Sports Injuries in the Aging Athlete
advertisement
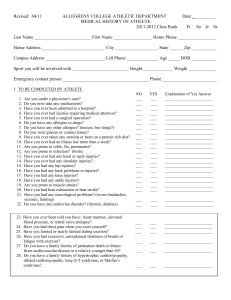
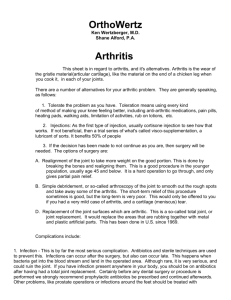
Common Problems of the Aging Athlete Brian L. Badman M.D. Orthopedics and Sports Medicine of Indiana Hendricks Regional Health Rotator Cuff Injuries Rotator Cuff Anatomy 4 muscles/tendons Supraspinatus Infraspinatus Teres Minor Subscapularis Rotator Cuff Function Shoulder rotation Arm elevation Helps keep humeral head within shoulder socket Rotator Cuff Injuries The position of injury for the rotator cuff is overhead WHY? Rotator Cuff Injuries Overhead Position Impingement between humerus and acromion Least efficient/weakest position for cuff Poor blood supply to tendons Rotator Cuff Injuries What causes the injury? Trauma Fall on an outstretched hand Arm forcefully pulled to side or downward Overuse Repetitive lifting, loading Traumatic Causes Tear of Tendons Partial Complete Overuse Causes Chronic Inflammation Bursitis Fraying Gradual progression of tear ONCE TEARING STARTS IT IS EASIER TO PROGRESS Why Does it Worsen? Weakened cuff cannot protect itself Space between acromion and humerus narrows Impingement worsens Tear progresses Watershed Region/Zone of Injury Torn Rotator Cuff Symptoms Pain in deltoid region Upper outer arm Pain worse with overhead activities Night pain Pain with exertion Lifting Symptoms MUST ALWAYS EVALUATE NECK AS SYMPTOMS FROM A HERNIATED DISK CAUSING NERVE IMPINGEMENT ARE SIMILIAR Evaluation History Physical Examination MRI Evaluation History Trauma, location, provocation of symptoms Exam Pain with isolated cuff testing Impingement signs Weakness Evaluation MRI NEED HIGH QUALITY MAGNET! Insurance will pay the same so might as well insist on best quality study Your doctor may not be aware that this is important so stress the need for a CLOSED MRI unless you are claustrophobic In-office Open MRI POOR QUALITY STUDIES Treatment If have a partial tear or cuff just inflamed (bursitis, tendonitis) Physical Therapy NSAIDS (Motrin, alleve, advil, celebrex) +/- Steroid Injection Rest Avoid overhead activities and lifting It may take several months for pain and inflammation to resolve Rotator Cuff Exercises Rotator Cuff Exercises: High Level Treatment Complete Tear In active individuals surgery is generally indicated Rotator cuff will not heal itself Results are better if a traumatic tear is fixed acutely (2-3 weeks) Takes 12 weeks for repair to heal to bone Anticipate a year to recover 3 monthsbegin overhead activities 6 monthsMay resume most activities as long as motion is good Postop Rehab Because the cuff heals slowly (12 weeks minimum) the repair is easily damaged if stressed too soon after surgery Slow progression with motion and strengthening is necessary May result in stiffness Usually resolves but may take entire year to return Goals of Surgery Repair tear Alleviate pain Maintain full ROM Maintain strength Surgery Arthroscopic Open Healing times are the same! Surgery Arthroscopic Less pain Small incisions ?Less stiffness Some tears are not repairable thru the scope Some tears are not repairable at all! Arthroscopic Surgery Acromioplasty Make more room for repair and eliminate spurs that may have predisposed to tear Arthroscopic Surgery Place anchors with sutures attached Knee Injuries: Diagnosis, Treatment and Prevention Anatomy Definitions Ligaments: Connect bones around joints, Provide joint stability Check reins Tendons: Anchor muscles to bones Cords Bones: Structural Supportsscaffold Articular Cartilage: Gliding Cartilage, Low friction smooth surfaceCovers Bone Meniscal Cartilage: Cushion Cartilage Shock absorber Anatomy Ligaments ACL: Anterior Cruciate Ligament PCL: Posterior Cruciate Ligament MCL: Medial Collateral Ligament LCL: Lateral Collateral Ligament Bone Provides structural support Attachment Site for muscles, ligaments tendons Bursa: Fluid filled sack covering bone, reduces friction Bursitis: Inflammation of the sack due to trauma, excess friction Subject to fracture and bruising with trauma Tendons Connect muscle to bone Glide in confined spaces Subject to friction Leads to inflammation when overused Trainable, Adapt to use Articular Cartilage Gliding cartilage on joint surface Specialized low friction, shock absorbing material Lubricated by specialized fluid Arthritis: Wear and inflammation lead to roughening of the cartilage surface, less efficient more friction Articular Cartilage Injuries Can result from chronic wear or sudden injury Can delaminate at bone-cartilage interface Sx: Pain Swelling Popping Catching Locking Knee Arthroscopy Small incisions Camera placed into the joint Small instruments trim and smooth cartilage Operate using a video monitor Surgical Treatment Treatment New Treatments Autologous Chondrocyte Implantation (ACI) Grow your own cartilage and reinsert into the knee Larger 2 staged surgery Grows new gliding cartilage Prevention Difficult Injury/ Trauma avoidance Adequate sports preparation, muscle balance Jumping, landing skills Don’t ignore joint instability- increases risk of further injury to the cartilage Possible role for glucosamine, chondroitin Result Meniscal Cartilage Located between the femur and tibia Acts like a shock absorber in the knee Structurally different from articular cartilage Subject to tearing and can “pinch” in joint Meniscus Injuries Tears of the cushion cartilage