Aneurysms, SAH, Dissections and STUDENT COPY
advertisement
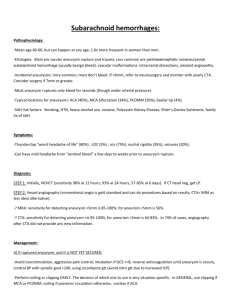
Week 8- Aneurysms, SAH, Dissections and Arteritis Week 8- Aneurysms, SAH, Dissections and Arteritis Week 8 Objectives Define Brain Aneurysm Define Pseudoaneurysms Recognize different types of aneurysm radiographically Be familiar with the angiographic evaluation of patients with cerebral aneurysms Be familiar with the angiographic evaluation of patients with subarachnoid hemorrhage (SAH) Identify methods of surgical treatment of aneurysms Discuss aneurysm coiling Perform basic set-up for Aneurysm coiling Discuss the treatment of wide-necked aneurysm Discuss the balloon remodeling technique What Is An Aneurysm? A cerebral aneurysm is a bubble like outpouching from an artery which predisposes its carrier to cerebral hemorrhage and stroke Images © Frank H. Netter, CIBA Collection of Medical Illustrations History 1927 Moniz - angiography 1937 Dandy describes the clipping of intracranial aneurysm 1949 Robertson described post-mortem lesions after aneurysmal SAH. Brain 72:150, 1949 1951 Ecker & Reimenschneider angiographic spasm Aneurysm Demographics Aneurysms are found in 2-5% of the population More likely to occur in adults age 40-60 There are as many as 27,000 aneurysms that could be diagnosed and treated per year in the U.S. They are more common in women (Sharon Stone had an aneurysm that was treated with coils by an interventional neuroradiologist) The annual rupture rate is approximately 1.5% Rupture of an aneurysm results in approximately 50% mortality and 25% stroke incidence Aneurysm Facts Factors believed to contribute to brain aneurysms: Smoking Hypertension Traumatic head injury Alcohol use Use of oral contraception Post menopausal women > Men Family history of brain aneurysms Other inherited disorders: Ehler’s syndrome, polycystic kidney disease, and Marfan syndrome Aneurysm Facts Symptoms of ruptured aneurysms: The worst headache of your life Localized and intense headache Nausea and vomiting Stiff neck or neck pain Blurred or double vision Pain above and behind eye Dilated pupils Sensitivity to light Loss of sensation The Configuration of Aneurysms Aneurysms can be categorized by their configuration. There are three basic distinctions between aneurysms. They are as follows: Fusiform Aneurysms – Whole vessel circumference involved Saccular Aneurysms – The lesion is eccentric. Pseudoaneurysms - Occur when the layers or wall has been perforated and the rupture is contained by an extraluminal hematoma. Terminology Associated With Cerebral Aneurysms Ectasia is a mild dilatation of a segment of vessel but is not considered to be an aneurysm at this point. Dissection is occurs when a tear in the lining of the artery occurs and blood flows in between layers of the blood vessel. Arteritis is inflammation of the cerebral arteries that obstructs and occludes them. Infundibulum is a funnel-shaped origin of a branch vessel. Classifications of Aneurysms Aneurysms of the Neurovascular system can also be classified into 4 main groupings. The groupings are as follows: Extradural Aneurysms Pseudoaneurysms Intradural Aneurysms Giant Aneurysms Classifications of Aneurysms Extradural Aneurysms Extradural Aneurysms occur outside of the Dura Mater and are less likely to cause subarachnoid hemorrhage. Classifications of Aneurysms True Vs. Pseudoaneurysms Other terms you will also hear are True Aneurysms and False (“pseudo”)Aneurysms True Aneurysms are when the intima, media and advential layers are all intact. False (Pseudoaneurysms) occur when the layers or wall has been perforated and the rupture is contained by an extraluminal hematoma. Causes of Pseudoaneurysm may include: Trauma Dissection Surgical or Endovascular Interventional Injury Biopsy Adjacent Infection Classifications of Aneurysms Intradural Aneurysms There are several categories of Intradural Aneurysms. They are as follows: Fusiform - (Associated with tortuosity, hypertension, atherosclerosis and advancing age) Mycotic and Inflammatory – (Caused by bacteria) Oncotic – (Caused by metastasis) Dissecting – (Caused by a disruption in the vessel walls) Saccular (Berry) – (Develop over time and resemble a “berry”) DeNovo – (Caused by carotid occulsion or ligation) Classifications of