Katy grand rounds april 14
advertisement

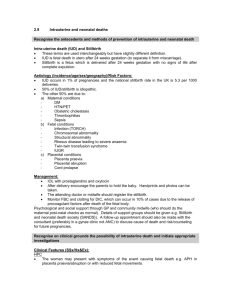
Evaluation of Stillbirth Katy Kemnetz, PGY2 Evaluation of stillbirth OBJECTIVES Objectives The participant will be able to: Identify the conditions that have been best demonstrated to cause stillbirth Evaluate a stillbirth using the most effective workup Accurately formulate an etiology for a stillbirth, when possible Employ the recmomended hospital policies for management of stillbirth Outline Definitions Causes of stillbirth Workup of stillbirth Other considerations Conclusions Evaluation of Stillbirth Definitions Definitions Spontaneous abortion Miscarriage <20 weeks gestation or <500g Intrauterine fetal demise “Stillbirth” >20 weeks gestation or >350g—state dependent ◦ 350g is 50%ile for 20 weeks gestation ◦ Illinois: >20 weeks gestation “Delivery of a fetus showing no signs of life as indicated by the absence of breathing, heart beats, pulsation of the umbilical cord, or definite movements of voluntary muscles” Does not include terminations of pregnancy or IOL for previable PPROM Evaluation of stillbirth Causes Causes of stillbirth >30 classification systems exist Important to distinguish between ◦ Underlying cause of death ◦ Mechanism of death ◦ Risk factors The National Institute of Child Health and Human Development CLASSIFICATION OF STILLBIRTH Classification of Stillbirth Eunice Kennedy Shriver workshop 2007 National Institute of Child Health and Human Development “An optimal classification system would identify the pathophysiological entity initiating the chain of events that irreversibly lead to death” Criteria for “cause” Epidemiologic data demonstrate an excess of stillbirth associated with that condition Biologic plausibility that the condition causes stillbirth Either rarely seen in association with live births or, when seen in live births, results in a significant increase in neonatal death A dose-response relationship exists ◦ The greater the “dose” of the condition, the greater the risk of fetal death Associated with evidence of fetal compromise The stillbirth likely would not have occurred if that condition had not been present Causes of stillbirth Reddy, UM et al. “Stillbirth Classification—Developing an International Consensus for Research.” Obstetrics and Gynecology, Vol 114, No 4, October 2009. Causes of stillbirth—NICHHD workshop consensus INFECTIONS Infection Associated with 10-20% of stillbirths in developed countries Higher association with preterm birth Sometimes difficult to prove causality Infection Ascending infectionamniotic fluid or fetusfetal pneumonitis Hematogenous spreadvillitis Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Mechanism of fetal death Severe maternal illness Placental infection that prevents oxygen/ nutrients from crossing to the fetus Fetal infection that causes a lethal congenital deformity Fetal infection that damages a vital organ Precipitation of preterm labor, with intrapartum fetal death Infections must be proven Signs of infection in the fetus ◦ Evidence on autopsy of extensive organ involvement Positive fetal cultures Positive maternal cultures plus chorioamnionitis/ funisitis Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Causes of IUFD: Spirochetes Organism Comment Treponema palladium Maternal disease Severe Syphilis placental dysfunction Borrelia burgdorferi Lyme disease Tick borne; not a common cause of stillbirth Borrelia recurrentis Relapsing fever Tick borne; common in the Western US; rare cause of stillbirth Borrelia duttonii Relapsing fever Tick borne; sub-Saharan Africa; important cause of stillbirth Leptospira interrogans Leptospirosis Uncommon Major cause of stillbirth when maternal prevalence is high Protozoa Organism Maternal disease Comment Trypanosoma brucei Trypanasomiasis Tsetse fly Trypanosoma cruzi Chagas disease Kissing bug Plasmodium falciparum Malaria Common in endemic areas Plasmodium vivax Malaria Toxoplosmosis gondii Toxoplasmosis Severe placental dysfunction Mosquitoes Rare Viruses Organism Maternal disease Comment Parvovirus B19 Erythema infectiosum Likely the most common viral etiologic agent Coxsackie A and B Various May be important Echovirus Various Importance unknown Enterovirus Various Importance unknown Hepatits E virus Fulminant hepatic failure