Histo Chapter 23 [4-20
advertisement

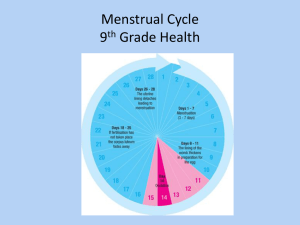
Histo Chapter 23: The Female Reproductive Sytem (pages 845-863) During each menstrual cycle, the ovary undergoes cyclic changes that have 2 phases: the follicular and luteal phases – graph page 846 - - Ovulation happens between the 2 phases Folllicular phase – starts with the development of a small # of primary follicles, directed by FSH and LH o Selection of dominant follicles happens by days 5-7 of the menstrual cycle o During the first 8-10 days, FSH is the main hormone that influences growth of the follicles It stimulates the granulosa and thecal cells, which start to secrete steroid hormones, mainly estrogens, into the follicular lumen As the dominant follicles make more estrogen, it inhibits the FSH Eventually, estrogen levels get high enough, that the follicle can grow and develop without FSH signals o Later in the follicular phase, before ovulation, progesterone levels start to increase in response to LH At this point, the estrogens inhibit any more making of FSH o Then, the LH levels surge, inducing ovulation This is accompanied by a smaller increase in FSH 34-36 hours after the start of the LH surge, or about 10-12 hours after the peak of the LH surge Luteal phase – starts immediately after ovulation o Here, the granulosa & thecal cells of the ruptured follicle change into the corpus luteum o The corpus luteum makes lots of estrogen and progesterone Both hormones, but mainly progesterone, cause the endometrium to start its secretory phase, which is done to prepare the uterus for implantation o LH is responsible for the development and maintenance of the corpus luteum during the menstrual cycle o If fertilization doesn’t happen, the corpus luteum degenerates within a few days, as the hormone levels drop o If fertilization does happen, the corpus luteum is maintained and continues to make progesterone and estrogens Fallopian (Uterine tubes) – paired tubes that extend from both sides of the uterus towards the ovaries - - The fallopian tubes transport the ovum from the ovary to the uterus, and provide the environment needed for fertilization and beginning of the development of the zygote up to the morula stage There’s 4 segments of the fallopian tubes: o Infundibulum – funnel shaped part of the fallopian tube next to the ovary, that is open to the peritoneal cavity The infundibulum has fimbriae that extend towards the ovary o - - Ampulla – next part, the longest part of the fallopian tubes (2/3 of it) The ampulla is where fertilization happens o Isthmus – part next to the uterus o Uterine (intramural) part – in the uterine wall, and opens into the uterine cavity The wall of the fallopian tube is made of 3 layers o Serosa (peritoneum) – outermost layer of the fallopian tube ,made of mesothelium and a thin layer of connective tissue o Muscularis – middle muscular layer o Mucosa – inner lining of the fallopian tube, made of columnar epithelium that can be either ciliated or nonciliated Ciliated columnar epithelium – there’s more of it in the infidibulum and ampulla Nonciliated peg cells – secretory cells that make fluid that provides nutrition to the ovum These epithelial cells undergo cycles of hypertrophy during the follicular phase, & atrophy during the luteal phase in response to hormones, mainly estrogen The ratio of ciliated to nonciliated cells also changes during the hormone cycle Estrogen stimulates cilia making, and progesterone increases the # of secretory cells The fallopian tubes start movements just before ovulation, and the fimbriae get close to the ovary near where rupture will happen When the oocytes is released, the ciliated cells in the infundibulum sweep it towards the opening of the fallopian tube, that way it doesn’t go into the peritoneal cavity The oocyte is transported along the uterine tube by peristalsis and cilia movement Fertilization usually happens in the ampulla, near its junction with the isthmus The ovum stays in the fallopian tube for about 3 days, before it enters the uterine cavity Things like inflammation, intrauterine devices, surgical manipulation, and tubal ligation, can all predispose to ectopic pregnancy o Most ectopic pregnancies happen in the fallopian tubes (98%), called tubal pregnancies The uterus will receive the morula from the fallopian tubes, and the rest of the development of the fetus happens in the uterus - In the pelvis, the uterus is between the bladder and the rectum In anatomy, the uterus is divided into 2 regions: the body and the cervix o Body (corpus) – large upper part of the uterus The part of the body above where the fallopian tubes attach, is called the fundus o Cervix – lower part of the uterus It’s separated from the body by the isthmus The lumen of the cervix is called the cervical canal, and has a constricted opening at each of its ends The internal os is the opening to the uterine body - - - - - The external os is the opening to the vagina The uterine wall is made of 3 layers – page 848 o Endometrium – innermost lining made