Update on Alzheimer's Research and Clinical Trials
advertisement

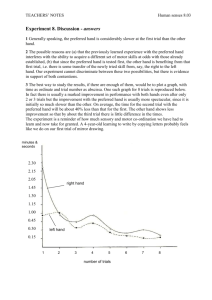
Update on Alzheimer’s Research and Clinical Trials Dr Cathy Short Neurologist Memory Disorders Unit Department of Neurology The Queen Elizabeth Hospital September 2015 INTRODUCTION • There are more than 342,800 Australians living with dementia • This number is likely to approach 1 million by 2050 unless there is a significant breakthrough in treatment • As of 2015, there are 46.8 million people with dementia worldwide • This number is expected to double every 20 years to approx. 74.7 million people in 2030 and 131.5 million in 2050 • Total estimated worldwide cost of dementia as of 2015 is US$818 billion • This cost has increased by 35% since it was last estimated in 2010 AD Research AD research continues both here and internationally in many different areas We will review some of the following: • treatment - drugs - non- pharmacological therapies • prevention - epidemiology - risk factors • diagnosis - Genetics - biomarkers (imaging, CSF, serum) Current medication for AD • 24 years after the first descriptions of the therapeutic benefits of tacrine ( one of the first AChEI’s) we still only have symptomatic therapies for AD. • Only 4 drugs are regularly used for AD: donepezil, galantamine, rivastigmine and memantine. • No new drug has been marketed for nearly 20 years • One of the major obstacles to progress in this field is a lack of understanding as to exactly what causes AD Alzheimer’s Disease Theories • A number of theories have been proposed to explain the cause of AD but to date, no one theory can adequately explain all aspects of the disease • Precise mechanisms for AD progression are also unclear • There are 3 major theories (Cholinergic, Amyloid, Tau) that are currently regarded as the most likely explanation for AD • They are being used as the basis for therapeutic development AD Pathology • Histopathologically, when we examine brain tissue under a microscope the 2 hallmarks of Alzheimer’s disease are extracellular amyloid plaques and intraneuronal neurofibrillary tangles (NFTs) composed of tau • Described in 1907 by Alois Alzheimer they remain the major pathological abnormalities seen in AD Amyloid Cascade Hypothesis • This has been the main focus of research to date • Beta-amyloid (Aβ) is the main component of amyloid plaques (one of the pathological hallmarks of AD) • Scientists now have a detailed understanding of how this protein fragment is clipped from it’s parent compound amyloid precursor protein (APP) by two enzymes – beta-secretase and gamma-secretase • Researchers are developing medications aimed at every point in the amyloid processing pathway • It has been postulated that after the deposition of amyloid plaques that a cascade ensues • This leads to inflammation and ultimately formation of neurofibrillary tangles (NFT’s) – the other major hallmark of AD • This causes problems with neurotransmitters and neuronal function in the brain and ultimately neurone death Anti-Amyloid strategies Immunotherapy • Initial studies showed that injecting animals with beta-amyloid lead to a good antibody response and clearing of the amyloid plaques from their brains • Subsequent human studies were prematurely ceased (2002) due to development of brain inflammation (meningoencephalitis) in 6% • However, there was evidence that the treatment had removed amyloid plaque • The concept of active immunisation hasn’t been abandoned yet – several pharmaceutical companies are in the early phases of developing new active vaccines Anti-amyloid strategies immunotherapy • As an alternative to actively immunising with beta-amyloid, the next studies looked at “passive immunisation” • This bypasses the need to respond to an antigen • Passive immunotherapy remains the leading approach today to disease–modifying treatment for AD • These monoclonal antibodies target various domains of the beta-amyloid peptide and prevent aggregation or speed up removal Monoclonal antibodies • To date, a number of monoclonal antibodies have been studied in clinical trials including bapinezumab and gantenerumab but were stopped prematurely due to lack of perceived efficacy • However analyses of some subgroups have shown benefits that have lead to further studies • There are still a number of other monoclonal antibodies that are being actively studied and some are showing early positive results– solanezumab, crenezumab and adecanumab – we await the outcomes of these studies Anti-amyloid strategies – reducing production • Another approach to reducing the amount of amyloid in the brain is to reduce the production • Inhibiting the enzymes that help produce amyloid-beta will lead to less being produced • BACE inhibitors specifically inhibit the betasecretase enzyme involved in the amyloid cascade. • There are a number of studies in progress (at TQEH and RAH) at the moment looking at the benefits of BACE inhibition in AD Anti-amyloid strategies – reducing production • Drugs have also been developed to inhibit gamma-secretase – the other main enzyme involved in producing beta-amyloid • There have been problems with unwanted side-effects from these agents – skin cancer, rash and hair discolouration • Semagacestat showed promise in early trials but failed to show benefit in phase 3 trials • Two other gamma-secretase inhibitors have also failed to show benefit • Pharmaceutical companies are currently working on developing more highly selective gamma-secretase inhibitors that will cause less side effects and