(NALOXONE) PROGRAMME - Eurasian Harm Reduction Network
advertisement

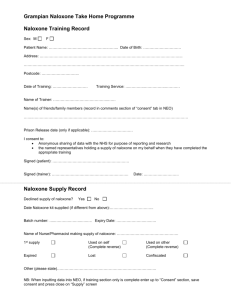
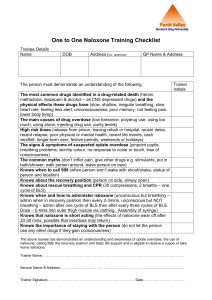
Improving health and protecting human rights for individuals, communities, and society OVERDOSE PREVENTION and MANAGEMENT EURASIAN HARM REDUCTION NETWORK (EHRN) Trainers: Gill Bradbury www.gillbradbury.co.uk Danny Morris www.dannymorris.org 09.00 SESSION ONE WELCOME & INTRODUCTIONS PROGRAMME LEARNING OBJECTIVES DAY ONE Welcome and Introductions • • • Introductory Exercise. House-keeping. Outline of Training & Expectations. An Overview of Basic Overdose Prevention Responses • • Historical Perspective & Background. Overdose Prevention Facts & Practice. Prison Context: Overdose Prevention Evidence & Lessons Learned • • • Prisons – A Public Health Priority - The Needs of Prisoners & Throughcare OD Prevalence Vulnerable Populations - Stigma, Discrimination & Barriers Review of (Focus) Country Responses to Overdose Prevention – • With reference to the EC Reports: Mapping Report - (Estonia, Lithuania, Poland & Romania). Identifying Gaps and Opportunities to Building Capacity • A collective SWOT exercise (Strengths, Weaknesses, Opportunities & Threats) – The chance for an open, honest & facilitated information sharing session to influence policy (and practice) with regard to overdose prevention upon release from prison. LEARNING OBJECTIVES 1 To enable building of capacity: OD prevention programming upon release from prison. 2 To provide a brief historical perspective on OD prevention programmes. 3 To ensure OD prevention & management knowledge. 4 To enable options & an understanding of the different types of OD prevention programmes available. 5 To provide an overview of prevalence, evidence & lessons learned. 6 To provide a review of the situation in each of the focus countries. 7 To enable current gaps and opportunities to be identified. 8 To enable positive advocacy for OD prevention programming. 9 To understand & compare good practice models. 10 To outline effective throughcare interventions which encourage partnership working. 11 To support the potential for in-country planning & action. 12 To ensure an understanding of the next steps for development – Support, supervision & mentoring. ATS Amphetamine-Type Stimulants NSP Needle Syringe Programme DCR Drug Consumption Rooms OD Overdose DRD Drug-Related Deaths OST Oral Substitution Therapy / Treatment EDMC Estonian Drug Monitoring Centre PLHIV People Living With HIV EMCDDA European Monitoring Centre for Drugs & Drug PUD Addiction PWID People who Use Drugs People Who Inject Drugs EC European Commission THN Take Home Naloxone EHRN Eurasian Harm Reduction Network ToR Terms of Reference EU European Union UNODC United Nations Office on Drugs & Crime IEC Information Education & Communication UK United Kingdom LGBT Lesbian, Gay, Bisexual & Transgender US United States (of America) MMT Methadone Maintenance Treatment WHO World Health Organisation NPS New Psychoactive Substances 10.00 SESSION TWO An Overview of Risk and Overdose Prevention Responses OD FACTS & BACKGROUND • • • • • • • • OD is the major cause of death among people who use drugs – mainly opiates / opioids. In the UK, opiate injectors are 14 x more likely to die. Most opiate users experience an OD in their life-time. Increases in OD deaths in recent years. An OD can happen several hours after opiate use. OD occurs more often in risk groups & those who have previously overdosed. Most ODs are witnessed by others. Most fatal overdoses are preventable! HISTORY of OD PROGRAMMES • USA: Originated in harm reduction (HR) services & needle syringe programmes (NSPs) as extension to services for people who inject drugs (PWID). • 1996: Earliest take home naloxone (THN) initiative in via Chicago Recovery Alliance. • 2003: DOPE Project, San Francisco (THN) although they had OD Prevention Programme from 2000. • Good Samaritan Laws: Offer legal protection to people who give reasonable assistance in event of illness or injury – Extended to administration of naloxone in some States. • UK Programmes: Scotland Pilot (2006 - 2007), then 2009 & Wales launched in 2009. No comprehensive English/Irish Programmes yet. 1) EXERCISE – OVERDOSE LITERACY 1. What are the risks related to overdose (OD)? 2. What are the signs of an OD? 3. How does overdose kill? 4. What shouldn’t be done in the event of an OD – (the myths)? 20 minutes – Discuss & identify in 3 small groups 20 minutes – Feedback & Power Point OVERDOSE RISKS • Lowered tolerance due to leaving prison, detox unit or rehabilitation centre & cessation of treatment. • Injecting drugs – (You can still OD if you don’t inject)! • Mixing drugs (poly-drug use) - especially depressants - including alcohol & benzodiazepines. • Using alone. • Homelessness & using in secretive environments. • Compromised health status & metabolism issues, e.g. HIV, HCV & TB (some medications interact increasing risk). • Mental health issues – suicidal ideation or neglectful attitude towards self. SIGNS of an OVERDOSE • Snoring / gurgling noises. • Unable to wake / rouse. • Pallor. • Turning blue (cyanosis) – Lips & extremities. • No pulse. • Pin point pupils. • Shallow breathing. • Difficulty breathing. HOW DOES OVERDOSE KILL? First breathing is very slow Then… breathing stops Then… the heart stops Lack of circulation of blood & reduction of oxygen to the brain… Death occurs… OD MYTHS & WHAT NOT TO DO • Cold bath / shower. • Walk person around. • Get them outside for fresh air. • Hit them. • Inject salt water or milk. • Inject stimulants. None of the above will ever reverse an OD & if it seems to – it is pure coincidence – PLEASE DISPEL THE MYTHS! Never leave the person alone & do call emergency services! 