of mucosa that meets the lumen o Myometrium – thick muscular layer, continuous with the muscle of the fallopian tubes and vagina o Perimetrium – outer serous (visceral peritoneum) layer covering the uterus The perimetrium is continuous with the pelvic and abdominal peritoneum, and consists of the mesothelium and a thin layer of loose connective tissue The perimetrium covers the entire posterior surface of the uterus, but only part of the anterior Both the myometrium and endometrium undergo cyclic changes each month to prepare the uterus for implantation, called the menstrual cycle o If the embryo implants, the cycle stops, and both layers undergo lots of growth and differentiation The myometrium is the thickest layer of the uterus, and has 3 layers of smooth muscle o The middle muscle layer has lots of large venous plexuses and lymphatics, called the stratum vasculare o The middle muscle layer is the thickest, and connects to smooth muscle bundles in the inner and outer layers o All 3 muscle layers work together as a functional syncytium o During pregnancy, much of the enlargement of the uterus is due to hypertrophy of these smooth muscle cells The smooth muscle can also develop new fibers through division of existing muscle cells, and differentiation of undifferentiated mesenchymal cells o As pregnancy goes on, the uterine wall gets progressively thinner as it stretches because of growth of the fetus o After birth, the uterus goes back to close to its original size, but the uterine cavity will stay larger, and the muscular wall remains thicker than before pregnancy The cervix has less smooth muscle and more connective tissue (elastic fibers) than the body of the uterus During the menstrual cycle, the endometrium will get more secretory with maturation of the follicles, and then at the end the endometrium will be partially destroyed and will slough, which is accompanied by bleeding from the mucosal vessels o This discharge of tissue and blood from the vagina lasts for 3-5 days, and is called menstruation (menstrual flow) o The menstrual cycle begins on the day menstrual flow begins 2 layers of the endometrium: o Stratum functionale (aka functional layer) – thick part of the endometrium that is the layer that proliferates and differentiates, and then gets sloughed off at menstruation o Stratum basale (aka basal layer) – retained during menstruation, and is the source for regenerating the functional layer - - The lining of the endometrium is a simple columnar epithelium with a mix of secretory and ciliated cells o The surface epithelium invaginates into the underlying lamina propria, called the endometrial stroma, to form the uterine glands Uterine glands have fewer ciliated cells The blood vessels of the endometrium also proliferate & degenerate during the menstrual cycle o The uterine artery gives off arcuate arteries that anastomose in the myometrium o Radial arteries branch from the arcuate, and enter the basal layer of the endometrium, where they give off small straight arteries to supply it – page 849 o The main branch fo the radial artery continues upward and becomes very coiled, which is why it’s called the spiral artery o Spiral arteris give off lots of arterioles that anastomose to form a capillary bed o The straight arteries and proximal part of the spiral arteries don’t change during the menstrual cycle o The distal part of the spiral arteries will degenerate and regenerate with each menstrual cycle The menstrual cycle is a cycle of changes in the functional layer of the endometrium - - - The menstrual cycle is controlled by FSH and LH, which regulate release of female steroids The cycle normally repeats every 28 days There’s 3 phases of the menstrual cycle: o Proliferative phase – happens along with follicle maturation, and is influenced by ovary estrogen release o Secretory phase – happens along with the corpus luteum, and mainly influenced by progesterone release o Menstrual phase – happens when hormone release is decreased as the corpus luteum degenerates At the end of the menstrual phase, the endometrium is a thin band of connective tissue, with basal parts of the uterine glands and the lower parts of the spiral arteries o This layer is called the stratum basale, and the stratum functionale had just been sloughed off Proliferative phase – page 851 is a pic of each phase o Estrogen causes stromal, endothelial, and epithelial cells in the stratum basal to proliferate rapidly o Epithelial cells in the basal part of the glands reconstitute the glands, and migrate to cover the endometrial surface o Stromal cells proliferate and secrete collagen and ground substance (proteoglycans) o Spiral arteries lengthen as the endometrium is reestablished o The proliferative phase continues until 1 day after ovulation (ovulation is about day 14 of a 28 day cycle) o - - - - At the end of the proliferative phase, the endometrium is thicker, the glands have narrow lumens and look wavy, and there’s glycogen in the epithelial cells Secretory phase: o Progesterone causes the endometrium