inhibit beta-amyloid production more effectively Anti-amyloid strategies – inhibiting aggregation • Curcumin (a substance in the spice Turmeric) – has anti-oxidant, anti-inflammatory and antiaggregation properties • It binds beta-amyloid and reduces amyloid plaque burden in mice • Phase 2 trial is ongoing – if effective – it may be a favoured therapy as toxicity is low Tau • Far fewer drug trials have focussed on tau • Interest has grown recently because of difficulties with antiAβ treatments • Mouse and primate models of AD show amyloid plaques that respond to anti-amyloid therapy but these animal models don’t replicate the tau pathology seen in human AD • Aged dogs develop an AD-like disorder with amyloid and NFT’s • Treatment of these animals with anti-amyloid therapies reduces plaque load but doesn’t alter cognition or change tau pathology • There is a very robust correlation between tau pathology and clinical measures of dementia Methylthioninium Chloride (Methylene Blue) • First drug targeting tau • Drug is derived from the dye used to stain NFT’s in neuropathological studies • Primarily inhibits tau aggregation • Phase 2 study showed cognitive benefits • SPECT and FDG-PET results also encouraging • Phase 3 trial for mild-moderate AD (both TQEH and RAH finished recruiting) will be finished February 2016 Other tau therapies • Several other drugs that inhibit the development of tau have been studied • Observational studies in geriatric patients taking chronic lithium for BPAD were found to have reduced risk of developing AD • Lithium inhibits chemical changes in tau that leads to formation of NFT’s • Studies on Lithium have been mixed – some have shown benefit with very low doses in mild cognitive impairment, others have shown worsening confusion – further studies are needed Other tau therapies • Tau immunisations have been studied in animal models and have shown a reduction in the amount of tau and also clinical benefits – Phase I trials are beginning Neurotransmitters and Receptors • 5HT6 (serotonergic) receptor in the brain is a promising drug target for Alzheimer’s Disease • There is good evidence that this receptor is involved in memory and learning • Antagonism of this receptor causes modulation of a number of other neurotransmitters (DA, ACh, NAd) and pathways in the brain • Phase II trials showed improved cognition with the addition of a 5HT rec. antagonist in moderate AD patients already on donepezil • Phase III trials are currently underway – recruiting at TQEH (for patients on any AD treatment) Inflammation in Alzheimer's Disease • All chronic neurodegenerative disorders and aging involve inflammation, oxidative stress and cellular dysfunction • Leads to impaired function and loss of brain cells • These brain cells are no longer able to participate in neuronal networks needed for cognitive, behavioural and motor function • Leads to self-perpetuating cycle of cellular injury and predisposition to further insults • Some research suggests that these inflammatory processes are the underlying cause of AD and that it leads to Aβ and tau accumulation Anti-inflammatory therapies • Markers of inflammation have been recognised in AD for a long time • Large epidemiological studies have demonstrated a lower prevalence of AD in long term users of NSAID’s • Large number of therapeutic trials of NSAID’s in AD (1993-2004) incl: Ibuprofen, indomethacin, naproxen, celecoxib ,rofecoxib and other anti – inflammatory meds such as prednisolone • All were negative Anti-Inflammatory Therapy • Primary prevention study (Alzheimer’s Disease Antiinflammatory Prevention Trial or ADAPT) of naproxen, celecoxib and placebo in cognitively normal elderly with a first degree relative with dementia • prematurely suspended -↑ cardiac and cerebrovascular events • Both drugs failed to ↓ incidence of AD after 2 years of treatment • 4 year follow-up found those exposed to naproxen were protected from onset of AD by 67% c/w placebo • NSAID’s not considered to be practical treatment option for AD – tolerability and safety issues Vitamins and Anti-oxidants • To date there has been insufficient evidence that low levels of vitamin B12 in elderly ↑ risk for dementia or that supplements improve performance • Again, studies looking at folate supplementation have been inconsistent • In 2014 a group of Oxford University researchers assembled all the best clinical trial data involving 22,000 people and concluded that taking B vitamins and folate doesn’t slow mental decline as we age, nor is it likely to prevent AD Vitamins and Anti-oxidants • Vitamin D – primarily has functions in bone health and metabolism but may also have antioxidant and anti-inflammatory properties • not clear whether Vitamin D deficiency is causally related to cognition or is a marker for another process • not confirmed that Vitamin D supplementation will have positive effect on cognition Vitamins and Anti-oxidants • Vitamins E, C and beta-carotene (pre-cursor for Vitamin A) – all powerful anti-oxidants • Epidemiological studies show that low intake is associated with ↑ dementia risk but association remains inconsistent • Multiple clinical trials provide evidence that supplements with these compounds did not alter cognitive outcomes in MCI, AD or healthy elderly but results still debated • Concern about cardiovascular risk of Vitamin E are likely to prevent further studies of this in AD Vitamins and Anti-oxidants • Ginkgo-biloba has been studied in trials • Reasonably firm evidence that it does not alter the risk of dementia or improve