10.45 SESSION THREE Prison Context: Overdose Prevention Evidence and Lessons Learned OVERDOSE on RELEASE from PRISON (1) • Release from prison is associated with significantly increased mortality from drug OD. • Risk does not appear to have decreased in last 20 years – (WHO, 2010). • For prisoners with history of opiate use, risk of dying from OD greatly increases in period following release - due to high rates of relapse & lower tolerance. • Critical time for action - ensuring continuity of care & targeted interventions to support treatment engagement & save lives. OVERDOSE on RELEASE from PRISON (2) • Review of prisoner deaths, occurring within 12 weeks, postrelease indicated 6 in 10 deaths were drug-related. • Increased risk of OD during first 2 weeks post-release - risk remains elevated until (at least) the fourth week. • During first week post-release, female prisoners 69 x more likely to die of drug-related causes. • During first week post-release, male prisoners 28 x more likely compared with general population. EU & MEMBER STATES – CONTEXT – (1) • Responding to drug-related healthcare needs of prisoners identified as public health priority by EU & Member States. • In response to concerns re: increasing prison populations, European Parliament (in 2004) adopted recommendation on rights of prisoners in EU - includes treatment of PUD in prison & reduction of health-related harm. • Prisoners recognised as a vulnerable population. • “EU Drugs Action Plan 2009 – 2012” - Objective of providing drug users in prison with improved access to healthcare to prevent & reduce health-related harms associated with drug dependence. EU & MEMBER STATES – CONTEXT – (2) • Drug offence conviction is important indicator of potential OD risk targeted interventions to high risk prisoners. • Growing importance now attached to ensuring common minimum prison standards across EU Member States & exchange of best practices. • Other Policy Guidelines: WHO Health in Prisons Guide (2007) & the UNODC Briefing on HIV Prevention, Treatment & Care in Prisons (2012). NEEDS of PRISONERS & SERVICES • Prisoners entitled to same level of medical care as people living in the community. • Prisons should provide drug-related treatment & care in conditions comparable to those outside. • Pre-release measures also essential for PUD. • Upon release, prisoners face a range of physical, practical & psychosocial challenges. • In that, they require comprehensive & specialised services to treat both, drug use & health problems. • Liaison with external services is therefore fundamental. THROUGHCARE • Vital for cooperation between services inside prison & health / social care services outside. • Important to enable continued support & seamless transition into community treatment. • Throughcare refers to arrangements for managing continuity of care before, during & immediately after custody. • In countries where prison & community services operate under the same roof, throughcare between the two settings is easier to achieve. • Within some prisons, pre-release units have been established to facilitate such referrals & to allow a smoother transition. PRISON RECOMMENDATIONS A number of interventions targeting opioid users have been recommended to reduce risk of fatal OD in period shortly following prison release: • Pre-release counselling on OD risks & training in first aid & OD management. • Optimising referral to achieve continuity of drug treatment between prison & community – (throughcare). • Distribution of naloxone among opioid users leaving prison. PRISONER VULNERABILITY • Prison populations vulnerable in other ways - complex (often unmet) needs. • Compared with general population, prisoners (particularly PUD) are extremely disadvantaged & marginalised. • Many prisoners have limited education & low socio-economic status. • Poverty, violence & crime also common features in their lives. • Women have multifaceted health & social needs. • High levels of co-morbidities – (i.e. physical & mental health problems) among prisoners & chronic, drug-related problems. BRAINSTORM People who use drugs & prisoners are vulnerable. However, there are other (PUD) populations who face secondary stigma & discrimination – • Identify these further marginalised groups of people. • Why might they be even more vulnerable? • Are there any special measures you could take to engage them? OTHER VULNERABLE POPULATIONS WOMEN - Prisoners more likely than men HOMELESS PEOPLE - At particular risk to have been incarcerated for drug offences. of OD & drug-related death. Less