to become even thicker and edematous o The glands enlarge and fill with secretory fluid, and look cork-screw shaped This fluid is mucus-like, and has lots of nutrients, especially glycogen, which will be needed to support the fetus o In the secretory phase, there is less mitoses than in the proliferative, and instead you see more hypertrophy of the epithelial cells o The spiral arteries lengthen more and get more colied o Progesterone and estrogen can turn the stromal cells into decidual cells The stimulus for this is implantation of the blastocyst The decidual cells are large pale cells rich in glycogen o The corpus luteum makes hormones for about 10 days if fertilization doesn’t happen Menstrual phase: o As hormones from the corpus luteum decrease, the blood supply to the stratum functionale changes o Periodic contractions of the walls of the spiral arteries cause the stratum functionale to become ischemic The glands stop secreting, and the endometrium shrinks, while the stroma becomes less edematous After about 2 days, contraction becomes so frequent and prolonged that blood flow is only brief, which causes disruption of the surface epithelium and rupture of the blood vessels When the spiral arteries close off, blood can still flow into the stratum basale, but not into the stratum functionale o You then get vaginal discharge, which has blood, uterine fluid, and sloughed stromal and epithelial cells from the stratum functional o As this tissue separates from the endometrium, the torn ends of veins, arteries, and glands are exposed, seeping out blood o Desquamation will continue until only the stratum basale remains o During this menstrual flow, clotting of blood is inhibited o The menstrual flow usually lasts about 5 days o The stratum basale is maintained by blood through the straight arteries o When bleeding stops, the epithelial cells rapidly proliferate dn migrate to restore the surface epithelium, and you start the proliferative phase of the next cycle Anovulatory cycle – there was no ovulation o When this happens, there’s no corpus luteum, so no progesterone is made o Without progesterone, the endometrium doesn’t go into the secretory phase, and so just proliferates until menstruation o In infertility, you can biopsy the endometrium to look for anovulatory cycles If fertilization and implantation happen, the endometrium won’t decline again until after birth o As the blastocyst embeds in the uterine mucosa in the early 2nd week, cells in the chorion of the developing placenta start to secrete hCG, which maintains the corpus luteum and stimulates it to keep making progesterone and estrogens, preventing decline of the endometrium In the fallopian tubes, the fertilized zygote undergoes cleavage, followed by mitotic divisions, without cell growth, causing a rapid increase in the # of cells in the embryo - - At first, the embryo is controlled by mom things that accumulated in the ovum during oogenesis Later, development is controlled by activation of the embryonic genome, which codes for growth factors and other stuff to progress to a blastocyst The cell mass resulting from all the mitosis is called a morula, and each individual cell in it is called a blastomere At the 3rd day after fertilization, the morula enters the uterine cavity In the uterus, the morula hangs out for a day and keeps doing cell division and development This development forms a blastocyst, made of a hollow sphere of cells with a central clump of cells called inner cell mass – page 853 is pics o The inner cell mass gives rise to the tissues of the embryo o The outer surrounding layer of cells is called the outer cell mass, and will form the trophoblast, and then the placenta Fluid passes inward during this to form a fluid filled cavity called the blastocyst cavity o This event defines the beginning of the blastocyst As the blastocyst hangs out free for 1-2 days, it loses the zona pellucida o Out this point, the outer cell mas is now called the trophoblast, and the inner cell mas is called the embryoblast Implantation happens when the uterus is receptive for implantation of the blastocyst, called the implantation window - This is a short time period, determined by progesterone and estrogen effects on the endometrium The implantation window is from day 6 after the LH surge, and ends by day 10 Antiprogesterone drugs like mifepristone will block progesterone receptors on the endometrium, preventing its effects and therefore conditions for implantation As contact is made with the uterine wall by the trophoblastic cells, the trophoblast rapidly proliferates and starts to invade the endometrium o The invading trophoblast differentiates into the syncytiotrophoblast and the cytotrophoblast o Cytotrophoblast – mitotically active inner cell layer producing cells that fuse with the syncytiotrohpoblast o Syncytiotrophoblast – outer erosive layer that is not mitotically active, and is made of a multinucleate cytoplasmic mass It invades the epithelium and underlying stroma of the endometrium - It has lots of golgi