Especially in endemic areas Poliovirus Polio Historic cause Varicella zoster Causes lethal Rubella fetal anomalies Mumps Chickenpox Rare cause German measles Rare in developed countries Parotitis Rare in developed countries Rubeola Measles Rare in developed countries Cytomegalovirus Asymptomatic Case reports HIV AIDS Not likely causative Influenza Respiratory tract infection Severe maternal illness Bacteria Organism Maternal disease Comment Asymptomatic Probably the most common organism assoc with stillbirth Asymptomatic Common cause of stillbirth Klebsiella Asymptomatic Common cause of stillbirth Enterococcus Asymptomatic Ureaplasma, mycoplasma Asymptomatic E. Coli GBS Damage to vital organs (brain, heart) Chlamydia trachomatis Severe placental Listeriosis dysfunction Pelvic infection Neisseria gonorrhoeae Pelvic infection Suggested cause—case reports Candida albicans Thrush; vaginitis Confirmed in case reports Listeria monocytogenes Transmitted transplacentally Suggested cause—case reports Goldenberg RL, Thompson C. The infectious origins of stillbirth. Am J Obstet Gynecol 2003;189:861–73 Causes of stillbirth—NICHHD workshop consensus MATERNAL MEDICAL CONDITIONS Hypertensive disorders Condition Estimated stillbirth rate per 1000 births in patients with the condition All pregnancies 6-7 Chronic hypertension 5-25 Superimposed preeclampsia 52 Gestational hypertension and mild preeclampsia 9 Severe preeclampsia 21 Eclampsia 18-48 HELLP syndrome 51 Simpson, LL. Maternal medical disease: Risk of Antepartum Fetal Death. Semin Perinatol, 2002, 26, 47. Hypertensive disorders Mechanism of fetal demise: To consider cause of death: Placental insufficiency ◦ IUGR ◦ Abruption If it progresses to eclampsia If it is associated with placental abruption or fetal growth restriction Diabetes Condition Estimated stillbirth rate per 1000 births in patients with the condition All pregnancies 6-7 Gestational diabetes 5-10 Type 1 diabetes 6-10 Type 2 diabetes 35 Simpson, LL. Maternal medical disease: Risk of Antepartum Fetal Death. Semin Perinatol, 2002, 26, 47. Diabetes Mechanism of fetal demise: To consider cause of death: Congenital abnormality Placental dysfunction Obstructed labor and intrapartum death Macrosomia ◦ Fetal hyperglycemiafetal insulin productionexcessive fetal growthmetabolic acidosis Signs of intrauterine or intrapartum asphyxia LGA fetus SGA fetus Severe malformation Placenta demonstrates characteristic histologic findings ◦ Large edematous villi ◦ Increased prominence of cytotrophoblasts Thyroid/renal disorders Condition Estimated stillbirth rate per 1000 births in patients with the condition All pregnancies 6-7 Stable treated hyperthyroidism 0-36 Uncontrolled thyrotoxicosis 100-156 Subclinical hypothyroidism 0-15 Overt hypothyrodism 15-125 SLE 40-150 Mild chronic renal disease 15 Moderate and severe chronic renal disease 32-200 Cholestasis of pregnancy 12-30 Simpson, LL. Maternal medical disease: Risk of Antepartum Fetal Death. Semin Perinatol, 2002, 26, 47. Thyroid/renal disorders Thyroid disorders Graves disease, where thyroidstimulating hormone receptor antibody causes fetal toxicosis Untreated thyroid disorders Renal disorders Linear relationship between maternal creatinine and risk of fetal demise Systemic Lupus Erythematosus Stillbirth rates are higher in the presence of HTN, nephritis, or APL Circulating auto-antibodies, anti-Ro, anti-La Congenital heart block, hydrops Maternal medical conditions Risk is a continuum Reddy, UM et al, 2009 Causes of stillbirth—NICHHD workshop consensus THROMBOPHILIAS Thrombophilias Antiphospholipid syndrome Inflammation, thrombosis, and infarction in the placenta Clear histopathological or clinical evidence of placental insufficiency Inherited thrombophilias Thrombophilias should only be considered as the cause of Factor Leiden mutation, Two V large prospective antithrombin III deficincy, Thrombophilias are cohort studies found no stillbirth with: common in healthy association between factor prothrombin mutation, •Evidence ofgene placental women with normal V Leiden mutation andprotein S protein C deficiency, insufficiency such as fetal outcomes pregnancy loss or placental deficiency growth restriction or infarction insufficiency and Placental infarction and •Recurrent fetal loss thrombosis