Reproduction
advertisement

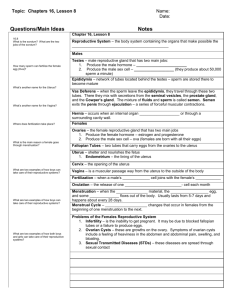
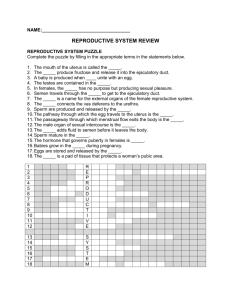
Reproduction General Biology 102 SUNY Orange at S. S. Seward Institute Both asexual and sexual reproduction occur in the animal kingdom • Asexual reproduction is creation of offspring whose genes all come from one parent • Sexual reproduction is creation of offspring by fusion of male gametes (sperm) and female gametes (eggs) to form zygotes Mechanisms of Asexual Reproduction • Many invertebrates reproduce asexually by fission, separation of a parent into two or more individuals of about the same size • Budding - two new individuals arise from outgrowths of existing ones • Fragmentation - breaking of the body into pieces, some or all of which develop into adults – must be accompanied by regeneration, regrowth of lost body parts Reproductive Cycles and Patterns • Most animals exhibit reproductive cycles related to changing seasons • Reproductive cycles are controlled by hormones and environmental cues • Animals may reproduce asexually or sexually, or they may alternate these methods • Parthenogenesis is a process in which an egg develops without being fertilized • Several genera of fishes, amphibians, and lizards reproduce only by a complex form of parthenogenesis Ovary size Ovulation Hormone level Ovulation Estrogen Progesterone Behavior Time Femalelike Malelike Femalelike Malelike • Sexual reproduction is a special problem for organisms that seldom encounter a mate • One solution is hermaphroditism - each individual has male and female reproductive systems • In sequential hermaphroditism, an individual reverses its sex during its lifetime Fertilization depends on mechanisms that help sperm meet eggs of the same species • The mechanisms of fertilization, the union of egg and sperm, play an important part in sexual reproduction • In external fertilization, eggs shed by the female are fertilized by sperm in the external environment Eggs • Internal fertilization - sperm are deposited in or near the female reproductive tract, and fertilization occurs within the tract • - requires critical timing, often mediated by environmental cues, pheromones, and/or courtship behavior • - requires behavioral interactions and compatible copulatory organs Ensuring the Survival of Offspring • All species produce more offspring than the environment can handle, but the proportion that survives is quite small • Embryos of many terrestrial animals develop in eggs that can withstand harsh environments • Many animals retain the embryo, which develops inside the female • In many animals, parental care helps ensure survival of offspring Gamete Production and Delivery • Must have systems that produce gametes • The least complex systems do not contain distinct gonads • More complex systems contain many sets of accessory tubes and glands that carry, nourish, and protect gametes and developing embryos • Many animals with relatively simple body plans have highly complex reproductive systems Genital pore Male organs: Seminal vesicle (Digestive tract) Female organs: Uterus Yolk gland Yolk duct Sperm duct (vas deferens) Oviduct Ovary Vas efferens Seminal receptacle Testis (Excretory pore) • Most insects have separate sexes with complex reproductive systems Accessory gland Testis Ovary Ejaculatory duct Oviduct Spermatheca Vas deferens Seminal vesicle Male honeybee (drone) Penis Vagina Accessory gland Female honeybee (queen) Reproductive organs produce and transport gametes: humans Female Reproductive Anatomy • The female external reproductive structures include the clitoris and two sets of labia • The internal organs are a pair of gonads and a system of ducts and chambers that carry gametes and house the embryo and fetus Female Reproductive Anatomy • Labia majora pubic bone • Labia minora ovary • Clitoris oviduct • Uterus cervix • Vagina endometrium • Urinary bladder follicle • Rectum corpus luteum Oviduct Ovary Uterus (Urinary bladder) (Rectum) (Pubic bone) Cervix Urethra Shaft Vagina Glans Bartholin’s gland Clitoris Prepuce Labia minora Vaginal opening Labia majora Oviduct Ovaries Follicles Corpus luteum Uterus Uterine wall Endometrium Cervix Vagina Ovaries • The female gonads, the ovaries, lie in the abdominal cavity • Each ovary – Has tough protective capsule – contains many follicles • Follicle consists of one egg surrounded by one or more layers of follicle cells • Ovulation expels an egg cell from the follicle • Remaining follicular tissue grows within the ovary, forming a mass called the corpus luteum (body, yellow) • The corpus luteum secretes hormones, depending on whether pregnancy occurs Oviducts and Uterus • Egg cell is released into the abdominal cavity near the opening of the oviduct, or fallopian tube • Cilia in the tube convey the egg to the uterus Vagina and Vulva • Vagina - thin-walled chamber that is the repository for sperm during copulation and serves as the birth canal • opens to the outside at the vulva, Mammary Glands • Mammary glands are not part of the reproductive system but are important to mammalian reproduction • Within the glands, small sacs of epithelial tissue secrete milk Male Reproductive Anatomy • Urinary bladder vas deferens • Urethra prostate gland • Epididymis testis • Erectile tissue scrotum • Seminal vesicle glans penis • Blulbourethral gland pubic bone Male Reproductive Anatomy • In most mammals, the male’s external reproductive organs are the scrotum and penis • Internal organs are the gonads, which produce sperm and hormones, and accessory glands Seminal vesicle (Urinary bladder) (Rectum) (Public bone) Vas deferens Erectile tissue of penis Ejaculatory duct Prostate gland Bulbourethral gland Urethra Vas deferens Glans penis Epididymis Testis Scrotum Prepuce Seminal vesicle (behind bladder) (Urinary bladder) Prostate gland Bulbourethral gland Urethra Erectile tissue of penis Scrotum Vas deferens Epididymis Glans penis Testis • The male gonads, or testes, consist of highly coiled tubes surrounded by connective tissue • Sperm form in these seminiferous tubules • Production of normal sperm cannot occur at the body temperatures of most mammals • The testes of many mammals are held outside the abdominal cavity in the scrotum, where the temperature is lower than in the abdominal cavity Ducts • From the seminiferous tubules of a testis, sperm pass into the coiled tubules of the epididymis • During ejaculation, sperm are propelled through the muscular vas deferens and the ejaculatory duct, and then exit the penis through the urethra Glands • Three sets of accessory glands add secretions to the semen, the fluid that is ejaculated • The two seminal vesicles contribute about 60% of the total volume of semen • The prostate gland secretes its products directly into the urethra through several small ducts • The bulbourethral gland secretes a clear mucus before ejaculation that neutralizes acidic urine remaining in the urethra Penis • The human penis is composed of three cylinders of spongy erectile tissue • During sexual arousal, the erectile tissue fills with blood from the arteries, causing an erection Human Sexual Response • Two reactions predominate in both sexes: – Vasocongestion, the filling of tissue with blood – Myotonia, increased muscle tension • The sexual response cycle has four phases: excitement, plateau, orgasm, and resolution In humans and other mammals, a complex interplay of hormones regulates gametogenesis • The process of gametogenesis is based on meiosis, but differs in females and males • Oogenesis is development of mature ova • Spermatogenesis is production of mature sperm Ovary Primary germ cell in embryo Differentiation Oogonium Oogonium in ovary Mitotic division Primary oocyte within follicle Primary oocyte Completion of meiosis I and onset of meiosis II First polar body Growing follicle Secondary oocyte Ovulation Entry of sperm triggers completion of meiosis II Second polar body Mature follicle Ruptured follicle Ovum Ovulated secondary oocyte Corpus luteum Degenerating corpus luteum Epididymis Seminiferous tubule Testis Cross section of seminiferous tubule Spermatogonium Sertoli cell nucleus Mitotic division, producing large numbers of spermatogonia Differentiation and onset of meiosis I Primary spermatocyte (in prophase of meiosis I) Meiosis I completed Secondary spermatocyte Meiosis II Early spermatids Lumen of Seminiferous tubule Spermatids (at two stages of differentiation) Differentiation Neck Sperm cells Head Midpiece Tail Plasma membrane Acrosome Nucleus Mitochondria • Oogenesis differs from spermatogenesis – 3 major ways: – During meiotic divisions, cytokinesis is unequal, with almost all of the cytoplasm in one daughter cell, the secondary oocyte – Unlike sperm, eggs are not produced continuously throughout life – Oogenesis has long “resting” periods, whereas sperm are produced in uninterrupted sequence Reproduction • Where do babies really come from? The Reproductive Cycles of Females • In females, the secretion of hormones and the reproductive events they regulate are cyclic Menstrual Versus Estrous Cycles • Two different types of cycles occur in females • Humans and other primates have menstrual cycles; other mammals have estrous cycles • In both cases, ovulation occurs after the endometrium has started to thicken in preparation for implantation • In menstrual cycles: – The endometrium is shed from the uterus in a bleeding called menstruation – Sexual receptivity is not limited to a timeframe • In estrous cycles: – The endometrium is reabsorbed by the uterus – Sexual receptivity is limited to a “heat” period The Human Female Reproductive Cycle: A Closer Look • The female reproductive cycle is one integrated cycle involving two organs: the uterus and ovaries • Secretion of GnRH from the hypothalamus and of FSH and LH from the anterior pituitary orchestrates the female reproductive cycle • Five kinds of hormones participate in an elaborate scheme involving positive and negative