GASTROINTESTINAL SYSTEM
advertisement

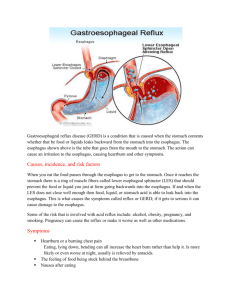
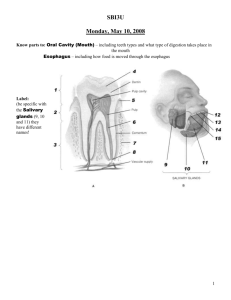
CH 16 Goodman Upper GI (mouth, esophagus, stomach and duodenum) - ingestion and digestion Lower GI: small intestines - digestion, absorption of nutrients; large intestines – absorbs water and electrolytes, stores waste products until elimination Enteric nervous system - just as many nerves as the spinal cord; can function completely independent of the CNS; it is thought that the “brain in the bowel” can have its own form of neuroses (such as functional bowel syndromes) PT needs to be aware of the clinical manifestations of GI issues - many have implications on physical activity tolerance and healing / recovery (dehydration, malnutrition, anemia) Gastrointestinal System Mouth>pharynx>esophagus>stomach>small intestine (duodenum, jejunum, ileum)>large intestine (cecum, ascending, transverse, descending, sigmoid) >rectum>anus **liver, gallbladder and pancreas needed for digestion Liver The liver has multiple functions, but two of its main functions within the digestive system are to make and secrete an important substance called bile and to process the blood coming from the small intestine containing the nutrients just absorbed. The liver purifies this blood of many impurities before traveling to the rest of the body. Gallbladder The gallbladder is a storage sac for excess bile. Bile made in the liver travels to the small intestine via the bile ducts. If the intestine doesn't need it, the bile travels into the gallbladder, where it awaits the signal from the intestines that food is present. Bile serves two main purposes. First, it helps absorb fats in the diet, and secondly, it carries waste from the liver that cannot go through the kidneys. Pancreas Among other functions, the pancreas is the chief factory for digestive enzymes that are secreted into the duodenum, the first segment of the small intestine. These enzymes break down protein, fats, and carbohydrates. Aug. 21, 2009 — The lowly appendix, long- regarded as a useless evolutionary artifact, won newfound respect two years ago when researchers at Duke University Medical Center proposed that it actually serves a critical function. The appendix, they said, is a safe haven where good bacteria could hang out until they were needed to repopulate the gut after a nasty case of diarrhea, for example. *Has been regarded as a vestigial structure (one that has lost all or most of its original function through evolution) www.sciencedaily.com Nausea (symptom) uneasy feeling - as if going to vomit - caused by irritation in nerve ending of stomach Vomiting (sign) Flow of stomach contents backwards through upper GI......and either aspirated into lungs or out the mouth (if back down the esophagus is technically just reflux) Caused by anything that causes nausea Complications include fluid and electrolyte imbalances, pulmonary aspiration --> aspiration pneumonia; malnutrition; rupture of esophagus; dental decay (if prolonged) If vomit is blood mixed with stomach acids looks like “coffee-grounds” and is aptly referred to as “coffee-ground vomit” Diarrhea (sign) Abnormal fluid mixture, frequency and/or volume of stool Results in poor absorption of fluid, nutritive elements, and electrolytes Anorexia (symptom vs. sign) Diminished appetite or aversion to food Anorexia - Cachexia (sign) Anorexia that results in wasting of muscle; is a common systemic response to cancer Associated with poor intake and high metabolic rate Constipation (sign) Fecal matter is too hard to pass easily; or when bowel movements are so infrequent that discomfort and other symptoms interfere with daily activities May occur due to diet, dehydration, side effect of medication, acute or chronic disease of digestion system, inactivity or prolonged bed rest, emotional stress Dysphagia (sign vs. symptom) Difficulty swallowing that results in the sensation that food is stuck somewhere in the throat or chest; may be a symptom / sign of many other disorders other than GI - such as neurological conditions Achalasia (sign vs. symptom) Rare disorder that makes it difficult for food and liquid to pass from esophagus to stomach. Due to loss of nerve cells in the esophagus so that food is not propelled down the GI tract Also, the lower esophageal sphincter (LES) which connects the esophagus and the stomach doesn’t fully relax. This results in a feeling of “fullness” in the sternal region that can progress to dysphagia Heartburn (symptom) Pain or burning sensation in the esophagus, can radiate to arms, jaw or back Abdominal pain Inflammatory - due to inflammation Mechanical - stretching of the walls of GI tract Ischemic - due to buildup of metabolites that are released in an area of reduced blood flow GI Bleeding Accumulation of blood in GI tract is irritating and tends to cause discomfort; vomiting (Coffee ground vomit), diarrhea (black, tarry), or hematochezia (bleeding from rectum) Fecal incontinence Inability to control bowel movements Psychological factors - confusion, anxiety, disorientation Physiologic - neurological / motor impairment Changes begin before 50 y/o Oral changes (tooth decay) may lead to difficulty with digestion Sensory changes - decreased taste buds which can contribute to depressed appetite Salivary secretions decrease - dry mouth, difficulty with digestion Organs lose tone but manage to function well enough Net effect of changes includes decreased alimentary mobility (increased constipation), decreased blood flow, decreased nutrient absorption> slower digestion and emptying There is a decline in “Intrinsic Factor” (IF) that typically promotes vitamin B12 absorption in the stomach; this frequently occurs after middle age. In advanced age (90 y/o), prevalence of problems associated with B12 deficiency is as high as 90% (anemia, neurological symptoms, constipation, weight loss) Hiatal Hernia Definition & Incidence: lower esophageal sphincter gets enlarged and stomach passes through the diaphragm into the thoracic cavity Estimated incidence of 5/1000 people / year Prevalence estimated at 60% of people over 60 y/o (symptomatic and asymptomatic) Etiologic / risk factors - anything that weakens the diaphragm muscle or alters the hiatus Pathogenesis / Clinical Manifestations: heart burn - worse when lying down or with increased abdominal pressure Medical Management: diagnosed by ultrasound imaging or barium swallow with fluoroscopy; treatment includes symptomatic control Gastroesophageal Reflux Disease (esophagitis) (GERD) Definition & Incidence: inflammation of esophagus; increasing incidence with aging; 15% or more of the population may have symptoms daily Types: reflux, chemical, infectious Etiologic / risk factors: backward flow of stomach acids; irritation by nasogastric intubation or radiation GERD (continued) Pathogenesis / Clinical Manifestations: Heart burn, belching, dysphagia; problem is that long term GERD can result in Barrett’s esophagus (metaplasia - dysplasia) which increases risk for neoplasia GERD (continued) Medical Management: diagnosis with history, endoscopy, barium radiography, H-pylori, esophageal pH Can be confused with angina; Nitroglycerin can help determine cardiac vs. GERD pain (but not without error - some GERD goes away with nitroglycerin) Treatment includes acid suppression, lifestyle modifications - drinking fluids between meals but not with meals, loose fitting clothes, avoiding caffeine, nicotine, alcohol, aspirin, NSAIDs, remaining upright for at least 3 hours after meals, weight loss if obese Minimally invasive surgery is being developed Mallory-Weiss Syndrome Mucosal laceration of the lower end of esophagus accompanied by bleeding. It is commonly caused by retching and vomiting due to alcohol abuse, eating disorders or a viral syndrome Diagnosis is made with endoscopy Treatment with fluid replacement, blood transfusion Endoscopic ligation may be required Neoplasm Definition & Incidence Two types - squamous cell and adenocarcinoma Adenocarcinoma is relatively uncommon but incidence is rising (H-pylori treatment might be reason) Etiologic / risk factors: irritation, any change in function that keeps food in the esophagus longer than it should that results in ulceration and metaplasia Neoplasm (continued) Clinical Manifestations - dysphagia is the primary sign / symptom, but it does not present until the esophagus is blocked between 30-50%; the only pain tends to be heartburn with lying down Neoplasm (continued) Medical Management - prevention by treatment of irritation / GERD, etc.; diagnosis with endoscopy Neoplasms are classified as resectable with curative intent, resectable but not curable, and not resectable/not curable; (depends on metastases, lymph node involvement) Prognosis is poor - 5 year survival is 10%, with a median survival of less than 10 months (related