Causes of stillbirth—NICHHD workshop consensus ALLOIMMUNIZATION Alloimmunization Red cell alloimmunization Platelet alloimmunization Anti-Rhesus D, anti-Rhesus C, anti-Kell Must have a positive indirect Coombs test Antibody titers more than 1:16 (or 1:8 for anti-Kell) Evidence of fetal anemia with hydrops Evidence of fetal extramedullary hematopoeisis HPA-1a, HPA-5a, HPA-4 Maternal antibodies against paternal and fetal platelet antigens Parental platelet incompatibility for the pertinent antigen Fetal thrombocytopenia Massive intracranial hemorrhage Causes of stillbirth—NICHHD workshop consensus CONGENITAL MALFORMATIONS CHROMOSOMAL ABNORMALITIES Criteria Epidemiologic data demonstrating an excess of intrauterine mortality Seen rarely in liveborn neonates When seen in liveborn neonates, it frequently results in neonatal death Biologic plausibility that it can result in death Congenital malformations Cause of death Stillbirth cases, % (out of total 2211 assessed) Trisomy 21 1.53 Jugulolymphatic obstruction 1.45 Turner syndrome 1.09 Twin-twin transfusion syndrome 1.09 Anencephaly 1.0 Trisomy 18 0.81 Amnion disruption sequence 0.59 Lower mesodermal defects 0.50 Idiopathic nonimmune fetal hydrops 0.50 Trisomy 13 0.41 Reddy, UM et al. “Stillbirth Classification—Developing an International Consensus for Research.” Obstetrics and Gynecology, Vol 114, No 4, October 2009. Chromosomal abnormalities Incidence Cytogenetic abnormalities account for 6-13% of all stillbirths This may be higher because 4050% attempted karyotypes fail to grow 23% monosomy X, 23% trisomy 21, 21% trisomy 18, 8% trisomy 13 Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Chromosomal abnormalities Autosomal recessive disorders Alpha thalessemia, Smith Lemli Opitz Phenotype in lethal cases may differ from live cases Autosomal dominant disorders Skeletal dysplasias More often spontaneous mutations Firestein: Kelley’s Textbook of Rheumatology, 9th ed. Saunders 2012 Causes of stillbirth—NICHHD workshop consensus FETOMATERNAL HEMORRHAGE Fetomaternal hemorrhage The cause 4% of all stillbirths Risk factors: ◦ ◦ ◦ ◦ Placental abruption Abdominal trauma Multiple gestation Abnormal fetal testing Fetomaternal hemorrhage Risk of stillbirth depends on ◦ Amount of hemorrhage ◦ Acute/chronic ◦ Gestational age A threshold of 20 mL/kg of fetal bleeding is associated with increased risk of stillbirth Autopsy confirmation of fetal anemia and hypoxia Causes of stillbirth—NICHHD workshop consensus PLACENTAL CAUSES Placental causes Placenta previa, vasa previa, neoplasms Placental abruption has 8.9 relative risk of stillbirth ◦ May be considered the cause of death if >30% of the placenta shows signs of abruption Reddy, UM et al, 2009 Placental causes Any disease that causes an SGA placenta may result in stillbirth ◦ <5% expected weight for gestational age ◦ Preeclampsia, DM, HTN, renal, chronic infections Any disease that causes an LGA placenta may result in stillbirth ◦ >95% expected weight for gestational age ◦ Hydrops fetalis, DM, syphilis Stillbirth classification—NICHHD workshop consensus UMBILICAL CORD PATHOLOGY Umbilical cord pathology Account for 3.4-15% of stillbirths Velamentous insertion ◦ If it leads to a vasa previa or bleeding during labor Umbilical cord prolapse ◦ Associated with prematurity, malpresentation, mutiparity, obstetric manipulation Umbilical cord occlusion ◦ Cord prolapse, entanglement (mono-mono twins) ◦ Torsion ◦ Rupture, strictures, hematomas Velamentous insertion Umbilical cord pathology Nuchal cord Isolated ofpregnancies a relevant ◦•Exclude Occurs in up toother 30% finding of normal nuchal cord or a true risk of stillbirth in ◦ Not associated with an increased causes of stillbirth knot at the time of study of 14,000 deliveries delivery is insufficient •Find of hypoxia True knotevidence evidence that cord ◦and Also common in live births cord occlusion on accident is the cause of ◦ Grooving of the cord, constriction of the umbilical stillbirth postmortem examination vessels, edema, congestion, thrombosisrequired to claim it is the etiology Stillbirth classification—NICHHD workshop consensus MULTIFETAL GESTATION Complications of multifetal gestation Monochorionic placentation ◦ Twin-twin transfusion syndrome occurs in 9% of mono-di twins ◦ Mortality