Unable to Attend the First Days? - American Association for Thoracic
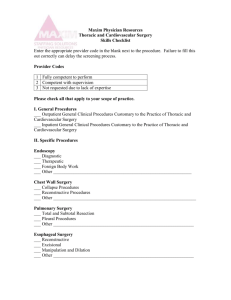
advertisement

Unable to Attend the First Days? Unable to Attend the First Days? (Prior 50+years) Unable to Attend the First Days? (Prior 50+years) Too Bad Unable to Attend the First Days? (Prior 50+years) Too Bad Read the Meeting book Unable to Attend the First Days? (Prior 50+years) Too Bad Read the Meeting book Get here earlier next year In Case You Missed it!!! General Thoracic Surgery New This Year In Case You Missed it!!! General Thoracic Surgery New This Year Brief Review of a Few of my favorite studies In Case You Missed it!!! General Thoracic Surgery New This Year Brief Review of a Few of my favorite studies I got to sit through ENJOY EVERY presentation Multimodality therapy for locally advanced thymomas: a cohort study of prognostic factors from a European multicentric database Dr. GIOVANNI LEUZZI Department of Surgical Oncology Thoracic Surgery Unit “Regina Elena” National Cancer Institute, Rome, Italy Background Locally-advanced Thymomas (LATs): 20-29 % Heterogeneous entity o Different tumor size o Different organ involvements Radical resection not usually feasible (50-78%) ~ 50 % LATs experience recurrence after surgery Higher stage (III-IV) and R+ resection decrease survival Our experience European Society of Thoracic Surgeons (ESTS) thymic database (38 Institutions) Stage I, II and IV excluded 2317 surgically-treated Thymic Tumors (01/1990 – 01/2010) 370 Masaoka-Koga stage III Thymomas (WHO Histology A to B3) Thymic carcinoma and NETT excluded Outcome & Treatment Strategy 1.0 Treatment strategy (n=353) Pts (%) Surgery alone 66(18.7%) IT + Surgery + AT 46(13.0%) IT + Surgery 42(11.9%) Probability of Survival Probability of Survival) .9 Surgery + AT 199(56.4%) .8 .7 .6 .5 .4 .3 p=0.006 .2 Surgery alone IT + Surgery + AT IT + Surgery Surgery + AT .1 0.0 0 IT Group Primary Surgery Group p-value CSS 85.0% 88.3% 0.82 RFS 77.9% 84.0% 0.31 30 60 CSS (months) CSS (months) 90 120 Probability of Survival Outcome & Adjuvant Therapy p=0.0004 AT Group No AT Group p-value CSS 91.1% 81.5% 0.0004 RFS 85.5% 79.3% 0.19 Conclusions Our analysis indicates that Induction Therapy is not associated with a survival advantage. Administration of Adjuvant Therapy and Completeness of Resection represent the most significant outcome predictors. Adjuvant Therapy should be administered whenever possible, especially in those patients with specific pathological features (pT2/3 or tumor size smaller than 5 cm) who may benefit the most from multimodality treatment. My Thoughts Very heterogeneous cohort of patients Induction Therapy in my Practice is reserved for Marginally resectable patients This might be a very significant source of bias The Impact of Adjuvant Chemotherapy in Pulmonary Large Cell Neuroendocrine Carcinoma (LCNC) Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery LCNC Rare tumor (2% to 3% all resected primary lung cancers) Preoperative diagnosis is often impossible Clinical behavior and prognosis similar to SCLC Surgery alone is insufficient to treat LCNC, even in early Stages Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery Author Year N° pts 5-y OS 5-y OS Stage I Recurrence % Garcia-Yuste et al. 2000 22 21 % 33 % 59 % Takey et al. 2003 87 57 % 67 % 40 % Battafarano et al. 2004 45 30 % 33 % 49 % Paci et al. 2004 48 21 % 27 % NA Rossi et al. 2005 83 NA 33 % 65 % Veronesi et al. 2006 144 42 % 52 % 40 % NA 38 % Pier Luigi Filosso, MD Sarkaria et al. 2011 100 University of Torino, Department of Thoracic Surgery 58 % 2014: 14 Centres 2054 