Higher Human Biology unit 2 section 4 CARDIOVASCUL
advertisement

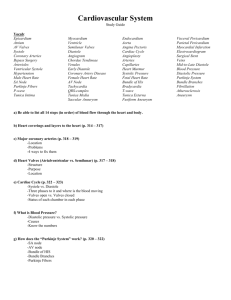
• 2 The cardiovascular system • (a) The structure and function of arteries, capillaries and veins to include endothelium, central lumen, connective tissue, elastic fibres, smooth muscle and valves. The role of vasoconstriction and vasodilation in controlling blood flow. Structure of the Cardiovascular System What is the Cardiovascular system? • The cardiovascular system, also known as the circulatory system, is composed of blood, blood vessels and the heart. • The heart functions as a pump to move blood through the blood vessels of the body. • A circulatory system is essential for large, multi-cellular organisms, such as humans and animals, and provide at least five major functions that are necessary for life. The five major functions of the cardiovascular system are: • Transporting oxygen and removing carbon dioxide • Transporting nutrients and removing wastes • Fighting disease • Transporting hormones • Regulating body temperature Cardiovascular system • http://www.youtube.com/watch?v=CjNKbL_-cwA Components of the CVS • The CVS consists of a double pump (the heart) and a complex system of blood vessels. The cardiovascular system • The cardiovascular system is made up of the heart along with the blood vessels. Blood vessels A layer of cells called the endothelium lines the central lumen of all blood vessels. It is surrounded by layers of tissue. These surrounding layers differ in each type of blood vessel. The middle of the vessel is called the central lumen. ARTERIES • Carry blood away from the heart • Endothelium • One cell thick • Elastic tissues & smooth muscles • Rebounds • Evens flow • Fibrous tissue • Tough • Resists stretch Contraction of the smooth muscle: vasodilation and vasoconstriction Arteries • Arteries carry blood away from the heart. The further the blood travels away from the heart, the lower the blood pressure gets. • They have an outer layer of connective tissue containing elastic fibres and a middle layer containing smooth muscle with more elastic fibres. The elastic walls of the arteries stretch and recoil to accommodate the surge of blood after each contraction of the heart. • The smooth muscle can contract, called vasoconstriction. This decreases the blood flow. It can also relax, causing vasodilation. This increases blood flow. Movement of these muscles controls blood flow. VEINS • Carry blood towards the heart • Endothelium • Larger lumen than arteries • Thinner muscle layer & few elastic fibres • Blood at lower pressure • Fibrous tissue VEINS • Contain valves • Prevents backflow of blood • Situated between skeletal muscles • Muscle compresses vein when contracted • Blood “squirted” towards heart Veins • Veins have an outer layer of connective tissue containing elastic fibres but a much thinner muscular wall than arteries. They contain valves to prevent back flow of blood as blood is at a lower pressure in veins than arteries. CAPILLARIES • Transport blood between arteries and veins • Form large networks (capillary beds) • Exchange of materials between blood and cells • Their walls are only one cell thick, allowing nutrients and waste to diffuse through with ease. Capillaries Arteriole Capillaries (capillary bed) Venule Capillaries • Capillaries are only one cell thick to allow exchange of substances with tissues. • (i) The exchange of materials between tissue fluid and cells through pressure filtration and the role of lymph vessels. • Similarity of tissue fluid and blood plasma with the exception of plasma proteins. Tissue Fluid and the Lymphatic system Lymphatic system • http://www.youtube.com/watch?v=Q530H1WxtOw Comparison of contents of plasma and tissue fluid Plasma Tissue fluid Protein e.g. red blood cells No protein Oxygen and carbon dioxide Oxygen and carbon dioxide glucose, amino acids glucose, amino acids water water Tissue fluid • Dissolved substances move out through the capillary walls by pressure filtration, forming tissue fluid. Tissue fluid is similar to blood plasma except it does not contain plasma proteins e.g. red blood cells. Tissue