can be 90% in untreated cases Complications of multifetal gestation Mono-mono twins ◦ Cord entanglement, preterm birth, growth impairment, malformations, genetic abnormalities, vascular anastomoses Gabbe: Obstetrics: normal and problem pregnancies, 6th ed. Saunders 2012 Causes of stillbirth—NICHHD workshop consensus UTERINE COMPLICATIONS Uterine complications Uterine rupture ◦ Evidence of obstructed circulation Uterine abnormalities ◦ There is an increased risk of uterine abnormalities in women with recurrent pregnancy loss/stillbirth ◦ Possibly due to poorly vascularized uterine tissue or space constraints ◦ Increased risk of PPROM, cervical insufficiency, preterm labor ◦ Septate uterus has highest risk of stillbirth and placental abruption Evaluation of stillbirth Workup Workup of stillbirth IMPORTANCE Importance of a stillbirth evaluation Counseling for risk of recurrence Possible intervention to reduce recurrence risk Facilitate emotional closure and healing Most stillbirths remain unexplained Incomplete evaluation ◦ Lack of clinician awareness ◦ Concerns of the family Lack of single universally accepted classification scheme ◦ Difficult to assign a definitive cause Unknown cause ◦ Sometimes despite thorough evaluation Workup of stillbirth OVERVIEW Overview Recommended studies Sometimes helpful Not generally useful •Autopsy •Placental pathology •Karyotype •Kliehauer-Betke •Indirect Coombs •Acquired thrombophilia panel •Anti B2-glycoprotein ab •Toxicology screen •Syphilis serology •Inherited thrombophilia panel •Glucose screening •TSH •CMV, toxoplasmosis, other infectious •Bile acids •Sonohysterogram •Routine TORCH titers •ANA testing •Cultures of placental membranes Silver et al, 2010 How do we know what works? “Evaluation of 1025 fetal deaths: proposed diagnostic workup.” Korteweg FJ, Erwich JJHM, Timmer A, et al. AJOG 2012. Prospective cohort study in 50 Dutch hospitals Singleton IUFDs at >=20wks gestation, excluding pregnancy terminations and intrapartum deaths Cause of death determined by a multidisciplinary panel (2 obstetricians, an OB resident, perinatal pathologist, neonatologist, genetics, microbiologist) ◦ Initial demonstratable pathophysiological entity initiating the chain of events that irreversibly led to death Contribution of each diagnostic test for determination of cause of death was determined by the panel ◦ Valuable for “establishing cause of death” or “excluding cause of death” Workup of stillbirth MEDICAL HISTORY Thorough medical/obstetrical history Workup of stillbirth EXAMINATION OF THE FETUS AND PLACENTA Workup of stillbirth EXAMINATION OF THE FETUS Physician’s exam Weight, head circumference, length Photographs ◦ Frontal and profie ◦ Whole body, face, extremeties, palms, abnormalities Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Time of demise Finding Time of demise Brown or red discoloration of the cord stump Desquamation >1cm >6 hours ago Desquamation of face, back, abdomen >12 hours ago Desquamation >5% of the body or >2 body zones >18 hours ago Skin color brown or tan >24 hours ago Mummification (reduced soft tissue, leathery skin, dark brown) >2 weeks ago “Estimating the time of death in stillborn fetuses: III. External fetal examination; a study of 86 stillborns.” Genest DR, Singer DB. Obstet and Gynecol, 1992; 80(4), 593 Autopsy New information that influences counseling in 26-51% of cases Dutch study: valuable in 72% of cases However, it is performed in <50% of cases ◦ Clinician hesitation to recommend autopsy ◦ Patient reservations Autopsy Ask about patient reservations Emphasize potential benefits to family Allow the family ample time to hold the baby and perform religious/cultural activities first Autopsy Medical autopsies require consent of next-of-kin Consent should be explicit enough that parents can limit the autopsy procedure Illinois Masonic Policy “An autopsy is an option for fetuses 20 weeks or greater, but if clinically indicated or requested by the family, an autopsy can be offered before 20 weeks.” If an autopsy is not requested, a Surgical Pathology examination can be performed Components of an autopsy Review of the clinical history, laboratories, antenatal imaging External examination: ◦ Weight, crown-rump length, foot length, crown-heel length, occipital-frontal