Aneurysms Giant Aneurysms Giant aneurysms are defined as aneurysms that are 25 mm or larger in size. Anatomy of an Aneurysm A cerebral aneurysm (also called an intracranial aneurysm or brain aneurysm) is a bulging, weakened area in the wall of an artery in the brain, resulting in an abnormal widening or ballooning. Because there is a weakened spot in the artery wall, there is a risk for rupture (bursting) of the aneurysm. A cerebral aneurysm generally occurs in an artery located in the front part of the brain which supplies oxygen-rich blood to the brain tissue. A normal artery wall is made up of three layers. The aneurysm wall is thin and weak because of an abnormal loss or absence of the muscular layer of the artery wall, leaving only two layers. The base is the “Neck and the top is the “fundus “ or “Dome" Sites of Aneurysm Formation The most common sites of Cerebral aneurysm are: The Circle of Willis Branch Bifurcations Sites of Aneurysm Formation Anatomical distribution and relative incidence of Intracranial Aneurysms. Left: Vessels of the circle of Willis showing multiple aneurysm Right: Inferior view of brain showing subarachnoid hemorrha Hemodynamic Properties of Aneurysms Aneurysms have the capacity to expand over time. The risk of rupture is related to the size of the aneurysm The tensile strength of an aneurysm is assumed to decrease according to Laplace’s formula which is as follows: P = 2 T/r Hunt and Hess Scale (Clinical Grading of SAH) Grade 1 2 3 4 5 Description Hunt and Hess Scale Asymptomatic or minimal headache and slight nuchal rigidity Moderate to severe headache, nuchal rigidity, no neurological deficit other than cranial nerve palsy Drowsiness, confusion, or mild focal deficit Stupor, moderate to severe hemiparesis, possible early decerebrate rigidity and vegetative disturbances Deep coma, decerebrate rigidity, moribund appearance Major Causes of SAH Ruptured arterial aneurysm Ruptured AVM Perimesenchymal vein or capillary bleeding 95% of cases Clinical Manifestations of SAH Ruptured aneurysm headache stiff neck focal deficit Ribeiro JA., et al, Acta Medica Portuguesa. 11(12):1085-90, 1998 Dec. Subarachnoid Hemorrhage: Signs and Symptoms Decreased alertness, Confusion, or Irritability Temporary Persistent Progressively worse to coma and death Syncope Mental Status Exam Abnormal vital signs Respiratory variation Hypertension Irregular heart rate Warning or “Sentinel” Bleeds Up to 50% of patients with SAH report a distinct, severe headache in the days or weeks before the index bleed Milder symptoms History of Headaches J Neurosurgery 1987 Features of Misdiagnosed Patients JAMA. 2004;291:866 -8 Features of Misdiagnosed Patients JAMA. 2004;291:866 -8 Features of Misdiagnosed Patients JAMA. 2004;291:866 -8 Who Needs Imaging? Occipital location Worsens with Valsalva Awakens from sleep Associated with syncope, nausea, or sensory distortion. Patients with a sudden acute-onset headache Prospective studies report that 30% of patients complaining of the “worst headache of their life” had positive findings on CT. Computed Tomography Sensitive for blood day of the bleed 95% within 12 hours of symptom onset as high as 98%. Sensitivity drops when symptoms are days in duration amount of bleeding is small study is difficult to interpret 85% Ruptured Ant CoA aneurysm SAH 20 ruptured right PCA Normal Circle of Willis 3-D CTA Normal Circle of Willis 3-D CTA 3-D CTA SAH 20 ruptured ACA aneurys m 3-D CTA SAH 20 ruptured PCoA aneurysm Lumbar puncture and CSF Exam LP whenever the CT or CTA is negative, equivocal, or technically inadequate Blood or red blood cells in the first 8 hrs. Xanthochromia or an inflammatory reaction when CSF exam delayed Lumbar Puncture (LP) SAH Survival Depends On… Elimination of risk of rebleeding by treating aneurysm (Aneurysm clipping or coiling) Management of Vasospasm Management of Intracranial Pressure (ICP) Management of Hydrocephalus Manangement of Other Complications Management of Cardiac Issues SAH Survival Depends On … Management of Vasospasm Vasospasm Normal Caliber SAH Survival Depends On … Management of Vasospasm Diagnosis Hypervolemic-hypertensive therapy Calcium channel blockers Cerebral angioplasty Intracisternal thrombolytic therapy SAH Survival Depends On … Management of Intracranial