and ER to secrete progesterone, estrogens, and hCG The trophoblast makes the blastocyst get entirely embedded within the endometrium at about the 11th day of development During pregnancy, the part of the endometrium that changes morphologically is called the decidua - - The decidua is shed with the placenta at birth The decidua includes all but the deepest layer of the endometrium – page 854 The stromal cells differentiate into large round decidual cells The uterine glands enlarge and get more coiled during early pregnancy, and then get thin and flat as the fetus grows and fills the uterus lumen 3 regions of the decidua: o Decidua basalis – part of the endometrium that underlies the implantation site o Decidua capsularis – thin part of the endometrium that lies between the implantation site and the uterine lumen o Decidua parietalis – rest of the endometrium and uterus By the end of the 3rd month, the fetus grows enough that the overlying decidua capsularis fuses with the decidua parietalis of the opposite wall, obliterating the uterine cavity By the 13th day, an extraembryonic space called the chorionic cavity is established o The cells that form the outer boundary of the chorionic cavity are the syncytiotrophoblast, cytotrophoblast, and extraembryonic somatic mesoderm, and they’re collectively called the chorion o The innermost membranes enveloping the embryo are called the amnion The endometrium of the cervix is different from the rest of the uterus: - It has large branched glands and lacks spiral arteries The cervical mucosa doesn’t change much in thickness during the menstrual cycle, and isn’t sloughed during menstruation During the menstrual cycle, cervical glands change the amount of mucus they secrete, in order to help transport the sperm in the cervical canal o This is controlled by ovarian hormones o At midcycle, the amount of mucus made increases a lot o This mucus is less viscous, and provides a more favorable environment for sperm migration At other times in the cycle, cervical mucus restricts passage of sperm into the uterus o Blocking the openings of the cervical mucosal glands causes them to retain their secretions, forming a dilated cyst in the cervix called Nabothian cysts This is common, and only clinically significant if lots of cysts causes the cervix to enlarge a lot The part of the cervix that projects into the vagina is called the ectocervix, and is covered with a stratified squamous epithelium – page 855 The mucus secreting columnar epithelium of the cervical canal is called the endocervix There’s an abrupt transition between the squamous epithelium and the columnar epithelium, called the transformation zone - - Before puberty and after menopause, the transformation zone is in the cervical canal During reproductive age, the transformation zone is just outside the external os Metaplastic changes in the transformation zone are precancerous lesions of the cervix Metaplasia here is reversible change of the epithelium in response to persistent injury to it from chronic infections o It happens from reprogramming of the epithelial stem cells, that will then differentiate along a new cell lineage In the cervical canal (endocervix), the metaplasia is seen as a replacement of the simple columnar epithelium with fully mature stratified squamous epihtleium – page 856 The cervical epithelial cells are constantly exfoliated inot the vagina PAP smears are used here for screening and diagnosis of possible cancerous lesions of the cervix The developing fetus is maintained by the placenta, which develops from both mom and fetal tissues - The fetal part comes from the chorion, and the mom part is formed by the decidua basalis These 2 parts do the exchange of things between mom and the fetus The uteroplacental circulatory system starts to develop around day 9, when vascular spaces called trophoblastic lacunae develop in the syncytiotrophoblast Mom capillaries develop sinusoids, which anastomose with the trophoblastic lacunae The pressure between the arteries and veins that communicate with the lacunae cause a flow going from the arteries to the veins, establishing a primitive uteroplacental circulation Transfer of nutrients from mom to the embryo is seen as many pinocytotic vesicles in the syncytiotrohpoblast Then, the cytotrophoblast proliferates, the chorionic mesoderm grows, and blood vessels develop more, to form villi- page 857 o Primary chorionic villi – formed by the rapidly proliferating cytotrophoblast, and sends cords (masses of cells) into the blood filled trophoblastic lacunae in the syncytiotrophoblast Primary villi show up between days 11-13 o Secondary chorionic villi – made of a central core of mesenchyme surrounded by an inner layer of cytotrophoblast and an outer layer of syncytiotrophoblast They develop at about day 16 when the primary chorionic villi get invaded by loose connective tissue from the chorionic mesenchyme The secondary villi cover the whole surface of the chorionic sac o - - - - - - - Tertiary chorionic villi – formed by the end of the 