cognitive performance in healthy elderly • Potential side-effects of bleeding tendency and drug interactions Vitamins and Anti-oxidants • Omega-3 fatty acids found in fish oil and nuts – thought to be neuroprotective • Studies have failed to show any improvement in cognition in AD patients • In elderly without AD – inconclusive evidence that they may slow cognitive decline • Further large –scale studies needed Mediterranean diet • This diet is rich in fruits, vegetables, olive oil, legumes, whole grains and fish • Studies have shown that people that closely follow a Mediterranean diet are less likely to have AD than those who don’t • Research suggests that a Mediterranean diet may – -slow cognitive decline in older adults -reduce the risk of MCI progressing to AD -slow the progression of AD and prevent disease-related deaths Diet in Alzheimer’s Disease • A recent study looked at 3 different diets: 1. Mediterranean diet 2. DASH diet (designed to treat hypertension – low salt and sugar) 3. MIND diet (Combination of the above 2 diets)emphasizes natural plant-based foods, limited saturated fats, encourages consumption of berries and green leafy vegetables (known to specifically benefit brain health) Diet in Alzheimer’s Disease • People that strictly followed any of these 3 diets had a lower risk of AD • Even a modest adoption of the MIND diet approach such as eating 2 vegetable servings per week, 2 berry servings per week and one fish meal per week appeared to lower the risk of AD • Researchers speculate that making healthy food choices may improve cholesterol and blood sugar levels and overall vessel health which may in turn reduce risk of MCI and AD • Another theory is that a Mediterranean diet may help prevent brain tissue loss • More studies are needed to know to what degree this diet prevents AD or slows cognitive decline “Brain Training” • This is quite broad and can include a range of structured mentally stimulating activities such as: crosswords learning a new language reading a book undertaking further education dedicated computerised brain training activities that focus on memory, attention or other cognitive functions • Recent studies have found that “computerised brain training” is only modestly effective at improving cognitive performance in healthy older adults • Further studies are about to start to see whether intensive computerised training can stop the progress of cognitive decline and the onset of dementia Physical Activity • Research into potential for physical exercise to reduce the risk of dementia is continuing • There are still no randomised trials available yet – several studies have found that physical activity in early, mid and later life is associated with lower risk of cognitive decline and dementia • Other studies have found that people who exercise experience a slower loss of brain tissue as they age. • In addition people who exercise regularly are less likely to have cerebro- and cardio-vascular disease which is associated with increased risk of AD Physical Activity • It is also beneficial in patients that have dementia • It can help prevent muscle weakness, mobility problems and other health complications associated with inactivity • It also helps reduce symptoms of stress, anxiety and depression • 3 types of exercise should be included in the program– sustained aerobic exercise, weight training and flexibility and balance training • If an exercise program is incorporated in the early stages of dementia it is more likely to be maintained as the condition progresses Insulin Resistance • Insulin resistance and the way the brain processes insulin may be linked to AD • Researchers are exploring the role of insulin in the brain and closely related questions of how brain cells use sugar and produce energy • Researchers have been studying diabetic medications such as pioglitazone which also has potent anti-inflammatory effects Insulin resistance • Preliminary studies with pioglitazone have had mixed results but there is a worldwide phase 3 study underway (site in Melbourne) • The study is looking at cognitively normal patients who are considered at risk of developing AD and giving either pioglitazone or placebo and giving placebo to those considered low risk • We await the results Vascular disease and Alzheimer’s • It is well known now that vascular risk factors including hypertension, heart disease, smoking, high cholesterol, obesity, stroke and diabetes are also risk factors for Alzheimer's disease. • The relationship between vascular disease and AD is complex and still not fully understood • It is likely that vascular disease in the brain lowers the threshold for the clinical expression of AD pathology Vascular disease and Alzheimer’s • Some observational studies have shown that the rate of cognitive decline in AD is reduced with better management of vascular risk factors but results have been inconsistent • Larger randomised controlled trials are needed over longer periods of time to determine effectiveness of treatment of vascular risk factors in AD • The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER study) is one such study that is showing promising preliminary results at 2 years • Preventative study looking at benefits of a combination of diet, exercise, cognitive training and vascular risk factor monitoring in an “at risk” population Research in Familial Alzheimers Disease • There are 3 known mutations that cause FAD – this accounts for less than 5% of all cases of AD • There are several new studies looking at antiamyloid drugs in