Pressure Major Cause of Death ICP monitoring Fluid restriction? Raising head Hypothermia Hypocarbia Barbiturate coma? Ventriculostomy Steroids? Mannitol Increased Intracranial Pressure The pressure exerted in the cranium by its contents:the brain, blood and cerebrospinal fluid. Components of Cranial Vault (ICP can cause herniation!!!) Meninges Brain Brain tissue 80-88% Blood Dura Arachnoid Pia Blood 2-11% CSF CSF 9-10% Elevated ICP = Danger Animated GIF taken from http://www.artie.com Other Problems Elevated ICP can also affect the perfusion of the brain Cerebral Perfusion Pressure (CPP) is measured by taking the Mean Arterial Pressure (MAP) and subtracting Intracranial Pressure (ICP) What does this mean? This shows that if the ICP goes up… and MAP stays constant… then the CPP decreases. This means the patient is not getting as much blood flow to the brain. Poor Outcomes Having an elevated ICP is one of the most damaging aspects of neurological trauma, and is directly related to poor prognosis. Normal Values A normal ICP in an adult ranges from 0-15 mmHG An ICP cannot surpass 40 without causing harm. Even values between 25-30 are considered fatal if they are prolonged. Causes of ICP? An elevated ICP can be caused by many different etiologies. Traumatic Brain Injuries Lyme Disease Hydrocephalus Brain Tumor Severe Hypertension Venous Sinus Thrombosis Restricting Jugular Venous flow (i.e. C-collars) Etc. Monitoring of ICP There are 4 main types of devices for monitoring ICP Intraventricular Catheters Fiber optic Monitors Subarachnoid Bolts Epidural Monitors Stages of ICP Initial compensatory Secondary compensatory Final compensatory ICP: Initial Compensatory Displacement of the cerebral spinal fluid into the spinal canal or into venous blood through the arachnoid mater Intercranial Pressure Regulation When BP increases, cerebral arterioles constrict; when BP falls, cerebral arterioles dilate to increase Cerebral Blood Flow (CBF) Metabolic regulation: Low O2 and high CO2 cause vasodilation; CSF reabsorption and decreased Cerebrospinal Fluid (CSF) production ICP: Secondary Compensatory Reduction of blood volume to the brain. This stage alters cerebral metabolism and produces brain tissue hypoxia and necrosis. ICP: Final Compensatory Displacement of brain tissue which is herniation and often leads to death. Clinical Manifestation of ICP Alteration in LOC – arousal and awareness Restlessness Irritability Confusion Dec.Glasgow coma score – scale for evaluating the best motor, verbal and eye opening response (score 3-15) Changes in speech Pupillary reaction – dilation of pupil ipsilateral to lesion, sluggish to respond to light Clinical Manifestations of ICP Bradycardia HA Vomiting – not preceded by nausea Double vision, ptosis of eyelid, inability to move eye upward Vital Sign changes – Inc.systolic pressurewidened pulse pressure Seizures SAH Survival Depends On … Management of Rebleeding Leading cause of death or morbidity during the first 2 weeks after SAH Incidence: 4-10% in 24 hours 15-25% in 2 weeks 2-3% after 1 month for 10 years Presents with sudden change in neurological status, new headache and coma. SAH Survival Depends On … Management of Rebleeding Aneurysmal Clipping Endovascular Coiling Hematoma Evacuation Procoagulatants Hematoma Evacuation Hematoma Evacuation Teaching Points SAH is often misdiagnosed CT is sensitive but not fool-proof LP for patients with normal or equivocal CT Early angiography and IR/ Neurosurgery eval to facilitate intervention Treat to prevent multisystem and neurological complications of SAH. Attend to the airway and BP Monitor and Control ICP Prevent Re-bleeding and Vasospasm Treatments for Cerebral Aneurysms Endovascular Coiling Surgical Clipping Aneurysm Therapy Surgical clipping (approximately 60-65% in the United States) Endovascular coiling (approximately 30-35% in the United States) In certain countries such as Finland, Great Britain and France, close to 90% of aneurysms are treated with endovascular coiling After the release of the ISAT results, the percentage of aneurysm patients treated with coiling in England went from 40% to 90% International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial The Lancet Vol 360, October 26, 2002 ISAT A recent large prospective study of 2143 patients with ruptured aneurysms who could equally be treated with clipping or coiling had to be prematurely stopped short of planned enrollment of 2500 patients because the coiled patients suffered significantly less death and dependency as compared to clipped patients (6.9% absolute difference, 22.6% relative difference) and it would have been unethical to continue the study ISAT Study Patients with ruptured intracranial aneurysms Dependency or Death at 1 year Neurosurgical Clipping 243/793 (30.6%) Endovascular Coiling 190/801 (23.7%) Lancet. 