patients Atypical Carcinoid LCNC Mixed Tumor SCLC Typical Carcinoid Unspecified Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery Aim of the study To evaluate the possible adjuvant CT effect on LCNC survival To assess clinicopathologic prognostic factors in a surgicallybased population of patient with LCNC Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery No. 400 pts % Age (median – IQR-) 66 (58-72) Gender (male) 252 63 Smokers (current/former) 99 25 Previous malignancy 99 25 I 185 48 II 110 29 III 76 20 IV 12 3 53 (44 CT; 9 RT) 13 146 37 pTNM Induction therapy Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery Adjuvant CT Overall survival 1.00 Median OS: 43 months 0.75 0.50 3-y surv rate: 54 % 5-y surv rate: 45 % 0.25 0.00 0 12 24 36 48 400 292 202 149 110 60 72 Months 84 96 108 120 54 35 25 22 At risk: 94 70 Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery OS according to adjuvant CT administration A slight improvement in OS was observed in those who received adjuvant CT (HR 0.82; 95%CI: 0.62-1.09, P=0.17) 1.00 0.75 0.50 0.25 No Yes 0.00 0 At risk: No 254 Yes 146 12 24 36 48 60 Months 72 84 96 108 120 182 110 126 76 92 57 68 42 59 35 42 28 33 21 22 13 19 6 17 5 Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery We observed a signal of an improved survival in LCNC patients treated with adjuvant CT We did not identify a particular subset of patients in which adjuvant CT might be more appropriate Prospective data collection (ESTS prospective database), will hopefully help to define more tailored treatment strategy for such aggressive neoplasm Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery My Thoughts Very Large Study of LCNC We All expected as much Adjuvant Chemotherapy Should be a Small Cell Regimen Cis/Etoposide PCI? Pier Luigi Filosso, MD University of Torino, Department of Thoracic Surgery Routine Venous Thromboembolism Screening after Pneumonectomy: The More You Look, the More You See Department of Thoracic and Cardiovascular Surgery Cleveland Clinic Foundation AATS 2015 STS Database General Thoracic Surgery Database DVT req. Rx Pulmonary Embolism 1% 1.2% 2011-13 Practice Change Routine screening pre discharge after pneumonectomy was initiated in 2006 as part of a quality improvement initiative Objectives • Ascertain the prevalence of VTE after pneumonectomy • Assess risk of developing VTE • Identify risk factors for VTE • Determine effect of VTE on survival Patients Pneumonectomy For Malignancy VTE Screened 2006 – 2012 n = 112 VTE Not Screened 1990 – 2001 n = 336 VTE Events Total n = 112 VTE 20 patients 50% In-hospital Discharge In 30 days 20% 10 4 Risk of VTE 1.0 %/day 0.75 Screened 0.5 Not screened 0.25 0 7 14 21 28 35 42 Days after Pneumonectomy Survival and VTE 100 Survival before VTE 80 % 60 40 Survival after VTE 20 0.0 0.5 1.0 1.5 Years 2.0 2.5 My Thoughts DVT post Px is a bad thing DVT is a Marker for an Unclear Mechanism of Mortality Right Heart failure Advanced Cancer Limited Pulmonary Reserve Giving Induction Radiation in Addition to Chemotherapy Is Not Associated with Improved Survival of NSCLC Patients with Operable Mediastinal Nodal Disease Chi-Fu Jeffrey Yang MD, Brian Gulack MD, Paul Speicher MD, Xiaofei Wang PhD, Mark Onaitis MD, David Harpole MD, Thomas D’Amico MD, Mark Berry MD, Matthew Hartwig MD Duke Cancer Institute Durham, NC Objective Assess outcomes of patients with operable stage IIIA-N2 disease who received induction chemotherapy (Chemo) vs induction chemoradiation (ChemoRT) National Cancer Data Base Hypothesis: No significant improvement would be observed with the addition of