circumference ◦ Joint mobility, facial features, hands, feet, genitalia Intraoral examination: ◦ Pharynx, soft palate, uvula Take into consideration changes from maceration Photographs External examination Lentz: Comprehensive Gynecology, 6th ed Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Components of an autopsy Internal examination ◦ Y or T shaped incision on anterior trunk ◦ Organs examined in situ ◦ Heart sometimes opened in situ, sometimes removed and fixed Vascular connections, septal defects ◦ Organs removed in bloc for detailed dissection ◦ Spinal cord removed Components of an autopsy Brain ◦ Coronal scalp incision extending to behind the ears ◦ Skull is opened along cranial sutures ◦ Can extend into posterior neck for posterior fossa (Dandy-Walker, Chiari) by removing occipital bone and cervical vertebrae ◦ Brain is placed in formalin for 10 days before examination Brain Chiari malformation—downward displacement of medulla Fligner 2011 Components of an autopsy Samples of tissue for ◦ Microscopic evaluation ◦ Viral cultures ◦ Bacterial cultures Metabolic studies (Guthrie card) Histologic exam Extramedullary hematopoeisis in fetal liver in fetus with non-immune hydrops Kumar: Robbins pathologic basis of disease, 8th edition. 2009 What autopsy can identify Markers of IUGR ◦ Head circumference percentile higher than weight percentile ◦ Brain weight appropriate for gestation while other organs are appropriate for body weight ◦ Altered brain weight:liver weight Kidneys ◦ Polycystic kidney disease Certain brain pathologies Congenital anomalies Kidneys A: 28 wks, suspicious for autosomal recessive polycystic kidney disease B: confirmed on autopsy C: 22 wks, suspicious for ARPKD D: Autopsy showed diffuse renal cystic dysplasia Autopsy can provide evidence Infection Anemia Hypoxia Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Alternatives to autopsy Partial autopsy ◦ Head-sparing autopsy (may miss CNS pathology) External examination by a trained pathologist ◦ Can identify syndromes, congenital anomalies, timing of death, growth anomalies ◦ Will likely miss fetal infections and internal anomalies External examination with selected biopsies ◦ More likely to identify fetal infections Alternatives to autopsy: MRI Advantages ◦ Very good for CNS pathology Sometimes better than autopsy, because fetal brain has high water content and liquefies ◦ Fluid collections and effusions in the body Disadvantages ◦ May miss cardiac anomalies, bowel anomalies ◦ Cannot diagnose infections or metabolic disease MRI 24 wks, massive bilateral intraventricular hemorrhage Fligner 2011 MRI Image-guided percutaneous biopsies ◦ <50% success rate at obtaining tissue in one study ◦ Somewhat inferior to autopsy: 12 cases where “minimally invasive autopsy” provided equivalent information to autopsy 12 cases where “minimally invansive autopsy” provided inferior information than autopsy 2 cases where MRI and biopsy provided superior information However, 73% of minimally invasive autopsies provided Information of equivalent clinical significance to autopsy Fligner 2011 Alternatives to autopsy X ray ◦ Useful for skeletal dysplasias ◦ Ribs/vertebrae as part of diagnosis of VACTERL or diabetic fetopathy X ray Achondrogenesis 1b (absence of vertebral bodies) Fligner 2011 X ray Hemivertebrae (VACTERL) Fligner 2011 Suggested workup of stillbirth EXAMINATION OF THE PLACENTA Examination of the placenta The most valuable diagnostic test in most studies ◦ Dutch study showed it to be valuable in 95% of cases Provides additional information in 30% of cases Examination of the placenta Weight in relation to norms for gestational age Evidence of abruption, infarction, thrombophilias Hemosiderin depositschronic abruption ◦ Perivillious and marginal fibrin deposition ◦ Decidual necrosis ◦ Evidence of infarction Examination of the placenta Multiples: chorionicity, vascular anastomoses in multifetal gestations Cord: thrombosis, velamentous cord insertion, vasa previa Evidence of infections ◦ More common in preterm stillbirth ◦ Viral nuclic acid amplification ◦ Bacterial cultures Examination of the placenta Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Workup of stillbirth GENETICS Karyotype Abnormal fetal karyotype noted in 8-13% of all stillbirths and in >20% of those with morphologic abnormalities or IUGR Dutch study: 11.9% prevalence of a chromosomal abnormality in the 362 IUFDs who underwent karyotyping ◦ 37% trisomy 21, 16% monosomy X, 4% trisomy 13 Karyotype was valuable in 29% of cases Cell culture Successful in only ~50% of cases Cells must be cultured in vitro—need metaphase chromosomes Only 1% of cells are dividing at any time Kumar: Robbins pathologic basis of disease, 8th edition. 