2002;360(9342):1267-74 Aneurysm Clipping Done under general anesthesia through a craniotomy (hole in the head) The brain is gently retracted in order to gain visual access to the aneurysm A clip is placed at the neck of the aneurysm 1 week in the hospital 1 month recovery Right Cerebellar Aneurysm Surgical Clipping - Step 1: Identify Vessels at Risk ACA Optic nerve Aneurysm exposed ICA & PCA and SCA Oculomotor nerve are identified as Aneurysm vessels at risk. MCA Right Cerebellar Aneurysm Surgical Clipping - Step 2: Measure Baseline Flows Basilar a Flowprobe Baseline SCA & PCA flows are measured SCA SCA = 18 cc/min PCA = 36 cc/min Aneurysm PCA Right Cerebellar Aneurysm Surgical Clipping - Step 3: Clip and Remeasure Positioning of Clip Temporary Clip Flow Integrity Checked SCA = 2-4 cc/min PCA = 55-60 cc/min Right Cerebellar Aneurysm Surgical Clipping - Step 4: Check Flow Integrity Post-Clip Clip Repositioned Flow Integrity Checked SCA = 16 cc/min PCA = 33 cc/min Clip Repositioned Where is the aneurysm? SAH Where is the aneurysm? Surgical clip Before After Clips ANEURYSM COILING A minimally invasive procedure usually performed under general anesthesia by an interventional neuroradiologist A very small plastic tube (microcatheter) is threaded from the groin to the aneurysm in the brain, and fine platinum threads (coils) are inserted into the aneurysm to fill it from the inside, much like filling a pothole The catheter is then removed and the small groin incision covered with a Band-Aid For an unruptured aneurysm, the patient is discharged home within 24 to 48 hours The History of Coiling 1987-1989: Dr. Guido Guglielmi (University of Rome) visits Dr Viñuela (Interventional Neuroradiologist) at UCLA and research work on coiling concept starts 1989: Dr Guglielmi comes permanently to UCLA 1989-1990: Bench and animal research March 6, 1990: First clinical use of Guglielmi Detachable Coil FDA approval in 1995 Imaging of the Aneurysm Non-invasive imaging (CT) has already been done. The Physician probably has a good idea where the aneurysm is located prior to angiography. A diagnostic angiogram is performed and the aneurysm is localized. A 3-D rotational spin can be performed while on the patient is still on the procedure table prior to coiling the aneurysm. Rotational/3D Angiogram Rotational/3D Angiogram The above image can then be transferred to another computer which will take the acquired images and information and transform it into a 3-D image, as pictured below. Rotational/3D Angiogram Measurements of the aneurysms can be obtained from these 3-D images. Procedure Set-Up As you will note, the beginning set-up is the same for all interventional cases. The following slides will review the following: Pressure Bag Set-up Sheath or Guide Catheter positioning Pressure Line Set-Up Don’t Forget To Label Both Ends! Tuohy-Borst Adapter Three-Way Stopcock Before Screwing to Sheath or Guide Catheter… Carefully Flush Check for bubbles Hook to Pressure Bag Line Check and Re-Check for Bubbles The Flow of things…the Pressure Bag Most times the pressure bags are even done ahead of time due to the non-invasive studies already done prior to angiography. The Flow of things…Placement of the Catheter, Shuttle Sheath or Guide Catheter Depending on the Physician and the situation, the Physician may either leave the diagnostic catheter in place or exchange for either the Shuttle Sheath or Guide Cath. If the diagnostic catheter is left in a microcatheter is selected and placed inside the diagnostic catheter. If either a Guiding Catheter or Shuttle Sheath is chosen, they are placed in the Common Carotid and the diagnostic/microcatheter combo is reinserted after being properly flushed with saline. The Flow of Things…The Shuttle