radiation to induction chemotherapy Down-staging Variable T stage down-staging N2 to N0/N1 down-staging Chemo (N = 528) Chemo+RT (N = 834) p-value 24% 46% 38% 58% <0.01 <0.01 • T stage down-staging was more common with induction chemoradiation • Nodal down-staging from N2 to N1/N0 was more common with the induction chemoradiation Overall Survival of Patients with Operable N2 NSCLC who Underwent Induction Chemotherapy vs. Induction Chemoradiation Treatment Median survival 5-year survival Induction CRT 3.3 years 41.4 % Induction CT 3.4 years 40.8 % p = 0.78 Induction CRT – 834 Induction CT – 528 698 445 533 341 406 278 356 227 299 188 205 130 110 62 49 29 My Thoughts There is almost always an association between downstaging (especially N) and survival improvement This relationship does not appear to hold true here Randomized Trial of Digital Versus Analog Pleural Drainage in Patients With or Without a Pulmonary Air Leak after Lung Resection. Sebastien Gilbert1,2 MD, Anna L McGuire3 MD MSc, Sonam Maghera4 BSc, Donna E Maziak1 MD MSc, Andrew J Seely1,2 MD PhD, Farid M Shamji1 MD, Sudhir Sundaresan1 MD, and P James Villeneuve1,2 MD PhD 1Division of Thoracic Surgery, The Ottawa Hospital 2The Ottawa Hospital Research Institute 3University of British Columbia 4Faculty of Medicine, University of Ottawa Ottawa, Canada Objective Compare digital and analog pleural drainage: Length of stay (primary) Duration of chest tube drainage (secondary) Take into account postoperative air leak status Hypothesis Digital pleural drainage = ↓length of stay (LOS) Regardless of postoperative air leak status Outcomes Group 1: Air leak absent (n=87) Analog Digital (n=43) (n=44) p Group 2: Air leak present (n=85) Analog Digital (n=42) (n=43) p LOS 4.3 (3.3-5.2) 4.0 (3.2-5.1) 0.09 6.2 (5.2-9.1) 6.2 (4.3-8.1) 0.36 CT Drainage 3.0 (2.9-4.9) 2.9 (2.2-3.9) 0.05 5.6 (4.0-8.9) 4.9 (3.1-6.4) 0.11 Median number of days with interquartile range My Thoughts Control Group had extreme non-standard of care air leak assessment (2 independent observers with a 3rd to break the tie) Fair comparison? Chest Tube removal is a daylight procedure. Accelerated hemithoracic radiation followed by extrapleural pneumonectomy for malignant pleural mesothelioma Marc de Perrot, Ronald Feld, Natasha B Leighl, Andrew Hope, Thomas K Waddell, Shaf Keshavjee, BC John Cho Toronto Mesothelioma Research Program University Health Network Toronto, Canada Rational • Optimal delivery of radiation to the primary tumor based on PET and CT scan findings • Sterilization of the edges of the tumor before surgery to decrease the risk of seeding • Short treatment • Potential immunogenic benefit Postoperative grade 3+ complications (n=24) Atrial fibrillation Empyema Pulmonary emboli Pneumonia Chylothorax Hemothorax Wound problem Patch dehiscence Others 0 2 4 6 8 Number of patients* *6 patients had more than one grade 3+ complication 10 12 Postoperative grade 3+ complications Rate of grade 3+ complications decreased over time p=0.02 Percentage of grade 3+ complications 70 60 50 40 Other complications than atrial fibrillation 45% 30 12% 20 10 Atrial fibrillation alone 15% 17% First 20 patients Last 42 patients 0 Pathological stage 94% stage III and IV 52% N2+ Overall survival Intention-to-treat analysis (n=62) Percent survival 100 80 60 40 20 Median survival 36 months 0 0 12 24 36 48 Months after start of treatment 60 Overall survival by histologic subtypes cT1-3N0M0 treatment naive (n=56) Overall survival (%) 100 Epithelial 76% 80 Biphasic 60 p=0.001 40 29% Median survival: Epithelial 51 mo Biphasic 10 mo 20 0 0 12 24 36 48 Months after