2009 Cell culture Acceptable cytologic specimens: ◦ Amniotic fluid (yield is 84%) obtained by amniocentesis at the time of prenatal diagnosis of demise, 20-30mL ◦ 1x1cm placental block from below the cord insertion site on an unfixed placenta ◦ 1.5cm segement of umbilical cord ◦ Internal fetal tissue specimen (costochondral junction, patella, lung, kidney, gonad, not skin) Cell culture Collect the specimen in a sterile manner ◦ Prokaryotic cells outcompete and overgrow any human cells Transport to the laboratory as soon as possible Blood, amniotic fluid, chorionic villi at room temperature Solid tissue transported on wet ice ◦ Lysosomal enzyme activity is inhibited at 4 C and viability is maintained Cell culture Monolayer in situ Up to 2 weeks for solid tissue culture Cells are swelled hypotonically, ruptured (blowing on the coverslip) and metaphase chromosomes are spread Automatic robotic harvesters Stained with Giemsa or Wright ◦ Results in banding pattern unique to each chromosome Karyotype Count the chromosomes in each cell ◦ Technologist at a microscope Must analyze 15-20 cells to get karyotype Photograph of karyogram or computer-assisted imaging ◦ Manipulate/move chromosomes ◦ Pattern-recognition software to generate karyogram ◦ Computer must be doublechecked by a technologist Stein 2011 If culture is unsuccessful Flourescent in-situ hybridization (FISH) ◦ Can test for the most common aneuploidies ◦ Can test for specific mutations FISH Molecular probe ◦ Fluorescent dye ◦ Visualized using fluorescence microscopy Molecular probes can be ◦ Specific to certain mutations ◦ A cocktail that coats the whole chromosome FISH can be performed on metaphase or interphase chromosomes—cell culture not required for FISH FISH DNA is denatured and allowed to hybridize with the probe Nonhybridized DNA is then counterstained FISH X, X Normal chromosome 21 Trisomy 21 Stein 2011 FISH Microdeletion in chromosome 22 associated with DiGeorge syndrome Stein 2011 FISH Advantages Does not require metaphase chromosomes Can obtain karyotype and information about mutations Disadvantages Probes must be known genes/mutations Limited number of colors can be seen with fluorescent microscope FISH with computer-assisted system •Fluorochromes can be mixed •Too subtle for human eye, but computer assisted systems allow detection of all 24 chromosomes •Karyotype in interphase Trisomy 18 and XXY Stein 2011 If live cells are not available: Microarray Screens the genome for copy number variations (CNPs) ◦ BAC arrays provide overview of genome ◦ SNP arrays provide more detailed coverage with probes on every 100-1000 base pairs ◦ Detects deletions, duplications, aneuploidies, unbalanced translocations with a gain/loss of sequences Good for small deletions or cryptic changes ◦ Cytogenetics resolution is only 5-10Mb Microarray Stein 2011 Limitations Many copy number changes are of uncertain clinical significance ◦ More CNVs are being identified every day It will not detect balanced translocations or inversions Microarray versus karyotyping Reddy UM et al, 2012: Prospective populationbased study of 532 stillbirths over 2 years Patients with IUFD underwent: ◦ Interview, chart abstraction, postpartum examination, placental pathology, karyotype analysis, and specimen collection DNA analyzed with an SNP microarray with data aligned to Human Genome release 18 Microarray versus karyotyping Benign CNV: full length listed in any of three databases of unaffected persons Pathogenic CNV: ◦ Evidence of pathogenicity in literature ◦ A gene listed in the OMIM database that is known to cause developmental/lethal disease ◦ In a pathogenic database Probably benign CNV: no evidence of pathogenicity in literature Unknown CNV Microarray versus karyotyping Microarray analysis yielded a result in 87.4% stillbirths compared to 70.5% for karyotype 85.2% of these were