to the lack of symptoms / signs until relatively late in the process) Esophageal Varices Dilated veins in the lower third of esophagus immediately beneath the mucosa due to portal hypertension usually associated with cirrhosis of the liver; usually painless but significant bleeding that can result in anemia and other low blood volume problems (in extreme cases shock) About 1/2 cease without intervention; ligation may be needed; in extreme cases a stent may be required to relieve portal hypertension Congenital Conditions Tracheoesophageal Fistula TEF - most common congenital esophageal anomaly; about 1 in 4000 live births; esophagus fails to make connection to the stomach : might go to trachea and then stomach; or trachea alone; or just end blindly with or without trachea making a connection to stomach requires surgical repair WHAT does this condition cause?? Depends on type See page 840 in Goodman Gastritis Definition & Incidence - inflammation of the lining of the stomach; represents a group of the most common stomach disorders; can be acute or chronic; most common form of chronic gastritis is caused by a bacterial infection: H-pylori Etiologic / risk factors: serious illness, medication use (ASA, NSAID), stress, H-pylori Clinical Manifestations - epigastric pain; can lead to GI bleeding Medical Management - Dx by history, endoscopy, biopsy, tests of stool or blood for H-pylori; Rx, remove cause if possible, time to heal Peptic Ulcer Disease PUD Definition & Incidence - break in protective mucosal lining which exposes submucosal areas to gastric contents/secretions Two types – gastric (stomach) or duodenal (DUs are 2-3 x more prevalent) Etiologic / risk factors: anything that causes gastritis Clinical Manifestations: epigastric pain - with burning, gnawing, cramping, aching near xiphoid coming in waves; can include nausea, loss of appetite and weight loss. Perforation causes increased pain in thoracic spine area T6-T11 with radiation to RUQ Medical Management: Dx: same as gastritis; Rx - same as gastritis; surgical intervention is required for perforation Gastric Cancer 1. Primary gastric lymphoma (relatively uncommon) 2. Gastric Adenocarcinoma - malignant neoplasm originating from gastric mucosa Etiologic / risk factors - chronic gastritis Clinical Manifestations - - depends on variety of factors such as size of tumor, presence of gastric outlet obstruction, metastatic versus nonmetastatic disease Medical Management - Dx is usually delayed due to symptomatic treatment of gastritis (early stages may be asymptomatic) Surgery is treatment of choice; prognosis depends on stage when discovered Gastric cancer (continued) Prevention: presently best advice is to eat at least 5 (1/2) cup servings of fruit and vegetables/daily combined with exercise, maintenance of healthy weight and reduced intake of salt-preserved foods Congenital Conditions Pyloric Stenosis (PS) - obstruction of pyloric sphincter (stomach into duodenum) Clinical Manifestations - projectile vomiting is the most common and dramatic early sign - and may occur at birth Projectile vomiting requires vomit to eject 1 foot or more when supine, or 3-4 feet when upright Medical Management - antispasmodic medications (if effective) for 6-8 months to see if stenosis loosens up; if it does not loosen up surgical repair is required Malabsorption Syndrome Definition & Incidence - group of disorders (celiac disease, cystic fibrosis, Crohn’s disease, chronic pancreatitis, pancreatic carcinoma, pernicious anemia, short gut syndrome, fibrotic changes due to gastroenteritis) characterized by reduced intestinal absorption of dietary components and excessive loss of nutrients in the stool Malabsorption syndrome (continued) Traditionally classified as: Maldigestion- failure of chemical process of digestion Malabsorption- failure of intestinal mucosa to absorb nutrients Can occur separately or together simultaneously Malabsorption syndrome (continued) Etiologic / risk factors - most often in therapy will see patients with gastroenteritis due to NSAID use and resultant fibrotic changes leading to malabsorption Malabsorption syndrome (continued) Clinical Manifestations - Progressive - related to nutrient deficiency General malaise - weakness, fatigue, muscle wasting B12 - pernicious anemia Iron, vit A, D, K - osteomalacia Calcium, vit D, magnessium - tetany Vit B complex - Numbness and tingling Electrolytes - muscle