3rd week, as the secondary villi get vascularized by blood vessels that developed in their connective tissue cores As the tertiary villi are forming, cytotrophoblstic cells in the villi continue to grow out through the syncytiotrohpoblast o When they meet the mom endometrium, they grow laterally and meet other processes growing from neighboring villi o This forms a thin layer of cytotrohpoblstic cells called the trophoblastic shell, around the syncytiotrophoblast o The trophoblastic shell is interrupted only at places where mom vessels communicate with the intervillous spaces o Future growth of the placenta is done by growth of the trophoblastic shell The connective tissue stroma of the villi has mesenchymal cells, reticular cells, fibroblasts, myofibroblsts, smooth muscle, macrophage, and antigen presenting cells of the placenta (called Hofbauer cells) o Fetal placental APCs are villous macrophage that came from the fetus, and carry out placental immune responses Blood starts to flow through the embryonic cardiovascular system and the villi at about 21 days o Exchange of nutrients and wastes happens at the intervillous spaces During the first 8 weeks, villi cover the entire chorionic surface, but as growth continues, villi on the decidua capsularis start to degenerate, producing a smooth avascular surface called the chorion leave The villi next to the decidua basalis rapidly increase in size and # and get highly branched o This area of the chorion is the fetal part of the placenta, and is called the chorio frondosum (or villous chorion) o The layer of the placenta that the villi project from is called the chorionic plate The chorion frondosum rapidly growths at the 4th-5th month o At this point, the fetal part fo the placenta is divided by the placental (decidual) septa into many areas called cotyledons o Placental septa form the boundaries of the cotyledons The placental septa don’t fuse with the chorionic plate, so mom blood can circulate easily between tehm Cotyledons look like bulging areas on the mom side of the basal plate The decidua basalis forms a layer called the basal plate, that is the mom part of the placenta o Vessels in this part of the endometrium supply blood to the intervillous spaces Except for rare ruptures of the capillary walls, fetal blood and mom blood don’t mix o These ruptures are more common at delivery o Fetal and mom blood are separated by the placental barrier – page 858 o Starting at the 4th month, the placental barrier gets thin to allow exchange of stuff This is caused by degeneration of the inner cytotrophoblast layer The placenta is the site of exchange of gases and metabolites between mom & fetal circulations o Fetal blood enters the placenta through 2 umbilical arteries, which branch a lot – p 859 o These branches go into the villi to form capillary networks with the intervillous psaces o - - Gases and metabolic stuff are exchanged across the thin fetal layers that separate the 2 bloodstreams at these capillaries Antibodies can also cross this layer to help the baby o Fetal blood then returns through veins that converge to form the umbilical vein o Mom blood is supplied to the placenta through lots of endometrial arteries (spiral arteries) that penetrate the basal plate Blood from these spiral arteries flows into the base of the intervillous spaces The blood pressure in the spiral arteries is much higher than in the intervillous spaces This blood then passes over the villi, where exchange of materials happens The placenta does not block toxins mom takes in from getting to the baby So mom blood goes to the intervillous spaces, and the pressure moves blood into them, where diffusion can then move stuff into the villi Before the placenta is established, the growth of the embryo is supported by things made by the trophoblast o the syncytiotrophpoblasts makes glycogen, cholesterol, fatty acids, & other nutrients The placenta is also an endocrine organ that makes steroids and hormones, and prostaglandins that are big in causing labor o These are also made in the syncytiotrophoblast o Progesterone and estrogen here is crucial to maintain the pregnancy As pregnancy proceeds, the placenta takes over as the major thing secreting progesterone and estrogen The placenta makes enough progesterone by the end of the 8th week to maintain pregnancy if the corpus luteum is surgically removed or fails to function To make estrogen, the fetal adrenal cortex provides the precursors to make it The placenta lacks the enzymes to make estrogen So monitoring estrogen production during pregnancy can be used as a marker of fetal development o Other hormones the placenta makes: Human chorionic gonadotropin (hCG) – needed for implantation and maintenance of pregnancy hCG starts being made around day 6, even before the syncytiotrophoblast is formed hCG is very similar to LH o hCG maintains the corpus luteum during early pregnancy hCG is also similar to TSH, which can cause hyperthyroidism when this stuff crosses over to mom and induces the thyroid to make T4 (GNC!) Early