in the knee Sx: Popping Sharp pain along joint Swelling Twisting pain Flexion, squat, stairs Locking if displaced Treatment Rest, Activity modification Strengthening, therapy, Steroid Injection +/Surgery for continued sx’s or recurrence Surgical Appearance Prevention Difficult, often part of the aging process Meniscus weakens, susceptible to tearing Stressed more with twisting, deep bending Routine low impact exercise Caution with deep flexion exercise Choose your parents well Knee Injuries Overuse injuries: Tendonitis, Bursitis Traumatic Injuries: Meniscus tears, Articular cartilage tears, Ligament tears, (Fractures) Cumulative Injuries: Arthritis Overuse Injuries Repetitive stress on de-conditioned tissues All tissues are injured with use and age Tissues repair themselves during rest periods Many injured tissues can regenerate with time Recurrent injuries with incomplete repair can accumulate resulting in inflammation Patellar Pathology Patellar/ Quad tendonitis Patellar Chondromalacia Patellar Instability Patellar Tendonitis Inflammation of a tendon Poor blood supply, slow to repair Over training or too rapid advancement in training Inadequate stretching Excess loads can lead to partial tearing Tendonitis Treatment RICE: Rest, Ice, Compression, Antiinflammatory medications Stretching, Deep tissue massage Reduce inflammation then gradual return to exercise Low impact, no jumping, Quadriceps strengthening, Physical Therapy Tendonitis Prevention Maintain good strength and flexibility Gradual advancement of activity Early intervention with injury or pain Ice, Motrin, Stretch, massage Reduce stressful activity Patellar Chondromalacia/Anterior Knee Pain Syndrome Pain in front of knee Worse with bending, stairs Grinding, crunching under knee cap Due to roughening of cartilage, malalignment Patellar Pain Treatment Reduce Inflammation Improve muscle balance, therapy, strengthening Bracing, taping patella Pain decreases as alignment improves Surgical options: Smooth cartilage, Realign patella to track more normally Surgical Treatment Prevention Improve muscle balance, quadriceps strength Avoid deep bending exercise (Patella stress goes way up) Minimize stair climbing, inclines Exercise on level surfaces Avoid leg extension machine Knee Ligament Injuries Strains or tears of the joint check reins MCL/ACL Tear most common in Knee Sx’s: Pain, swelling, decreased range of motion Later looseness, instability, giving way episodes Problems with cutting, twisting movements Too much motion of knee Both Men and Women at risk ACL Injuries Primary restraint to anterior tibial translation Essential to pivoting, cutting Involved in proprioception Limited capacity to repair after injury >200K injuries/year >100K reconstructions/year Ligament Injuries Noncontact ACL injuries Clear female predominance 2x soccer, 4x basketball FM:M Multifactorial causes: Decreased muscle protection, ACL size, narrow notch, menstrual cycle Mechanical: Valgus align, land in extension, less muscle co-contraction add tension to ACL Jumping, landing training can reduce risk Treatment Initially: Stop play, Ice, Compression, Crutches Motion, Leg raises Exam, Imaging studies Prehab Bracing Surgery ACL Surgery Most common ligament surgery Replace rather than repair Arthroscopic surgery Create new ligament from other tissues: Patellar tendon, Hamstring tendons Six months before return to play ACL Surgery ACL Surgery ACL Injury Prevention Adequate sports preparation (Skiing) Good Quad/Hamstring balance, tone Practice jumping, landing, twisting (Esp Females) Recognize fatigue and back off Knee braces don’t prevent injuries PCL Tears Less common than ACL Contact, tackle sports Often from fall on flexed knee, blow to anterior knee, posterior stress More easily compensated for than ACL TX: RICE, rehab, brace Surgery for multi-ligament injury (LCL, lat complex) MCL Tears Most common knee lig injury Cutting, twisting, blow to lateral knee, valgus stress Medial pain, varying degree of medial laxity on stress exam Tx: RICE, brace, motion, rehab, brace Iliotibial Band Syndrome Overuse/ friction bet IT band and Lat epicondyle Runners, cyclists, repetitive flexion activities During flexion ITB passes from ant to post to the lateral femoral epicondyle. Bursa reduces friction Causes: ITB tightness, varus, foot pronation, Internal tibial torsion, crossing midline at heel strike Clin: Lateral pain, may radiate, downhill, stairs Tx: Rice, ITB/hip stretch, NSAIDS, act mod, running technique changes Knee Arthritis Wear of the gliding articular cartilage (OA) Roughness increases gliding friction Sx: Pain, inflammation, swelling Pain with weather change, load bearing Improves with rest, antiinflammatory medicines, low impact exercise Arthritis Treatment Goal: Reduce pain, swelling, maintain motion, minimize disability, slow joint destruction Modalities: Anti-inflammatory meds, steroids, braces, cane, exercise Newer: Glucosamine/ Chondroitin tablets, Lubricating fluid injections (Hyalgan, Synvisc, Orthovisc, etc.), electromagnetic field currents? Surgery, Last resort Knee Replacement Remove worn cartilage surface Replace with metal and plastic bearing surface 6 month recovery 10-15 year longevity90% Arthritis Prevention Minimize trauma Regular low impact exercise Disease modifying agents on the horizon Vitamins/Anti-oxidants Glucosamine/Chondroitin