asymptomatic patients who either have one of the known rare genetic mutations or are at very high risk of developing AD based on their family history • It is hoped that these studies will give us more insight into whether treatment at the asymptomatic stage will prevent later development of AD Alzheimers Prevention Initiative • The Alzheimers Prevention Initiative (API) is an international consortium established to conduct research into an extended family (5000 members) in Colombia South America • This family carry the presenilin 1 mutation that affects amyloid processing • API are performing a study on asymptomatic individuals that carry the PS1 mutation using the monoclonal antibody crenezumab vs. placebo • This is a five year study and is still recruiting Dominantly Inherited Alzheimer Network (DIAN) • DIAN is an international initiative funded by the National Institute on Ageing (NIA) in the USA. • The network tracks individuals from families in whom an AD mutation has been identified • One of their goals is to detect physical or mental changes that distinguish those who inherit a mutation from those who do not. • The DIAN-TU study is looking at asymptomatic patients with a known mutation or at very high risk of developing AD and treating them with one of 2 monoclonal antibodies (solanezumab and gantenerumab) vs. placebo • This study is still recruiting (one site in Australia at the Austin Hospital) and is due for completion end 2019 Biomarkers • Making a diagnosis of Alzheimers disease is still essentially a clinical diagnosis • It is not a difficult diagnosis to make when the disease is clinically obvious but it can be challenging when the disease presentation is atypical or a patient presents at a very early stage • Having a diagnostic biomarker available would avoid any uncertainty and allow a definitive diagnosis to be made. • In addition to investigating experimental drugs, there are a range of clinical trials in progress examining various brain imaging techniques (eg. amyloid and tau PET) as well as the testing of a range of potential biomarkers in CSF and blood Biomarkers • Researchers hope that these techniques will one day provide methods to definitively diagnose AD in it’s earliest and most treatable stages • Ideally we could diagnose before symptoms appear and start treatment in this asymptomatic phase before significant neurodegeneration has occurred • We now know that the pathological changes of AD (seen on amyloid PET scans) can start up to 20 years before cognitive symptoms appear • This is perhaps why many trials done later in the disease have not been effective • Biomarkers may also eventually offer better methods to monitor response to treatment Outlook • There are often no simple solutions to complex problems and AD is a good case in point • Clinical trial results to date have been disappointing for several reasons: our understanding of the pathophysiology , the range of causes and how AD progresses from preclinical to advanced disease is still limited. too great a focus on amyloid-directed therapy – need to look at non-amyloid targets such as tau, antioxidants/neuroprotectants and others giving treatment too late in the disease process Outlook • In the future, AD may be treated like other chronic diseaseswith a mixture of disease-modifying and symptomatic therapies used in combination and in sequence • Likely scenario could be: Start AChEI Add a disease-modifying drug eg. monoclonal ab Change to another disease-modifying drug if disease progresses Consider changing/ adding another agent such as a BACE inhibitor or 5HT receptor antagonist • Limitations will be adverse effects and affordability Outlook • Although there have been many obstacles and setbacks along the way to developing treatment for AD – the future still looks promising • We are hopeful that an effective treatment will become available in the near future • Trials of several promising agents are in progress here and internationally Clinical Trials in AD • RAH and TQEH currently both have AD clinical trials centres • Soon we will be combining to one large AD trials centre based at TQEH • Clinical trials will be co-located with a large Multidisciplinary Memory Service • This will be known as the Central Adelaide Local Health Network (CALHN) Memory Service and will provide a multi-disciplinary approach to diagnosing and managing dementia with ongoing support for patients and their carers through a case manager. Current RAH AD trials • Merck – mild to moderate AD – BACE inhibitor – 2 years plus extension study • Merck –prodromal AD – BACE inhibitor – 2 years plus extension study • Marguerite road study – mild AD –monoclonal antibody (Gantenerumab)– 2 years • AMARANTH – prodromal/mild AD – BACE inhibitor – 2 years • AZTherapies – prodromal AD -cromolyn sodium (intal) / ibruprofen (brufen) – 2 years Clinical Trials at TQEH • Merck – mild to moderate AD – BACE inhibitor – 2 years plus extension study • Lundbeck- moderate AD (MMSE 12-22) – 5HT receptor antagonist (Idalopiridine) -6 months actively recruiting • Marguerite Road – mild AD – monoclonal antibody (Gantenerumab) – 2 years • Roche – monoclonal antibody (Crenezumab) – in planning stages – to start Dec 2015/Jan 2016 THANK YOU Please contact TQEH Memory Disorders Unit and Clinical Trials Ph: 82226748, Fax: 82226435 Or RAH Clinical trials centre Ph : 8222 2798 Fax :8222 2799 Any new referrals for diagnosis, treatment or involvement in clinical trials Patient and carer support for clinical trials is an important part of finding a cure for AD!