Pelvic Ring Fractures
advertisement

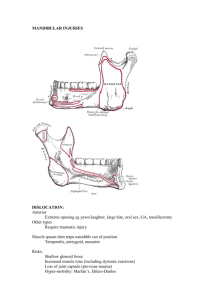
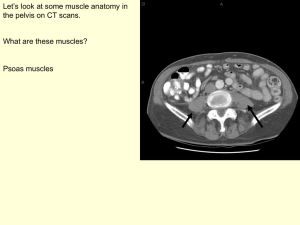
+ Pelvic Ring Fractures Christy Johnson + Outline Background Anatomy and Function Assessment Radiology Classification Treatment + Background Mechanism: high energy blunt trauma Mortality rate: 15-25% for closed fractures Up to 50% for open fractures Hemorrhage is the leading cause of death overall Venous (80%) > arterial Have a high index of suspicion for injury of internal iliac vessels or lumbosacral plexus + Background Associated injuries: Chest injury (63%) Long bone fracture (50%) Head and abdominal injury (40%) Spine fractures (25%) Urogenital injuries in 12-20% Survivors: 1.89 additional injuries Non-survivors: 2.95 additional injuries Only 2 in 14 deaths (14%) are directly attributable to pelvic injury + Anatomy: Osteology Ilium Sacrum Pubis Femur Ischium + Osteology Ring structure made up of the sacrum and two innominate bones No inherent osseous stability + Anatomy: Muscles Iliacus Piriformis Pectineus Sartorius Rectus femoris Adductor longus Adductor brevis Adductor magnus + Ligaments Anterior structures: provide 40% of stability Posterior structures: provide 60% of stability + Pelvic Stabilizers Sacrospinous Ligament: Resist ER Iliolumbar: Augment posterior stability Sacrotuberous Ligament: Resist ER and Vertical shear Posterior interosseous sacroiliac ligaments are the strongest in the body + Assessment Primary Survey Airway Breathing Circulation Disability Exposure Secondary Survey Pelvis assessed by compression/distraction Skin evaluation Smith/Johnson/Cothren et al Journal of Trauma 2007 + Resuscitation/ Hemorrhage 2 large-bore IVs 2L crystalloid on arrival Hct/Hgb does NOT correspond to EBL Hypotension = 3040% EBL Patients presenting in shock (SBP<90) have mortality rates up to 10 times that of normotensive patients Starr et al JOT 2002 + Sites of Hemorrhage External bleeding controlled by direct pressure Thoracic cavity evaluated by CXR for hemothorax: chest tube if necessary Abdominal cavity evaluated by a FAST or CT scan in stable patients or ex-lapin unstable patients If other causes eliminated, then EBL likely from pelvis Blood replacement as indicated by response to fluid resuscitation Ratio of FFP: PRBC/ 1:1.5 associated with decreased mortality and transfusion requirements Injury 2010 + Physical Exam Test stability by placing gentle rotational force on each iliac crest Perform ONCE Look for external rotation of lower extremity +/- limb-length discrepancy + Physical Exam (continued) Neurologic exam L5 and S1 injuries most common Rectal exam to evaluate sphincter tone and perirectal sensation Urogenital exam Concomitant urologic injury 12% of the time Catheter placement should be preceded by rectal exam, evaluation of meatus, vaginal exam 57% of men with urethral injury show no signs Vaginal injuries missed in up to 50% of cases Vaginal and rectal exams Mandatory to rule out occult open fracture + Radiographs AP Pelvis Inlet Outlet Oblique/Judet Obturator oblique Iliac oblique + Mechanisms of Pelvic Injury Anterior Compression Lateral Compression Vertical Shear Combined mechanism Young and Burgess, Rad 1986 Young and Burgess J Trauma 1989 + AP Compression + Anteroposterior Compression Type Definition APC1 Symphysis widening < 2.5cm APC2 Symphysis widening > 2.5 cm. Sacrotuberous, sacrospinous and anterior SI joint ligaments are disrupted. Posterior SI ligaments intact. APC3 Disruption of anterior and posterior SI ligaments. Disruption of sacrospinous and sacrotuberous ligaments + Lateral Compression + Lateral Compression Type Definition LC1 Oblique or transverse ramus fracture and ipsilateral anterior sacral