Asthma
advertisement

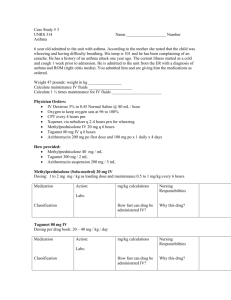
Asthma Asthma Definition Reactive airway disease Chronic inflammatory lung disease Inflammation causes varying degrees of obstruction in the airways Asthma is reversible in early stages Triggers of Asthma Allergens Exercise Respiratory Infections Nose and Sinus problems Drugs and Food Additives GERD Emotional Stress Early and Late Phases of Responses of Asthma Fig. 28-1 Asthma Pathophysiology Bronchospasm Airway inflammation Asthma Pathophysiology Early-Phase Response Peaks 30-60 minutes post exposure, subsides 3090 minutes later Characterized primarily by bronchospasm Increased mucous secretion, edema formation, and increased amounts of tenacious sputum Patient experiences wheezing, cough, chest tightness, and dyspnea Asthma Pathophysiology Late-Phase Response Characterized primarily by inflammation Histamine and other mediators set up a selfsustaining cycle increasing airway reactivity causing hyperresponsiveness to allergens and other stimuli Increased airway resistance leads to air trapping in alveoli and hyperinflation of the lungs If airway inflammation is not treated or does not resolve, may lead to irreversible lung damage Factors Causing Airway Obstruction in Asthma Fig. 28-3 Summary of Pathophysiologic Features Reduction in airway diameter Increase in airway resistance r/t Mucosal inflammation Constriction of smooth muscle Excess mucus production Asthma Clinical Manifestations Unpredictable and variable Recurrent episodes of wheezing, breathlessness, cough, and tight chest Asthma Clinical Manifestations Expiration may be prolonged from a inspiration-expiration ratio of 1:2 to 1:3 or 1:4 Between attacks may be asymptomatic with normal or near-normal lung function Asthma Clinical Manifestations Wheezing is an unreliable sign to gauge severity of attack Severe attacks can have no audible wheezing due to reduction in airflow “Silent chest” is ominous sign of impending respiratory failure Asthma Clinical Manifestations Difficulty with air movement can create a feeling of suffocation Patient may feel increasingly anxious Mobilizing secretions may become difficult Asthma Clinical Manifestations Examination of the patient during an acute attack usually reveals signs of hypoxemia Restlessness Increased anxiety Inappropriate behavior Increased pulse and blood pressure Pulsus paradoxus (drop in systolic BP during inspiratory cycle >10) Asthma Complications Status asthmaticus Severe, life-threatening attack refractory to usual treatment where patient poses risk for respiratory failure Asthma Diagnostic Studies Detailed history and physical exam Pulmonary function tests Peak flow monitoring Chest x-ray ABGs Asthma Diagnostic Studies Oximetry Allergy testing Blood levels of eosinophils Sputum culture and sensitivity Asthma Collaborative Care Education Start at time of diagnosis Integrated into every step of clinical care Self-management Tailored to needs of patient Emphasis on evaluating outcome in terms of patient’s perceptions of improvement Asthma Collaborative Care Acute Asthma Episode O2 therapy should be started and monitored with pulse oximetry or ABGs in severe cases Inhaled -adrenergic agonists by metered dose using a spacer or nebulizer Corticosteroids indicated if initial response is insufficient Asthma Collaborative Care Acute Asthma Episode Therapy should continue until patient • is breathing comfortably • wheezing has disappeared • pulmonary function study results are near baseline values Asthma Collaborative Care Status asthmaticus Most therapeutic measures are the same as for acute Increased frequency & dose of bronchodilators Continuous -adrenergic agonist nebulizer therapy may be given Asthma Collaborative Care Status asthmaticus IV corticosteroids Continuous monitoring Supplemental O2 to achieve values of 90% IV fluids are given due to insensible loss of fluids Mechanical ventilation is required if there is no response to treatment Asthma Drug Therapy Long-term control medications Achieve and maintain control of persistent asthma Quick-relief medications Treat symptoms of exacerbations Asthma Drug Therapy Bronchodilators -adrenergic agonists (e.g., albuterol, salbutamol[Ventolin]) Acts in minutes, lasts 4 to 8 hours Short-term relief of bronchoconstriction Treatment of choice in acute exacerbations Asthma Drug Therapy Bronchodilators Useful in preventing bronchospasm precipitated by exercise and other stimuli Overuse may cause rebound bronchospasm Too frequent use indicates poor asthma control and may mask severity Asthma