to make symptoms worse. -Symptomatic (klonopin for myoclonus/tremor, etc) -Prognosis: Worse if bilateral parkinsonism or frontal lobe syndrome. Death is usually 5-10 years after symptom onset.