Cardiovascular: Heart - Misericordia University
advertisement

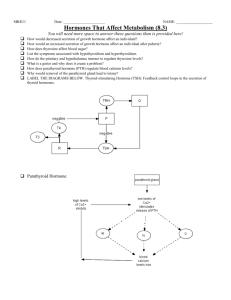
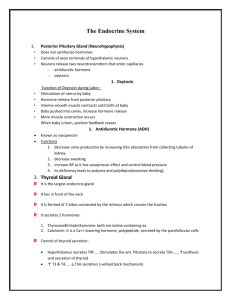
Endocrine System Biology 211: Anatomy & Physiology 1 Tony Serino, Ph.D. Biology Department Misericordia University Endocrine System • Controls and modifies the internal environment by releasing chemicals (hormones) into the blood • Slower response time but longer duration of action compared to nervous system Chemical Messengers (hormones) • Hormone –secreted by cell into blood and acts on another cell some distance away • Neurohormone –secreted by neuron into blood to affect a target cell some distance away • Local hormones –secreted by cell into interstitial fluid to affects cells nearby – Paracrines –affect neighboring cells – Autocrines –affect the secreting cell • Pheromones –secreted by cell onto body surface to affect cells of another individual Hormones • Chemical Classification – Amines –single or few amino acids, most water soluble • Epinephrine, Thyroxine (but water insoluble), Melatonin – Proteins –short to long chains of amino acids; water soluble • GH, FSH, LH, Insulin, Glucagon, ADH, etc. – Steroids –derivatives of cholesterol; water insoluble • Estrogen, Testosterone, Progesterone, Cortisol, Aldosterone Steroid Hormones Characteristics Common to all Hormones • Must have target cell with appropriate receptor molecules • Receptor-hormone complex must trigger events in target cell that changes its physiology • Mechanisms for deactivating the hormone response must be present Controlling Hormone Response • Half-life of the hormone • Physiological range • Modifying target cell response – Up and down regulation • Turning off secretion – Negative feedback – Control by other hormones, neurons and metabolites Control of Hormone Secretion Mechanisms of Hormone Action 2nd messengers Water Soluble Water Insoluble Carrier protein nd 2 Messengers: cAMP 2nd Messengers: IP3 and Ca++-Calmodulin Steroid Hormone Transduction Different Styles of Secretion • Prohormone –a hormone that is made as a larger (inactive form) that must be changed prior to secretion (allows for storage of hormone in secreting cell) Ex.: proinsulin, pro-opiomelanocortin • Prehormone –a hormone that is secreted in an inactive form that must be changed near or in the target cell Ex.: Thyroxine, Angiotensinogen Proinsulin Types of Endocrine Disorders • Hypersecretion – Too much secretion of the hormone • Hyposecretion – Too little secretion of hormone • Hyporesponsiveness – Normal secretion, but little to no response by target cells Endocrine Glands Hypothalamus Control of Pituitary Posterior Pituitary Anterior Pituitary Control of Growth • Growth periods: prenatal and postnatal (consists of pre-puberal (especially the first 2 years –infancy) and puberty • Several factors influence growth: genetics, diet, health, and hormonal balance • Prenatal growth dominated by insulin secretion, post-natal dominated by GH, thyroxine, and sex hormones GH secretion and effects Increase protein synthesis (increase mitosis) Increase differentiation GH secretion stimulated by exercise, fasting, sleep (diurnal rhythm), stress, decreased plasma glucose, increased plasma AA (such as after a high protein meal) GH interactions with other Hormones • Thyroxine: essential and permissive for GH – Needed to maintain energy levels for growth – Increases sensitivity of target cells to GH effects • Insulin: essential for GH effects – Dominant hormone for pre-natal growth • Estrogen and Testosterone: surge at puberty stimulates GH release, synergistic with GH anabolism; also trigger epiphyseal closure • Cortisol: anti-growth effects; decrease GH secretion, cell division, and increase catabolism GH pathologies • Hypersecretion: – Gigantism –in children with responsive epiphyseal plates – Acromegaly –in adults, with closed epiphyseal plates GH pathologies • Hypofunction: – Dwarfism –in children • Pituitary –decreased GH secretion • Laron –decreased responsiveness due to lack of GH receptors 28 yo woman with pituitary dwarfism; 45” tall Achondroplastic Dwarfism (genetic dwarf) due to failure of cartilage to form in epiphyseal plate Thyroid Location Thyroid Follicle (follicular cells thyroxine) Parafollicular cells calcitonin T3 & T4 Formation and Secretion T3 & T4 Control of Thyroxine Secretion Short loop Long loop Thyroid Malfunction • Hypothyroidism • Endemic goiters –due to iodine deffeicency • Cretinism –i thyroxine in child results in igrowth (dwarf) and severe mental retardation • Myxedema –i thyroxine in adult, leads to swelling of tissues plus other symptoms Cretinism Thyroid Malfunction • Hyperthyroidism • Toxic goiters (Graves disease) –Ab may stimulate thyroid without negative feedback control • Exophthalmos –symptom present in many hyperthyroid patients Parathyroid Location Parathyroid PTH Actions • Stimulates resorption of bone hCa+ and PO4- in blood • Stimulates Ca+ absorption in intestine (active Vit. D3 necessary for Ca+ absorption) • Stimulates Ca+ reabsorption and PO4- excretion in kidney • Stimulates Vit. D3 formation (skin) and activation (kidney) • Vital for life Adrenal Location and Structure Adrenal Layers (Epinephrine (adrenalin)) (Androgens) (Glucocorticoids (cortisol)) (Mineralocorticoids, (Aldosterone)) GAS (General Adaptation Syndrome) Adrenal Malfunction • Hypersecretion Cushing’s syndrome –increase in glucocorticoids – Usually due to over secretion of ACTH by pituitary or from adrenal cortex tumors stimulating an increase in glucocorticoids. Characteristic obesity of trunk only and development of “buffalo hump” (a fat pad behind the shoulders). Will develop hypertension, atherosclerosis, muscular weakness and fatigue. Conn’s syndrome –excess amount of aldosterone – Salt imbalance, water retention, hBP, muscle weakness Adrenogenital syndrome –too much androgen – Premature sexual development in children or masculinization in women Cushings (buffalo hump) Obesity of trunk Adrenogenital syndrome A 15 yo girl, note typical masculine build, under developed breasts, and excessive body hair Adrenal Cortex Malfunction • Hyposecretion –Addison’s disease – Due to decrease amounts of mineral and glucocorticoids – Can be due to over use of steroids or an autoimmune mechanism resulting in destruction of the gland – Dehydration, K+ loss, iBP, fatigue, pigmentation deepening (bronzing of skin) may be symptom of loss of negative feedback Pineal Gland • Plays a major role in circadian rhythm control through its sympathetic connection to the hypothalamus • Melatonin increases at night and decreases during daylight • Implicated in the control of major life changes (such as the onset of puberty and adulthood Thymus Gland • Bilobed organ that is largest in children, but begins to regress sharply at the onset of puberty (around age 11) • It is the site of T-cell lymphocyte production and produces hormones (such as, thymosin) that modifies their physiology