ala compression fracture LC2 Rami fracture and ipsilateral posterior ilium fracture dislocation (crescent fracture) LC3 Ipsilateral lateral compression and contralateral APC (windswept pelvis). Common mechanism: rollover vehicle or peds struck + Vertical Shear + Vertical Shear Associated with the highest risk of hypovolemic shock, mortality Usually result from falls from height Posterior and superior directed force APCIII + vertical displacement + Mortality from Pelvic Injuries Hemodynamic instability + pelvic fracture = 40% mortality Major cause of death: Hemorrhage (15%) Major cause of death LC injuries: closed head injuries Major cause of death APC: combined pelvic and visceral injuries Hemorrhage in pelvic injuries Venous bleeding more common than arterial bleeding Superior gluteal artery (most common arterial injury in APC) Internal pudendal artery (most common in LC) Metz et al Orthop Clin N Am 2004 Smith et al J Trauma 2007 + Circumferential Pelvic Antishock Sheeting Rapid, inexpensive, temporary means of decreasing pelvic volume Indications: initial management of an unstable ring injury Risk of bladder injury in pelvic fractures with internal rotation component (i.e. LC injuries) Technique: center over greater trochanters (NOT iliac crest/abdomen) + External Fixation Advantages: Indications: Pelvic ring injuries with an external rotation component (APC, VS) Unstable ring injury w/ ongoing blood loss Contraindications Decreases pelvic volume Stabilization of pelvis Ilium fracture that precludes safe application Acetabular fracture Technique: Iliac wing or supraacetabular pins Egbers Orthopade 1992 + Angiography/ Embolism Small percentage of pelvic fractures have significant arterial injuries amendable to angio (10%) Must have stabilized pelvis (pattern or ex-fix) because most bleeding is venous which will tamponade Eliminate other sources of bleeding Successful in 70-90% of cases but takes 3-4hrs + Treatment Overview Nonoperative Indicated for mechanically stable pelvic ring injuries LC1: anterior impaction fracture of sacrum and oblique ramus fx with <1cm of posterior ring displacement APC1: widening of symphysis <2.5 cm with intact posterior pelvic ring Isolated pubic ramus fx Operative Anterior ring stabilization: Symphyseal fixation Posterior ring stabilization Anterior or posterior SI joint fixation Sacral bar Iliac wing fixation + Treatment Comparison Technique Pro Con Pubic Symphysis Plating Can be done simultaneously w/ laparotomy Only stabilizes anterior ring Posterior approachORIF Visualization of reduction and sacral screw placement; limits risk of neurologic injury Prominent hardware complications Anterior approach – ORIF Allows for placement of multiple plates across the SI joint Risk of L4 and L5 injury Percutaneous Good for sacral fx and Neurologic injury; Iliosacral SI dislocations; low soft technically demanding screw tissue complications + Tenets of Fixation Complete instability of posterior ring: Complete instability of posterior ring with vertical (cephalad) displacement Anterior fixation alone is inadequate for maintaining reduction Posterior fixation should be supplemented with anterior stabilization Posterior injury is regarded as the more critical and in need of accurate reduction with stable fixation Reduction generally proceeds from back to front + Summary Pelvic ring injuries are highly associated with other injuries Evaluation of pelvic stability is critical and requires an understanding of mechanism of injury, a careful examination, and scrutiny of radiographic imaging Management requires an interdisciplinary approach and may be life saving + Questions? Thanks to: Dr. Helfet Matt Griffith Chris Mattem Milton Little