eLearning PowerPoint Template
advertisement

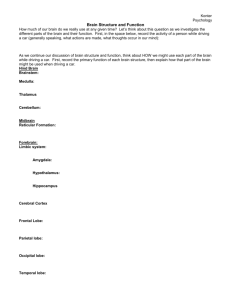
Localization in Neurologic Diagnosis Part 1 D. Joanne Lynn, MD Associate Professor of Neurology Associate Dean of Student Life Joanne.Lynn@osumc.edu Objectives Be able to accurately differentiate between examination findings suggesting upper vs. lower motor neuron pathology Correlate neurologic signs and clinical features to the appropriate level of the neuroaxis for the following neurologic localizations: Focal cortical disease, including a gross classification of aphasias; Cerebellar disease; Brainstem lesions; Spinal cord disease; Root and peripheral nerve disease; Neuromuscular junction dysfunction; Myopathy Objectives – continued… Define dysarthria, dysphagia, aphasia, aphonia. Compare and contrast Broca’s, Wernicke’s, conduction and global aphasia. List the primary functions of the frontal, parietal, temporal, and occipital lobes. Correlate visual field deficits with lesions along the visual pathways. Describe abnormalities of clinical eye movements that will be caused by lesions in cerebral and brainstem pathways that control eye movements. Recognize clinical presentations that suggest brainstem pathology: grouped cranial nerve palsies, crossed motor and sensory findings. Recognize clinical syndromes related to spinal cord pathology based on examination findings of motor and sensorydeficits. Identify motor, sensory and reflex abnormalities that occur in C6, C7, C8, L5 and S1 radiculopathies. Holism vs. Cortical localization Holism – all parts of the brain are similar in function, undifferentiated and work together as an aggregate field Localism – the concept that specific neurons and areas of the brain have specific functions Connectionism – a view that mental or behavioral phenomena are the product of interconnected networks of simple units. Cortical Localization vs. Holism Phineas Gage – 1848 Broca and M. Leborgne – 1861 Wilder Penfield – electrical stimulation results Animal ablation studies Functional studies by PET – 1990s Phineas Gage and the frontal lobe Paul Broca and M. Leborgne’s brain Learning localization via pathological observations Wilder Penfield and Cortical Mapping Penfield and cortical mapping PET scan and mapping Joanne Lynn MD LOCALIZATION IN NEUROLOGIC DIAGNOSIS Levels of the nervous system Central Nervous System • • • • • Cerebrum / cortex Basal ganglia Cerebellum Brainstem Spinal Cord Peripheral Nervous System • • • • Roots Plexus Peripheral nerves Neuromuscular junction • Muscle Anatomical Localization History and physical examination Can the findings be explained by: One lesion? Multiple discrete lesions? A diffuse process? What level / levels of nervous system are affected? Beware false localizing signs, non-physiologic (functional) disease Levels of the nervous system Let’s start at the top with the cerebral cortex Important cortical areas for clinical diagnosis Cortical Functions - Language Aphasia/dysphasia – true language disturbance with errors of grammar, word production and / or comprehension This should be differentiated from disorders of speech production: Dysarthria – disorder of articulation due to the motor function underlying speech in which language is intact Dysphonia – impairment of the ability to produce sounds due to disorder of larynx or its innervation Aphonia – total loss of voice often due to bilateral recurrent laryngeal nerve injury, resection of larynx, etc. Cerebral Dominance / Lateralization 90% of the population is definitely right handed 99% of these are strongly left hemisphere dominant for language The 10% who are left-handed are different: 80% have some degree of language representation in both hemispheres Language testing Handedness Spontaneous speech: fluency, articulation, prosody, grammar, errors (paraphasias) Comprehension: single words, yes/no questions, complex commands Repetition Naming Reading/ Writing Broca’s aphasia Lesion in dominant inferior frontal gyrus Nonfluent aphasia Comprehension good Associated contralateral hemiparesis if nearby motor strip is involved http://www.google.com/imgres?imgurl=http://www-rohan.sdsu.edu/~ Wernicke’s aphasia Lesion in dominant superior temporal gyrus Speech fluent but nonsensical Poor auditory comprehension Poor awareness of problem Aphasia- Localization Vascular supply related to aphasias Frontal Lobe Hemiparesis Personality changes: Apathy, euphoria, jocularity, irritability, social inappropriateness Decreased executive functions Frontal micturation area – 2nd frontal gyrus – may develop urinary incontinence (as in NPH) Disorders: tumors, head trauma, hydrocephalus Tests: alternating sequences alternating motor patterns ` fist-palm-side test Descending Corticospinal and Corticobulbar