pregnancy tests measure for hCG hCG is also measure to see how viable the pregnancy is trophoblast disease and ectopic pregnancies will increase the hCG - - Human chorionic somatomammotropin (hCS, aka human placental lactogen, hPL) hCS is very similar to GH hCS is made by the syncytiotrophoblast, and promotes growth, regulates glucose metabolism, and stimulates mammary duct proliferation in mom’s breasts IGF’s are made by the cytotrophoblast for proliferation and differentiation Endothelial growth factor (EGF) At 4-5 weeks, EGF is made by the cytotrophoblast and stimulates proliferation of the trophoblast At 6-12 weeks, synctiotrophoblasts make the EGF to maintain the differentiated trophoblasts Relaxin – made by decidual cells to relax the cervix and pelvic ligaments to prepare for birth Leptin – made by the syncytiotrophoblst to regulate mom’s storage of nutrients, and helps move them to the baby Leptin is especially made in the last month of gestation After birth, the uterus continues to contract, causing the placenta to separate from the uterine wall and be delivered, usually about 30 minutes after birth o The entire fetal part of the placenta, fetal membranes, and projections of decidual tissue, get released o One of the most common problems of labor is abnormal placentation (detachment) If decidual tissue is disrupted during implantation, the placenta invades deep into the uterine wall This can cause 3 things: placenta accrete, placenta increta, or placenta percreta Placenta accreta – happens when the placenta attaches too deeply into the uterine wall, doesn’t penetrate the myometrium ¾ of placenta detachment problems Placenta increta – when placenta gets into the myometrium Placenta percreta – when the placenta went through the whole uterine wall and attaches to other organs, like the bladder, rectum, etc. Placenta increta or percreta often need treated with a hysterectomy After the placenta is delivered, the endometrial glands and stroma of the decidua basalis regenerate o Endometrial regeneration is complete by the end of the 3rd week after birth, except at the placental site, which needs another 3 weeks o During the 1st week after delivery, remnants of the decidua are shed and form the redbrown uterine discharge called lochia The vagina is a fibromuscular tube that joins the internal female reproductive organs to the external environment - - - - - It extends from the cervix to the vestibule (area between the labia minora) In a virgin, the opening inot the vagina is surrounded by the hymen, which are folds of mucous membrane extending into the vaginal lumen o The hymen comes from the endodermal membrane that separated the developing vagina from the cavity of the urogenital sinus in embryo Layers of the vaginal wall: o Inner mucosal layer – has many folds (rugae), and is lined with stratified squamous epithelium (page 861) o Intermediate muscular layer – smooth muscle that can be divided into an outer longitudinal layer, and inner circular layer The outer layer is continuous with the uterus and much thicker than the inner layer o Outer adventitial layer – separated inot an inner dense connective tissue layer next to the muscularis, and an outer loose connective tissue layer that blends with the adventitia of the surrounding structures The inner layer has lots of elastic fibers for elasticity, and the outer layer has blood vessels and nerves The lumen of the vagina is lined by stratified squamous nonkeratinized epithelium The vaginal surface is lubricated by mucus made by the cervical glands o The vestibular glands in the vaginal vestibule also make mucus to lubricate The epithelium of the vagina also changes with the menstrual cycle o In the follicular phase, estrogen causes the epithelial cells to make and accumulate glycogen as they migrate towards the surface o Cells are continuously desquamated, but in the menstrual phase, the superficial layer of the vaginal epithelium is shed The lamina propria has a deep region that has veins that stimulate erectile tissue during sexual arousal o The lamina propria also has immune cells The vagina has few sensory nerve endings, and most of them are more clustered in the lower 1/3 of the vagina Vulva – female external genitalia - The vulva has stratified squamous epithelium Mons pubis – round prominence over the pubic symphysis formed by subcutaneous fat Labia majora – 2 large longitudinal folds of skin with muscle, hair on the outside, and sebaceous and sweat glands Labia minora – paired hairless folds that border the vestibule Clitoris – erectile tissue with 2 erectile bodies called copora cavernosa that attach to a glans clitoris, which is loaded with sensory nerves Vestibule – lined by stratified squamous epithelium, and has the Skene’s and Bartholin’s vestibular glands to secrete mucus o If the duct of the Bartholin’s gland is obstructed, it usually dialates and fills with secretion, forming a Bartholin’s cyst Pap smears - superficial epithelial cells are scraped from the mucosa & stained with Papanicolaou stain - Page 862