benign, too small, or probably benign 2.6% were pathogenic, 6.9% were aneuploid Microarray detected CNV consistent with DiGeorge syndrome not detected by karyotype in 3 cases Conclusions: microarray Genetic workup should be guided by Disadvantages Advantages family history and presence of More expensive Can detect congenital mutations tooanomalies small for FISH Higher chance of Consider microarray when karyotype obtaining a result fails to grow in culture Workup of stillbirth MATERNAL WORKUP Workup of stillbirth IMMEDIATE MATERNAL WORKUP Laboratories (Recommended) CBC Kliehauer-Betke Human parvovirus B-19 IgG and IgM Lupus anticoagulant, anticardiolipin antibodies Indirect Coombs ◦ If not already done antepartum Toxicology screen Kliehauer Betke Recommended to do before induction of labor However, given that only massive hemorrhage is likely to cause fetal death, can also be done up to 2-3 weeks after delivery In Dutch study, FMH was a contributing factor in 10.6% of the total cohort Kliehauer Betke Reddy et al 2009 Antiphospholipid antibodies One fetal death satisfies criteria for testing Confirm with repeat testing in 6-12 weeks Given significant implications for More likely positive if stillbirth was accompanied by IUGR or severe preeclampsia future pregnancies and future Two dutch studies (750 fetal deaths in Korteweg et health of the testing et is al 2012) al 2010, 1025 fetal mother, deaths in Korteweg showed that neither testing for acquired nor generally recommended inherited thrombophilia is valuable ◦ Unless the patient has a family or personal history of thrombophilia Laboratories (Sometimes useful) Syphilis TSH Inherited thrombophilia workup Guided by maternal history and risk ◦ Factor V Leiden, prothrombin gene mutation, antithrombin III, fasting homocysteine factors Glucose screening Sonohysterogram ◦ Especially if loss associated with preterm labor, PPROM, cervical insufficiency, previable gestations, fetal malpresentation Inherited thrombophilia Korteweg et al 2010. Multicenter, prospective study. 750 singleton fetal deaths >=20 wks, Consider it in cases of severe excluding terminations placental pathology, a and Tested for vWF, antithrombin, IUGR, protein or C, total free protein prothrombin gene mutation, factor history of S,thrombosis V Leiden However, remember most Cause of death classified bythat a panel “Except forwith vWF and paternal free protein S, women these conditions will acquired and thrombophilic defects were not haveprevalent uncomplicated pregnancies more after fetal death.” However, many case-control studies show an association Laboratories (unproven benefit) Toxoplasmosis, rubella, CMV, HSV, other infections ◦ Viruses for which vaccines are prevalent are uncommon in developed countries ◦ However, if autopsy, pathology, or history is suggestive, take maternal/neonatal serology, special tissue staines, testing for nucleic acids ANA Routine TORCH Dutch study: of the women tested for TORCH, 17.0% had positive IgM for TORCH, parvo, syphilis, or hepatitis B However only 1.8% of the total cohort had infection as the cause of death Suggested workup of stillbirth POSTPARTUM MATERNAL WORKUP In selected cases Paternal karyotype Protein S and C activity Kliehauer-Betke Evaluation of stillbirth Considerations AIMMC protocol All intact fetal remains are sent to the morgue within 4 hours of expiration, UNLESS a Surgical Pathology examination is requested If a Surgical Pathology examination is requested ◦ Remains with a Surgical Pathology requisition to the Histology Laboratory ◦ Central Transport and Nursing are responsible for the initial transport of the body to the morgue and filling out the morgue census sheet AIMMC protocol If autopsy is requested, the fetus is obtained from the morgue An autopsy is an option for fetuses >=20 weeks ◦ But if clinically indicated or requested by the family, an autopsy can be offered before 20 weeks AIMMC protocol Autopsies are performed by AIMMC pathologists ◦ Trained in fetal/neonatal autopsies ◦ Consult specialists when needed Preliminary result in 24 hours; final result in 30 days Genetic and molecular testing at ACL A fetus that undergoes an autopsy can still receive private burial Fetal death disposition notification Within 24 hours after an abortion/miscarriage the