tracts Alternating sequencing tasks – impaired in extensive frontal lobe disease Frontal lobe function: alternating sequences: Fist, side, palm Temporal Lobe Bilateral lesions: profound memory loss Dominant side: decreased verbal learning Nondominant side: decreased visual learning Visual field defects Most common site of seizure focus for partial seizures Temporal lobe and memory Parietal Lobe Either side: disturbance of sensation on the opposite side of the body Central sensory functions: Decreased 2 point discrimination Sensory inattention / extinction Sensory agnosia: Astereognosis Agraphesthesia Parietal Lobe Pain pathways – Spinothalamic tract to thalamus To parietal lobe Parietal Lobe Vibration and proprioception input Posterior or dorsal columns To Nucleus gracilis and cuneatus To Thalamus To Parietal lobe Parietal Lobe Syndromes Dominant hemisphere: Apraxias – inability to carry out an action in response to verbal command in the absence of problems with comprehension, impairment of motor function. Gerstmann’s syndrome: impaired calculation, left-right confusion, finger agnosia, dysgraphia Nondominant hemisphere: Neglect of opposite side Impaired constructional ability Neglect – parietal lobe dysfunction Occipital lobe http://cerebrabraintech.com/alexia-turbobrain-technology/understanding-the-human-brain Visual system Optic nerves, tracts, Radiations and cortex And associated visual field defects Laughter is the best medicine Basal ganglia A whole set of clinical neurologic problems may be associated with lesions of the basal ganglia. Clues to this localization include: Some types of tremor Rigidity Hypokinesia or hyperkinesia Postural disturbances Many movement disorders caused by dysfunction in this system are not associated with dramatic abnormalities on routine imaging – so the clinician must recognize typical syndromes by clinical features on history and exam. Cerebellum Cerebellum – clinical signs Incoordination Dysdiadochokinesis Terminal dysmetria Intention tremor Truncal and appendicular ataxia Hypotonia Rebound Oculomotor abnormalities Dysarthria commons.wikimedia.org Ataxia Incoordination or clumsiness of movement not caused by weakness or sensory loss – rather caused by a disordered contractions of paired agonist and antagonist muscles The word ataxia derives from Greek words meaning ‘lack of order’ Localization: True ataxia is Cerebellar Sometimes people speak of Vestibular ataxia or Sensory (proprioceptive) ataxia because they are also associated with staggering gait/ loss of balance So beware that this is a word that may mean different things to different speakers Cerebellar modulation Of descending Corticospinal tract Brainstem level localization Brainstem – Clues to Brainstem Localization Grouped cranial nerve findings Brainstem site Site within skull Generalized disorder of nerve, NMJ Divergent eye movements with diplopia Vertigo Discrepancies in lateralization of motor or sensory deficits – alternating sensory or motor findings Look for well-defined syndromes – like brainstem strokes Brainstem wiring for eye movements Joanne Lynn MD FACIAL PALSIES – PLEASE LOCALIZE AS UPPER VS. LOWER MOTOR NEURON LESIONS Facial palsy on the right…. Left facial palsy Woman with a peripheral facial palsy – note that the Left side of the forehead does not wrinkle while the right does. Brainstem stroke syndromes and localization Midbrain stroke syndromes Laughter is the best medicine Spinal Cord Simplified spinal cord for clinical case analysis Spinal cord syndromes Complete transverse lesion Hemisection (BrownSequard) Posterior column loss Anterior spinal syndrome Central cord syndrome Remember crossing of pain and temperature fibers in cord UMN vs LMN signs Upper motor neuron signs: Increased tone spasticity Hyperreflexia Extensor plantar response Lower motor neuron signs: Decreased tone Hyporeflexia Flexor plantar response Muscle atrophy, fasciculations Atrophy of Interossei muscles Atrophy is more prominent with weakness of LMN etiology Reflexes Myotatic stretch reflexes Monosynaptic reflex: stretch muscle, stimulate Ia sensory afferent, stimulate alpha motorneuron Ankle S1, S2 Patellar L3, L4 Biceps C5, C6 Triceps C7, C8 Reflex arc Stupid Neurology cartoon Come back for Part 2 – It is much shorter! Thank you for completing this module Questions? Contact me at: Joanne.Lynn@osumc.edu Survey We would appreciate your feedback on this module. Click on the button below to complete a brief survey. Your responses and comments will be shared with the module’s author, the LSI EdTech team, and LSI curriculum leaders. We will use your feedback to improve future versions of the module. The survey is both optional and anonymous and should take less than 5 minutes to complete. Survey