feedback Control by hypothalamus Inhibited by combination of estrogen and progesterone Hypothalamus Stimulated by high levels of estrogen GnRH Anterior pituitary FSH Inhibited by low levels of estrogen LH Pituitary gonadotropins in blood LH FSH FSH and LH stimulate follicle to grow LH surge triggers ovulation Ovarian cycle Growing follicle Corpus luteum Mature follicle Follicular phase Ovulation Degenerating corpus luteum Luteal phase Progesterone and estrogen secreted by corpus luteum Estrogen secreted by growing follicle in increasing amounts Ovarian hormones in blood Peak causes LH surge Progesterone Estrogen Estrogen level very low Progesterone and estrogen promote thickening of endometrium Uterine (menstrual) cycle Endometrium Days Menstrual flow phase Proliferative phase 0 5 10 Secretory phase 14 15 20 25 28 The Ovarian Cycle • In the ovarian cycle, hormones stimulate follicle growth, which results in ovulation • Following ovulation, the follicular tissue left behind transforms into the corpus luteum The Uterine (Menstrual) Cycle • Cycle after cycle, the maturation and release of egg cells from the ovary are integrated with changes in the uterus • If an embryo has not implanted in the endometrium by the end of the secretory phase, a new menstrual flow commences Menopause • After about 450 cycles, human females undergo menopause, the cessation of ovulation and menstruation Hormonal Control of the Male Reproductive System • Testosterone and other androgens are directly responsible for the primary and secondary sex characteristics of the male • Androgen secretion and sperm production are controlled by hypothalamic and pituitary hormones LE 46-14 Stimuli from other areas in the brain Hypothalamus GnRH Anterior pituitary Negative feedback FSH LH Leydig cells make testosterone Primary and secondary sex characteristics Sertoli cells Spermatogenesis Testis In humans and other placental mammals, an embryo grows into a newborn in the mother’s uterus • Pregnancy, or gestation, is the condition of carrying one or more embryos in the uterus • Duration of pregnancy in other species correlates with body size and maturity of the young at birth Conception, Embryonic Development, and Birth • Conception, fertilization of an egg by a sperm, occurs in the oviduct • After fertilization, the zygote undergoes cleavage and develops into a blastocyst before implantation in the endometrium Cleavage starts Cleavage continues Ovary Fertilization occurs The blastocyst implants Uterus Ovulation Endometrium From ovulation to implantation Endometrium Inner cell mass Cavity Blastocyst Implantation of blastocyst Trophoblast First Trimester • Human gestation can be divided into three trimesters of about three months each • The first trimester is the time of most radical change for both the mother and the embryo • During its first 2 to 4 weeks, the embryo obtains nutrients directly from the endometrium • Meanwhile, the outer layer of the blastocyst mingles with the endometrium and eventually forms the placenta • Blood from the embryo travels to the placenta through arteries of the umbilical cord and returns via the umbilical vein Maternal arteries Maternal veins Placenta Maternal portion of placenta Umbilical cord Chorionic villus containing fetal capillaries Fetal portion of placenta (chorion) Maternal blood pools Uterus Fetal arteriole Fetal venule Umbilical cord Umbilical arteries Umbilical vein • The first trimester is the main period of organogenesis, development of the body organs 5 weeks. 14 weeks. 20 weeks. Second Trimester • During the 2nd trimester – The fetus grows and is very active – The mother may feel fetal movements – The uterus grows enough for the pregnancy to become obvious Third Trimester • During the 3rd trimester, the fetus grows and fills the space within the embryonic membranes • A complex interplay of local regulators and hormones induces and regulates labor, the process by which childbirth occurs from ovaries Oxytocin from fetus and mother’s posterior pituitary Induces oxytocin receptors on uterus Stimulates uterus to contract Stimulates placenta to make Prostaglandins Stimulate more contractions of uterus Positive feedback Estrogen • Birth, or parturition, is brought about by a series of strong, rhythmic uterine contractions Placenta Umbilical cord Uterus Placenta (detaching) Uterus Cervix Umbilical cord Dilation of the cervix Expulsion: delivery of the infant Delivery of the placenta The Mother’s Immune Tolerance of the Embryo and Fetus • A woman’s acceptance of her “foreign” offspring is not fully understood • It may be due to suppression of the immune response in her uterus Modern Reproductive Technology • Amniocentesis and chorionic villus sampling are invasive techniques in which amniotic fluid or fetal cells are obtained for genetic analysis • Noninvasive procedures usually use ultrasound imaging to detect fetal condition • Modern technology can help infertile couples by in vitro fertilization Head Head Body Body