fluid surrounds cells and supplies them with glucose, amino acids, oxygen and other useful substances. Carbon dioxide and other metabolic waste (waste produced by chemical reactions in the cell) diffuse out of the cells and into the tissue fluid to be excreted. Summary Tissue Fluid and Lymphatic System Lymph passes into lymphatic system Lymph vessel Blood leaving in venule low pressure Some tissue fluid enters capillary by osmosis Some tissue fluid enters lymphatic system Blood arriving in the arteriole high pressure capillary Some plasma forced out of capillary Respiring cell Tissue fluid • Case study on disorders of the lymphatic system. Suitable examples include the effect of kwashiorkor on fluid balance and elephantiasis. Lymphatic system • Excess tissue fluid is absorbed by lymphatic vessels which are found around cells in each tissue, forming lymph fluid. The lymph fluid eventually returns to the blood. • (b) The structure and function of the heart. • (i) Cardiac function and cardiac output. • Definition of cardiac output and its calculation. Cardiac Function and Cardiac Output Heart Rate (HR) • Number of times heart beats in one minute • Normal values around 72bpm • Normal range is between 60-90 Stroke Volume (SV) • Volume of blood ejected by each ventricle during contraction • The heart pumps the same volume of blood through the ventricles during each beat. • ~ 70ml Cardiac Output Cardiac Output is the volume of blood pumped by each ventricle per minute and is the function of two factors: • Heart rate (beats per minute) • Stroke volume (the volume of blood ejected by each ventricle during each contraction) CO = HR x SV • Measuring pulse rate in arteries using pulsometer. Calculate cardiac output under different conditions. Some typical values for cardiac output at varying levels of activity Activity Level Heart rate (bpm) Stroke Volume (ml) Cardiac Output (l/min) Rest 72 70 5 Mild 100 110 11 Moderate 120 112 13.4 Heavy (athlete) 200 150 30 Cardiac output • Heart rate (HR) = number of beats of the heart per minute (bpm) • Stroke volume (SV) = volume of blood ejected by each ventricle during contraction (ml). The left and right ventricles pump the same volume of blood through their arteries each time. • Cardiac output (CO) measures the volume of blood pumped out by each ventricle per minute. To calculate this: CO = HR x SV • http://www.phschool.com/science/biology_place/labbench/lab10/int ro.html Cardiac function The Heart Atrioventricular valve Semi-lunar valve Atrioventicular valve Semi-lunar valve • The opening and closing of the AV and SL valves are responsible for the heart sounds which can be heard with a stethoscope. • (ii) The cardiac cycle to include the functions atrial systole, ventricular systole, diastole. Effect of pressure changes on atrio-ventricular (AV) and semi lunar (SL) valves. THE CONDUCTING SYSTEM OF THE HEART Stuart brown – stooibrown@yahoo.com • Cardiology. As a youngster I had a cardiac pacemaker. Two, actually. I still have one of them, plus the x-ray of the damn thing in my chest. So I can talk a bit about what it did for me (and what it didn't do) and the sorts of tests which were done on me to examine my heart's performance. Cardiac cycle • 1. 2. 3. The cardiac cycle consists of three stages: Atrial systole Ventricular systole Diastole Cardiac cycle 1. Atrial systole Pressure in the atria builds up as muscles of the atria walls contract, forcing blood through the AV valves into the ventricles. AV valves open, SL valves shut. 2. Ventricular systole Pressure in the ventricles build up as muscles of the ventricle walls contract, forcing blood through the SL valves into the arteries. SL valves open, AV valves shut. 3. Diastole Pressure decreases in both atria and ventricles as muscles relax. Blood flows back into the atria and starts to flow into the ventricles. The higher pressure in the arteries closes the SL valves. AV valves open, SL valves shut. Pure Science Specials - Of Hearts and Minds • https://www.youtube.com/watch?v=Xwx5fbElMfk • 50 mins • (iii) The structure and function of cardiac conducting system including nervous and hormonal control. • Control