spasms, palpitations Vit K - easy bruising / bleeding Protein - generalized swelling Malabsorption syndrome (continued) Medical Management - treat underlying condition; nutritional supplementation – may need to bypass GI (parenteral nutrition - IV feeding); prognosis depends on underlying condition Vascular Diseases Embolic occlusions of visceral branches of abdominal aorta Intestinal Ischemia - caused by atherosclerosis or emboli; pain, rapid onset of cramping Rx - surgery Bacterial Infections Food borne illnesses such as botulism are caused by bacteria. Can be fatal. Appropriate treatment depends on identifying pathogen. Many episodes of acute gastroenteritis need fluid replacement and supportive care. Inflammatory Bowel Disease (IBD) Definition & Incidence 1. Crohn’s disease (CD) - chronic, life long inflammatory disorder that can affect any segment of the intestinal tract with “skips” (sections of normal bowel with skips or lesions) 2. Ulcerative colitis (UC) - chronic inflammatory disorder of the mucosa of the colon in a continuous manner –chronic diarrhea and rectal bleeding IBD (continued) Etiologic / risk factors - both have unknown etiologies Pathogenesis - both are considered autoimmune Clinical Manifestations - recurrent involvement of intestinal segments resulting in a chronic, unpredictable course Inflammatory process begins with low-grade fever, malaise, weight loss, diarrhea and abdominal cramping / pain; may be followed by obstructive phase with persistent bloating and distention from the movement of gas through the system IBD (continued) Medical Management - Dx only by history and ruling out other conditions; monitoring includes use of radiographs, colonoscopy, barium enema x-ray, fecal occult blood tests, blood testing Rx: symptom relief, anti inflammatory meds, diet, surgery to resect parts of intestine may be necessary Antibiotic Associated Colitis Antibiotics can disrupt normal GI bacterial flora; common for C - difficile (Clostridium difficile) to dominate; it is a microorganism that can replace normal GI tract flora It is not invasive, but can create toxins that damage the colonic mucosa; signs start as a lot of watery diarrhea - can occur early with antibiotic treatment or within 4 weeks after the medications have stopped. Treatment is aimed at fluid and nutrition replacement, and antimicrobials can be prescribed to treat the c-diff Irritable Bowel Syndrome (IBS) Definition & Incidence - group of symptoms most common disorder of the GI system Referred to as ‘nervous indigestion’, ‘spastic colon’, ‘nervous colon’ and ‘irritable colon’ There is absence of inflammation; it should not be confused with Crohn’s or Ulcerative colitis (It is not as severe - there are no structural or biochemical defects identified) IBS (continued) Etiologic / risk factors - three main functional abnormalities: 1. altered GI motor activity; 2. visceral hypersensitivity; 3. altered processing of information by the nervous system IBS (continued) Clinical Manifestations - Abdominal pain that is relieved by a bowel movement, bloating, distention, passage of mucus, changes in stool form (hard or loose and watery), alterations in stool frequency, or difficulty in passing a movement Medical Management - Dx - history; no test. Rx aimed at symptoms, lifestyle changes (dietary), stress reduction, behavior therapy (to identify and reduce triggers) Diverticular Disease Diverticulosis - outpouchings in intestinal wall, uncomplicated Diverticulitis - inflammed outpouching, complicated Asymptomatic in 80% of people with diverticulosis; when inflammed - severe pain Treatment to relieve symptoms, prevent diverticulitis; if diverticulitis may need antibiotics and complete rest of colon with naso gastric tube feedings and IV fluids until inflammatory process has been resolved Diverticular disease (clarified) *outpouching is called diverticula The presence of diverticula in wall of colon or small intestine describes the herniation of mucosa through the muscles of the colon It is when food particles or feces become trapped in diverticula and become infected and inflammed >>> diverticulitis Rarely reversible Neoplasms Intestinal Polyps - growth or mass in wall of intestines Benign Tumors (most common adenomas, leiomyomas, lipomas) - Rarely become malignant; only need to be treated if causing symptoms Malignant Tumors Adenocarcinoma - (colorectal cancer) second leading cause of cancer death in US men