Causes and Diagnosis of Hypokalemia
advertisement

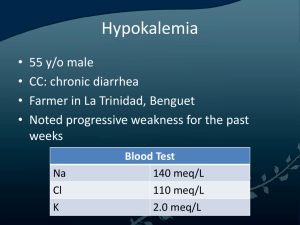
Diagnosis of Hypokalemia Mahmoud Barazi, M.D. Nephrology Fellow TTUHSC Case • 77 y.o WF who presented with a chief complain of Diarrhea. • Also found to have Hypokalemia and Hypomagnesaemia. • HPI: - 7 days hx of diarrhea with decreased oral intake. - No F/C/S Case • PMH - Non-Hodgkin’s lyphoma S/P Autologus BMT - HTN - AKD - CHF Case • Home Medications: - ASA 81 mg daily - Lasix 20 mg daily - Robitussin 20 mEq p.o BID - Tylenol 650 mg PO q4h prn - Folic Acid 1 mg po bid - Loratadine 10 mg po daily Physical Exam • VS: Tmp 99 HR 94 BP 101/51 RR 16 SaO2 92% Gen: A&O x 3, in mild distress HEENT: AT/NC, EOMI, PERRLA Neck: Supple, No JVD, No thyromegaly Chest: CTAB CVS: S1, S2 normal, No M/R/G, NSR ABD: Soft, NT, BS present, No organomegaly EXT: No C/C/E Labs @ presentation • WBC 6.2 Hgb 11.3 Plt 60 • Na 137 K 2.1 Cl 95 CO2 28 AG 16 Glu 101 BUN 18 Cr 1.1 Ca 7.8 Alb 3.2 Mg 1.4 • UA pH 6.5 Trace Protein Positive Nitrite Moderated Leuk. Esterase Spec Gravity 1.009 Cloudy RBC 0-3 WBC 15-2 • C-Diff neg. Urine culture was positive for E.coli Causes of Hypokalemia • Decreased K Intake • Increased entry into cells - Elevation in pH Increased Insulin Elevated B-agonist activity Hypokalemic periodic paralysis Marked increase in blood cell production Hypothermia Chlorquine intoxication Causes of Hypokalemia • Increased GI losses - Vomiting Diarrhea Tube drainage Laxative abuse Causes of Hypokalemia • Increased urinary losses - Diuretics - Primary mineralocorticoid excess - Loss of gastric secretions - Nonreabsorable anions - Metabolic acidosis - Hypomagnesaemia - Amphotericin B - Salt-wasting nephropathies – including Batter’s or Gitelman’s syndrome - Polyuria Diagnosis of Hypokalemia • Can usually be determined from the history • In other case, the diagnosis is not readily apparent • Measurement of BP, urinary K exertion and assessment of AB balance are often helpful Urinary Response Urinary Response Urinary response • The minimum urine K concentration in response to Hypokalemia is 5 to 15 meq/L • A normal subject can lower urinary potassium exertion below 25 to 30 meq per day in the presence of potassium depletion. • < 15 meq per day is likely representative of extrarenal losses Acid Base Assessment • Metabolic Acidosis - with Low urine K exertion in asymptomatic patient is suggestive of Lower GI losses due to Laxative abuse or villous adenoma - with K wasting is most often due to DKA, Type 1 or Type 2 RTA Acid Base Assessment • Metabolic Alkalosis: - With low Urine K exertion is due to surreptitious vomiting or diuretic use - With K wasting and normal BP is most often due to surreptitious vomiting or diuretic use or to Batter’s syndrome. Urine pH and Urine Cl concentration are helpful - With K wasting and HTN is suggestive of surreptitious diuretic Rx in Pts with underlying HTN, renovascular disease or primary mineralocorticoid excess Bartter’s & Gitelman’s Syndrome • • • • • • • Autosomal recessive disorders Hypokalemia Metabolic Alkalosis Hyperreninemia Hyperplasia of juxtaglomular apparatus Hyperaldosteronism Occasionally hypomagnesaemia Bartter’s Syndrome • • • • Named after Dr. Frederic Bartter Prevalence 1 per million Often, but not always associated with MR Pt with a variant of classic Bartter’s syndrome suffer from the same electrolytes disorders, but also has sensorineural deafness and renal failure Gitelman’s Syndrome • After Dr. Hillel Gitelman • Prevalence is 1 per 40000 • More benign than Bartter’s Distinctions between Batter’s & Gitelman’s Syndrome Bartter’s Syndrome Gitelman’s Syndrome Localization of defect Ascending limb of Hanle Distal Tubule Age of Presentation Prenatal, during infancy, early childhood Mostly late childhood or at adult age Biochemical difference Serum Mg may be decreased Serum Mg is decreased Urinary exertion of Ca is increased Urinary exertion of Ca reduced Concentrating capacity severely impaired Concentrating capacity normal or slightly impaired GFR may be normal or declining GFR is normal Functional Studies Back to our Pt • Day 4 of hospitalization Mg 1.6 K in 24 hour urine was 57 and Ca was 32 • Day 9 of hospitalization Mg 1.8 K in 24 hour urine was 81 and Ca was 52 Diagnosis ?