Drug Therapy Bronchodilators (longer acting) – 12 or 24 hr; useful for nocturnal asthma Avoid contact with tongue to decrease side effects Can be used in combination therapy with inhaled corticosteroid 8 Asthma Drug Therapy Antiinflammatory drugs Corticosteroids (e.g., beclomethasone, budesonide) Suppress inflammatory response Inhaled form is used in long-term control Systemic form to control exacerbations and manage persistent asthma Asthma Drug Therapy Antiinflammatory drugs Corticosteroids Do not block immediate response to allergens, irritants, or exercise Do block late-phase response to subsequent bronchial hyperresponsiveness Inhibit release of mediators from macrophages and eosinophils Asthma Drug Therapy Anti-inflammatory drugs Mast cell stabilizers (e.g., cromolyn, nedocromil) Inhibit release of histamine Inhibit late-phase response Long-term administration can prevent and reduce bronchial hyper-reactivity Effective in exercise-induced asthma when used 10 to 20 minutes before exercise Asthma Drug Therapy Leukotriene modifiers (e.g. Singulair) Leukotriene – potent bronchco-constrictors and may cause airway edema and inflammation Have broncho-dilator and anti-inflammatory effects Asthma Patient Teaching Related to Drug Therapy Correct administration of drugs is a major factor in determining success in asthma management Some persons may have difficulty using an MDI and therefore should use a spacer or nebulizer DPI (dry powder inhaler) requires less manual dexterity and coordination Asthma Patient Teaching Related to Drug Therapy Inhalers should be cleaned by removing dust cap and rinsing with warm water -adrenergic agonists should be taken first if taking in conjunction with corticosteroids Nursing Management Nursing Diagnoses Ineffective airway clearance Anxiety Ineffective therapeutic regimen management Nursing Management Planning Normal or near-normal pulmonary function Normal activity levels No recurrent exacerbations of asthma or decreased incidence of asthma attacks Adequate knowledge to participate in and carry out management Nursing Management Health Promotion Teach patient to identify and avoid known triggers Use dust covers Use of scarves or masks for cold air Avoid aspirin or NSAIDs Desensitization can decrease sensitivity to allergens Nursing Management Health Promotion Prompt diagnosis and treatment of upper respiratory infections and sinusitis may prevent exacerbation Fluid intake of 2 to 3L every day Nursing Management Health Promotion Adequate nutrition Adequate sleep Take -adrenergic agonist 10 to 20 minutes prior to exercising Nursing Management Nursing Implementation Acute Intervention Monitor respiratory and cardiovascular systems Lung sounds Respiratory rate Pulse BP Nursing Management Nursing Implementation ABGs Pulse oximetry FEV and PEFR Work of breathing Response to therapy Nursing Management Nursing Implementation Nursing Interventions Administer O2 Bronchodilators Chest physiotherapy Medications (as ordered) Ongoing patient monitoring Nursing Management Nursing Implementation An important goal of nursing is to decrease the patient’s sense of panic Stay with patient Encourage slow breathing using pursed lips for prolonged expiration Position comfortably Nursing Management Nursing Implementation The patient must learn about medications and develop self-management strategies Patient and health care professional must monitor responsiveness to medication Patient must understand importance of continuing medication when symptoms are not present Nursing Management Nursing Implementation Important patient teaching: Seek medical attention for bronchospasm or when severe side effects occur Maintain good nutrition Exercise within limits of tolerance Nursing Management Nursing Implementation Important patient teaching (cont.): Patient must learn to measure their peak flow at least daily Asthmatics frequently do not perceive changes in their breathing Nursing Management Nursing Implementation Counseling may be indicated to resolve problems Relaxation therapies may help relax respiratory muscles and decrease respiratory rate Nursing Management Nursing Implementation Peak Flow Results Green zone Usually 80-100% of personal best Remain on medications Nursing Management Nursing Implementation Peak Flow Results Yellow zone Usually 50-80% of personal best Indicates caution Something is triggering asthma Nursing Management Nursing Implementation Peak Flow Results Red zone 50% or less of personal best Indicates serious problem Definitive action must be taken with health care provider