mother must be informed of her right to determine the final disposition of the remains ◦ Private burial ◦ Cremation ◦ Hospital disposition Fetal death disposition notification http://www.idph.st ate.il.us/vitalrecord s/pdf/Fetal%20Dea th%20Disposition%2 0Notification.pdf Fetal death disposition notification If patient is unclear, sign the form without making a selection ◦ RN notes “undecided at discharge” Fax a copy to Mission and Spiritual Care at 773296-5010 and place a copy in the chart Mission and Spiritual Care or the Perinatal Loss Coordinator will follow up with the family If the family can not be reached within 2 weeks, Pathology will initiate the procedure for hospital disposition Private burial Perinatal loss coordinator has a list of funeral homes Cremation or burial Only a licensed funeral director can pick up the fetus ◦ Parents provide the name to Health Information Management Cost: some funeral home directors reduce the rate ◦ Medicaid pays for modest funeral and burial For very young fetuses, parents advised that there might not be many remains after autopsy Hospital disposition St Luke’s Cemetery ◦ 5300 N. Pulaski Road, Chicago, IL 60630 “Babyland,” exact location not identified No charge Perinatal loss coordinator Always notifiy Anna Zieba (pager 61-7656, phone 61-7127) Always notify Mission and Spiritual Care 61-5005 ◦ Can provide religious services from most religions Considerations Parents benefit from seeing/holding the infant ◦ Warn them about how the baby will appear Use the term “baby” Encourage parents to name the infant ◦ Knowing the sex is important Fetal loss can be devastation at any gestational age Different cultures grieve in different ways Considerations Keepsakes and memory boxes Child Life specialist can aid with siblings For a loss in the ER, consider consulting crisis if parents show signs of depression Bereavement care track after discharge Evaluation of stillbirth Conclusions Conclusions The cause of a stillbirth is the initial pathophysiologic entity that irreversibly led to fetal death Cause must be proven with evidence of fetal harm There are many benefits to finding a cause Encourage patients to allow an evaluation within the boundaries of their personal and cultural values Conclusions Recommended laboratories are CBC, Kliehauer-Betke, parvovirus B-19 IgG and IgM, lupus anticoagulant, anticardiolipin antibodies, and toxicology screen Only perform other labs as indicated by maternal history Encourage patients to receive an autopsy ◦ Partial autopsy and MRI are alternatives Always send the placenta to pathology Conclusions Encourage karyotyping Base evaluation for other chromosomal abnormalities on family history and results of other studies Consider FISH or microarray if low likelihood of getting a result from cell culture Utilize hospital resources for perinatal loss THANK YOU Evaluation of stillbirth Sources ACOG Practice Bulletin Number 102. “Management of Stillbirth.” American College of Obstetricians and Gynecologists. March 2009. acog.org Fligner CL, Dighe M. “Fetal and Perinatal Death Investigation: Redefining the Autopsy and the Role of Radiologic Imaging.” Ultrasound Clin 6, 2011 (105-117). Illinois Masonic Medical Center Perinatal Loss Policy. Policy 20.118.044 Korteweg FJ, Erwich JJHM, Timmer A, et al. “Evaluation of 1025 fetal deaths: proposed diagnostic workup.” Am J Obstet Gynecol 2012; 206:53.e1-12. Korteweg FJ, Erwich JJHM, et al. “Prevalence of Parental Thrombophilic Defects after Fetal Death and Relation to Cause.” Obstet and Gynecol. August 2010, Vol 116, No 2, part 1. Kumar: Robbins and Coltran Pathologic Basis of Disease, Professional Edition, 8th ed. 2009 Saunders, an imprint of Elsevier. Reddy UM, Goldenburg R, et al. “Stillbirth Classification—Developing an International Consensus for Research.” Obstet and Gynecol. Oct 2009, Vol 114, No 4. Reddy UM, Page GP, Saade GR. “Karyotype versus Microarray testing for Genetic Abnormalities after Stillbirth.” N Engl J med 367; 23, December 2012 Silver R, Heuser C. “Stillbirth Workup and Delivery Management.” Clin Obstet and Gynecol 2010; 53, 3. Stein, CK. “Applications of cytogenetics in Modern Pathology.” McPherson: Henry’s Clinical Diagnosis and Management by Laboratory Methods, 22nd ed. 2011 Saunders, an imprint of Elsevier.