Sheath The Shuttle Sheath is a long (usually 90 cm) sheath used to engage the Common Carotid artery. It provides stiffness and stability when coiling. The Pressure Bag line is attached to the sideport of the Shuttle Sheath MicroCatheters This is one of several types of microcatheters (there are also microwires used with the microcatheters). They are ideally positioned directly within the aneurysm sac where the coils will be delivered. Roadmapping and Steering of Coaxial System Use of Bi-plane fluoroscopy Use of Roadmapping feature may be helpful Advance system carefully (Intracranial arteries are thinner than peripheral arteries- less media and adventitia) Hand injections should be done carefully so as not to rupture any perforators. Roadmap During Coiling The Flow of Things…Aneurysm Coiling Once the aneurysm is identified and analyzed,the microcatheter is placed within the aneurysm and the coiling process is started. Follow-up DSA runs are periodically acquired to check the progression of the coiling The Coiling Process The Flow of Things…Aneurysm Coiling The coiling process will probably last for several hours, so one thing to consider, does the patient have or require a Foley catheter? Another note about the drugs. During the coiling process, it’s a good idea to have Protamine Sulfate readily available in case of aneurysm perforation and the need to reverse Heparin. GDC Coil Detachment Device Cable Attachment Black and Red Cables are placed in the corresponding holes of the detachment mechanism Coil Preparation An Aneurysm Coiling Seen Step-ByStep The next several slides will demonstrate an Aneurysm Coiling step-by-step. SAH Rupture of an aneurysm at the tip of the basilar artery Tip of Ventriculostomy before after Pros and Cons of Coiling PROS Minimally invasive Short recovery Safer than surgery Cheaper than surgery CONS Shorter track record Possibly less durable Requirement for followup angiography The Future Increased percentage of patients treated with coiling, in large volume referral centers Use of adjunctive maneuvers increases the percentage of aneurysms treatable with endovascular techniques Increased efficacy of coiling therapy (new, bioactive materials, tissue healing strategies) Development of non-invasive follow-up techniques with CT or MR scanning Better educated population will actually demand availability and discussion of both endovascular coiling and surgical clipping options What about Aneurysms with Wide Necks? Aneurysms with wide necks must be treated in a slightly different manner. The use of a Neuroform stent or some similar stent must first be placed across the base or neck of the aneurysm. This is done so that the coils will remain within the aneurysm sac. Wide neck mid basilar aneurysm Stent + Coil Wide-Neck Aneurysm Coiling with Stent Assistance Stent + coils Balloon Remodeling Balloon remodeling is the use of a balloon while placing coils within the aneurysm. The balloon is inflated while the coil is placed and then deflated once coil is in place. Onyx is another possible choice to treat aneurysms Take Home Points The ISAT study recently demonstrated a substantially better clinical outcome (22.6% less death and dependency relative difference, 6.9% absolute difference) in patients with ruptured aneurysms treated with endovascular coiling compared to patients treated with surgical clipping Take Home Points All patients with aneurysms should be informed of the availability of both endovascular coiling and surgical clipping by a neurosurgeon and an interventional neuroradiologist The death and complication rate for aneurysm therapy is dramatically reduced in high volume centers that offer both surgical clipping and endovascular coiling Information and Links American Society of Interventional and Therapeutic Neuroradiology (ASITN) http://www.asitn.org/ Homework Assignments Read Chapter 16 (pp. 311-347)and Chapter 25 (pp. 467-481) References Morris, P.P. Practical Neuroradiography, 2nd Edition, 2007 Osborn, A.G. Handbook of Neuroradiology, 2nd Edition, 1999 Bontrager, K.L. TEXTBOOK of Radiographic Positioning and Related Anatomy , 5th Edition, 2001 Snopek, A.M Fundamentals of Special Radiographic Procedures, 5th Edition, 2006 Tortorici, M.R. Fundamentals of Angiography, 1982 Various other Internet sources