start of treatment 60 My Thoughts Very Novel Treatment Superb Results 100% Resectability rate because the Lung has to come out! 52 Is surgical resection justified for myasthenia gravis? Long-term results in over 1000 cases. Andrew J. Kaufman, MD; Justin Palatt, MD; Mark Sivak, MD, Peter Raimondi, BS, Dong-Seok Lee, MD; Andrea Wolf, MD, MPH; Fouad Lajam, MD, Faiz Bhora, MD; Raja M. Flores MD. Department of Thoracic Surgery, Mount Sinai School of Medicine Andrew J. Kaufman MD Assistant Professor, Thoracic Surgery Mount Sinai School of Medicine Chief, Thoracic Surgery Mount Sinai Beth Israel New York, New York Methods • Retrospective review of a prospectively maintained database of thymectomy patients from 1941-2013. • 1002 included in study. • Inclusion Criteria: • Thymectomy • Age at time of surgery • Gender • Duration of symptoms before surgery • Osserman Classification before and after surgery • Surgical technique • Presence of thymoma • Date of remission, and status at last follow-up Interval-censored Kaplan-Meier estimate of time to complete stable remission Estimated Failure Probability Probability of CSR Cumulative Failure Probability 0.5 0.4 0.3 Time Interval in Years Estimate of CSR Estimate of Non-CSR Standard Error 0-2 15.99% 84.01% 1.42% 3-7 19.39% 80.61% 1.49% 8-8 19.43% 80.57% 1.49% 9-10 27.68% 72.32% 1.72% 11-15 29.14% 70.86% 1.74% 16-24 32.17% 67.83% 1.89% 25-39 36.65% 63.35% 2.25% 40-50 47.31% 52.69% 8.98% 0.2 0.1 0.0 0 10 20 30 Time Time to Remission in years 40 50 My Thoughts • 60 year Study • Lessens the impact • Data not particularly granular • But, very large study with important bottom line Adjuvant Radiation is Not Associated with Improved Survival in Patients with Positive Margins Following Lobectomy for Stage I & II Non-Small Cell Lung Cancer Brian C Gulack, MD; Jeffrey Chi-Fu Yang, MD; Paul J Speicher, MD, MHS; H. Volkan Kara, MD; Thomas A D’Amico, MD; Mark F Berry, MD, MHS; Matthew G Hartwig, MD 57 Background • Lobectomy – Most common surgical procedure performed for stage I or II NSCLC. – 4-6% associated with positive margins. • Current NCCN guidelines for positive margins: – Re-resection +/- chemotherapy (preferred). – Adjuvant radiation +/- chemotherapy. – Based on limited data. • Reviewed the National Cancer Data Base (NCDB) in order to better guide therapy for this clinical scenario. – Hypothesis: Significant benefit from adjuvant XRT 58 Methods Lobectomy for Stage I or II NSCLC Negative Margins Positive Margins Adjuvant Radiation No Adjuvant Radiation Adjuvant Radiation Pneumonectomy Propensity Match 59 Results No Adjuvant Radiation Adjuvant Radiation Adjusted HR: 1.08 (95% CI: 0.88, 1.32) P = 0.009 Covariates included in adjustment: age, sex, race, insurance status, Charlson/Deyo comorbidity index, pathologic grade, pathologic stage. Results Pneumonectomy Lobectomy w/XRT 16 My Thoughts • Very Ambitious Study • Is the Database really capable of answering question • Pneumonectomy inclusion is hard sell • Good place to start 62 Demographics associated with POSVT Variables: Demographic OR CI P-value Male gender 1.46 1.33-1.59 <0.0001 55-64 2.35 1.84-2.96 <0.0001 65-74 4.23 3.29-5.43 <0.0001 >75 6.33 4.89-8.19 1.52 1.34-1.73 Age (18-54 referent) White race <0.0001 <0.0001 “Uncomplicated” POSVT Outcome No SVT, uncomplicated course (n=12,064) Isolated SVT, no other complications (n=1,116) p-value Postoperative stroke 0.2% <1.0% <0.05* In-hospital mortality 0.2% <1.0% >0.70* Median length of stay (Q1;Q3) 5 (4;6) 6(5;8) <0.001 90-day readmission 16.6% 20.3% 0.003 90-day readmission with stroke 0.6% 1.4% 0.006 My Thoughts • Typical Non-Surgical Risks (Age, COPD, CHF) • Slightly Increased with Thoracotomy • Surprising Stroke Risk • No information on Treatment/prophylaxis Unexpected Readmission after Lung Cancer Surgery: A Benign Event? Varun Puri, Aalok P Patel, Traves D Crabtree, Jennifer M Bell, Stephen R Broderick, Daniel Kreisel, A Sasha Krupnick, G Alexander Patterson, Bryan F Meyers Objectives • Study incidence and predictors of unanticipated postoperative readmission after lung resection for cancer • Assess short- and long-term implications • Hypothesis - Unexpected readmission will be associated with a risk of short-and long-term mortality Objectives • Study incidence and predictors of unanticipated postoperative readmission after lung resection for cancer • Assess short- and long-term implications • Hypothesis - Unexpected readmission will be associated with a risk of short-and long-term mortality Results Path. Stage I Path. Stage II Path. Stage III All p <0.001 Conclusions • Unplanned readmissions (4.3%) are not infrequent after lung resection • These events are associated with elevated risk of short- and longterm mortality • Greater resource allocation to high risk patients • Consider regionalization of care My Thoughts • Readmission is surrogate for something • Patient performance status? • Surprising late effect • Hazard Function Development of a Nomogram for Predicting Outcomes after Sublobar Resection for Lung Cancer An Analysis of ACOSOG Z4032 Michael Kent, MD on behalf of the ACOSOG Z4032 Investigators AATS Annual Meeting, 2015 Introduction ACOSOG Z4032 • Z4032 was a randomized, prospective trial • Compared sublobar resection to sublobar resection with brachytherapy • Accrual 2006-2010 (n=224) • Included 41 centers and 48 surgeons Results Baseline Demographics • Median age: 70 • Median F/U: 4.4 years • Mean DLCO: 46% predicted • Wedge resection: n 129 (74.6%) • No LN sampling: n 61 (35.3%) Overall Survival Multivariate Analysis Factors Hazard Ratio p-value Age 1.03 (1.00,1.06) 0.04 Baseline DLCO% 0.97 (0.95,0.99) <0.01 Margin Tumor Ratio 0.83 (0.53,1.28) 0.39 Maximum Tumor Diameter 1.29 (1.00.1.68) 0.05 Histology Type 1.24 (0.76,2.02) 0.39 My Thoughts • Excellent 5 yr survival • Independent from LN status and Margin • Most Dependent on Gas exchange • Turns out there are worse things than Lung Cancer Spotlight on Esophageal Perforation – A multinational study using the Pittsburgh Esophageal Perforation Severity Scoring System Michael Schweigert Department of Thoracic Surgery The Pittsburgh PSS Points are given to each variable according to the following scale: • 1 = age > 75 years, tachycardia (> 100 bpm), leukocytosis ( > 10000 WBC/ml), pleural effusion (on chest x-ray, CT or barium swallow); • 2 = fever (> 38.5 °C), noncontained leak (on barium swallow or CT), respiratory compromise (respiratory rate > 30, increasing oxygen requirement or need of mechanical ventilation), time to diagnosis > 24 hours; • 3 = presence of cancer, hypotension 79 Results: Etiology & Site • Etiology: • Spontaneous 119 (41.3%) • Iatrogenic (instrumentation) 85 (29.5%) • Traumatic perforation 84 (29.2%). • Site of perforation: • Cervical 45 (16%) • Thoracic 202 (71.6%) • Abdominal 35 (12.4%). 80 Results: PSS Groups In accordance with the original publication we divided the study population into three groups: 81 My Thoughts • You don’t get a second chance to make a first impression on perforation • Choose Well • This Scoring system can help 25.04.2014 Verfasser 82 Final Thoughts In Case you’ve missed my “In case you missed…” Too Bad Read the Meeting book Get here earlier next year