and women combined; they have a long pre-invasive phase; few early warning signs - rely on medical screening with colonoscopy; persistent change in bowel habits is the single most consistent symptom Rx: surgical removal Obstructive Disease Definition & Incidence - anything that reduces the size of the gastric outlet, preventing normal flow of chyme and delaying gastric emptying Leads to: distention, cramping pain, tenderness that progresses to point of being constant, vomiting due to reflux, constipation, signs of dehydration, hypovolemia After ~ 24 hours of complete obstruction, impaired blood supply can lead to necrosis and strangulation; can cause fever, leukocytosis, peritoneal signs or blood in feces Obstructive Disease (continued) Three causes: Organic, mechanical, functional 1. Organic: due to another condition 2. Mechanical Obstruction Adhesion - scar tissue from surgeries Intussusception - telescoping of intestines on itself (Figure 16-17) Volvulus - twisting Hernia - protrusion of intestines through the groin, abdomen, navel (weakness in muscle and connective tissue normally containing it) 3. Functional Obstruction Adynamic or Paralytic Ileus - neurologic or muscular impairment of peristalsis Oglvie’s Syndrome - Acute colonic pseudoobstruction early postoperatively following trauma to hip, pelvis, or after elective hip or pelvic surgery; etiology unknown - but thought to be related to disruption to sacral parasympathetic nerves (S2-S4 supply colon and rectum) Congenital Conditions Stenosis & Atresia - stenosis - narrowing of small intestine; atresia is a defect caused by incomplete formation of lumen Meckels Diverticulum - outpouching of the bowel located at the ileum of small intestine Definition & Incidence - inflammation of the vermiform appendix that often results in necrosis and perforation and subsequent peritonitis Etiologic / risk factors - 1/2 no known cause; 1/3 due to obstruction of some type that prevents drainage (what is the other 1/6 is caused by?) Pathogenesis - obstruction -> infection; or just infection Clinical Manifestations - constant pain RLQ, n&v ; children - fever; adults - mild fever; aggravated by anything that increase abdominal pressure Can present atypically “Pinch an inch” test > rebound test Medical Management - remove appendix Peritonitis Definition & Incidence - inflammation of peritonium – serous membrane lining the wall of abdominal cavity; if spontaneous >primary; if due to trauma, surgery, peritoneal contamination from a perforation > secondary. Etiologic / risk factors - primary ?; secondary, trauma, surgery, GI issue that leads to perforation Clinical Manifestations - decreased GI motility and distention with gas; vague generalized abdominal pain; as progresses becomes severe pain and abdomen becomes rigid (involuntary guarding), n&v, fever Medical Management - infection control, and treat consequences Rectal (or anal) Fissure Ulceration or tear of lining of the anal canal usually caused by excessive tissue stretching or tearing such as during childbirth or a large, hard bowel movement; tends to reopen frequently Heal within a month or two - may need stool softeners to help facilitate healing by preventing re injury Rectal Abscesses and Fistulas Abscesses (infection) or fistula (opening) can occur as a result of an infected anal gland, fissure or prolapsed hemorrhoid and are most common in people with Crohn’s disease Hemorrhoids “piles” Varicose veins of a pillow like cluster of veins that lie just beneath the mucus membrane at the lowest part of the rectum - associated with anything that increases intra-abdominal pressure (Box 16-1); internal hemorrhoids may require ligation (tying up), sclerosing (shrinking the vessels) , laser or cryosurgery to destroy the tissue; external can be treated with local applications of topical medications, high fiber diet, avoidance of constipation 1. The Digestive System Diagram, Organs, Function, and More - WebMD www.webmd.com/digestive-disorders/digestive-system 2. Upper GI Tract Anatomy - eMedicine World Medical Library emedicine.medscape.com/article/1899389-overview 3. Gut. 2004 February; 53(2): 310–311. 4. Evolution Of The Human Appendix: A Biological 'Remnant' No More www.sciencedaily.com/releases/2009/08/090820175901. htm 5. Achalasia — Diagnosis and treatment at Mayo Clinic www.mayoclinic.org/achalasia/ Emotional Support Animals Andrea C. Mendes PT, DPT Sean M. Collins PT, ScD