of contraction and timing by cells of the sinoatrial node (SAN) and atrio-ventricular node (AVN). Interpretation of electrocardiograms (ECG). • The medulla regulates the rate of the SAN through the antagonistic action of the autonomic nervous system (ANS). Sympathetic accelerator nerves release adrenaline (epinephrine) and slowing parasympathetic nerves release acetylcholine. Regulation of the Cardiac Cycle Sino-atrial node (SAN) and Atrial Ventricular node (AVN) Electrical activity of the heart • http://www.youtube.com/watch?v=v3b-YhZmQu8&feature=related Cardiac conducting system • The heart beat is regulated by both nervous and hormonal control. • Nervous control: • Cells of the sino atrial node (SAN), also known as the pacemaker, in the right atrium set the pace at which cardiac cells contract without conscious thought. They are called autorhythmic. • The SAN generates an electrical impulse which spreads throughout the atria, causing atrial systole. The impulse reaches the AVN which then carries the impulse across the ventricles, causing ventricular systole. Autonomic Nervous System • The autonomic nervous system (ANS) consists of 2 antagonistic (opposing) branches • Sympathetic nerve • Parasympathetic nerve Sympathetic Sympathetic accelerator nerves Release adrenaline (epinephrine) Increases heart rate Parasympathetic Parasympathetic slowing nerves Release acetylcholine Decreases heart rate The medulla region in the brain regulates the rate of the SAN through the Autonomic Nervous System (ANS). It contains two branches which work in Antagonistic (opposing) ways. Sympathetic accelerator nerves release adrenaline (epinephrine) which increases heart rate. Slowing parasympathetic nerves release acetylcholine which decreases heart rate. ABPI schools • Adrenaline animation: • http://www.abpischools.org.uk/page/modules/hormones/horm8.cfm ?coSiteNavigation_allTopic=1 Hormonal Regulation of the Heart • Under certain circumstances e.g. stress or exercise the sympathetic nervous system causes the adrenal glands to produce adrenaline which travels in the blood to act on the SAN, which generates impulses at a higher rate, increasing heart rate Hormonal Regulation of the Heart • Under certain circumstances e.g. stress or exercise the sympathetic nervous system causes the adrenal glands to produce adrenaline which travels in the blood to act on the SAN, which generates impulses at a higher rate, increasing heart rate • Hormonal control: • Under circumstances such as stress and exercise, the sympathetic nervous system causes the adrenal glands to produce the hormone adrenaline which acts on the SAN to increase heart rate. • The impulses generated by the SAN creates currents that can be detected by an electrocardiogram (ECG). • P wave – atrial systole • QRS waves – ventricular systole • S wave - diastole ABNORMAL ECG’S • Atrial flutter • Rapid contraction of the atria • Atria contract 3 times for every ventricular contraction ABNORMAL ECG • Ventricular tachycardia • Ventricles beat rapidly and independently of the atria ABNORMAL ECG’S • Ventricular fibrillation • Unco-ordinated electrical activity • Pumping cannot take place • Fatal if not corrected • Defibrillation • (iv) Blood pressure changes, in response to cardiac cycle, and its measurement. • Blood pressure changes in the aorta during the cardiac cycle. Measurement of blood pressure using a sphygmomanometer. A typical reading for a young adult is 120/70 mmHg. Hypertension is a major risk factor for many diseases including coronary heart disease. blood pressure measurement • http://www.youtube.com/watch?v=ElCbQMiBC6A&NR=1 Blood pressure • Blood pressure changes in the aorta during the cardiac cycle. It can be measured using a sphygmomanometer. • An inflatable cuff stops blood flow and deflates gradually. The blood starts to flow (detected by a pulse) at systolic pressure. The blood flows freely through the artery (and a pulse is not detected) at diastolic pressure. • A typical reading for a young adult is 120/70 mmHg. High blood pressure, known as hypertension, is a major risk factor for many diseases including coronary heart disease.