likely to Also, likely to have serious drug-related health engage with services & may come into more (& other) problems + specific needs. contact with law enforcement agencies. YOUNG PEOPLE - 11 % of OD deaths PLHIV / PLHCV and / or TB - High reported in Europe occurred in those under rates of HIV, HCV & TB amongst PUD. Poorer 25 years. Young people at risk of OD due to general health. Some illicit drugs can interact lack of experience & lack of specialist services. with ARVs / TB medications. More susceptible to OD - metabolism issues & health status. MIGRANTS / FOREIGNERS - On average, 21 % of prisoners were foreigners. Migrants often unaware of services available within the community & may have difficulties accessing them. ROMA PEOPLE - LGBT / MSM - Drug use widespread. Additional issues re: stigma & discrimination, LGBT people may not access services unless specifically targeted. Numbers of LGBT people held in prison system is unknown. Widely discriminated DUAL DIAGNOSIS - Studies show that against. Such marginalisation makes them less several types of mental health disorders, likely to access services & receive treatment, occur at higher prevalence rates among which is a protective factor. Also more likely to prisoners than in the general population be imprisoned. STIGMA & DISCRIMINATION • A social process which can reinforce relations of power & control. • Leads to loss of status & discrimination for those who are stigmatised. Ref: Link & Phelan • Drug use often inter-related with discrimination, lack of economic & social empowerment & minority status. • Stigma attached to injecting drug use & HIV is further amplified by the social stigma of HCV which significantly affects PWID. BARRIERS to ACCESS Notley et al. (2012) identify several barriers (to treatment generally) Grouped under 3 main headings: system barriers; social barriers; & personal & interpersonal barriers. • System barriers include poor communication between services. • Main social barrier was stigma, particularly amongst certain (marginalised) communities. • Personal & interpersonal barriers - include perceived lack of choice & personal control… BREAK 11.30 am 11.45 SESSION FOUR Optimum OD Prevention and Management: Naloxone Programming FILM “Naloxone - I am the evidence” Service users & staff of Swansea Drug Project (Wales) describe the powerful impact of naloxone distribution there. • http://www.youtube.com/watch?v=jVdp5oDp_5g 10 minutes OD PROGRAMMING • IEC – Information, Education & Communication Materials. • Brief Interventions – Overdose Training & First Aid. • Peer-Led Education & Training. • Pre-Release Education & Training. • THN – Take Home Naloxone. • Sign-posting to Community Harm Reduction Services. • Meet & Greet at Prison Gate – Naloxone Supply. WHAT TO DO? Remember the word C.A.R.A. • • • • C – Call an ambulance A – Airway (check it’s clear) R – Recovery position A – Administer Naloxone DO NOT PANIC! Or/ DR’s ABC • D - Danger • R – Response • S – SHOUT • A - Airway • B - Breathing • C - Cardiopulmonary SCARE ME • Stimulation: Does the person respond to stimulation – shake & speak to rouse If not, this is an overdose needing attention. • Call Emergency Services. • Airway: Is person’s airway unobstructed? - Are you able to breath for them? Surviving an opiate OD is all about having a clear airway and breath! • Rescue Breathing: Provide rescue breathing for the person as this can save a life if all else fails! • Evaluate the Situation: How is the breathing coming along? - Do you have naloxone nearby? - Is it worth stopping the breathing to get it? • Muscular Injection: Administer naloxone dose into shoulder or thigh muscle. Resume rescue breaths. • Evaluate again: Naloxone takes 3 - 5 minutes to work. Keep up rescue breathing. Give another dose of naloxone if no response in five minutes. DIFFERENT TYPES of NALOXONE PREPARATIONS WHAT is NALOXONE? • Used in clinical settings as emergency treatment for opiate OD since the 60’s. • Naloxone is an opiate / opioid antagonist. • Temporarily reverses effects of an overdose - (only opiates). • Naloxone lasts between 20 minutes to 1 hour. • Overdose can last up to 8 hours - Naloxone buys time to call emergency services. • People can return to an OD state once naloxone wears off – Therefore, it is important that emergency services are called! • Different preparations: Most commonly separate ampoule & injecting equipment in a kit - but pre-filled syringes & intra-nasal sprays are also available (more expensive). NALOXONE STORAGE • Naloxone should be carried with the person at all times – OR/ • Held in specific place at home / where person uses drugs. • PUD should make others aware that they have naloxone, how to use it & where it is kept! • Do not refrigerate & must be protected from light. • Expiry date 18 months – 3 years after manufacture (shelf life) – Anecdotal evidence will work after expiry. • However, commitment to prescribing should include & ensure resupply when expiry date reached. HOW TO USE NALOXONE • • • • • • Remove needle & syringe from package. Attach needle to syringe. Tap ampoule to remove Naloxone from ampoule neck. Carefully ‘snap’ ampoule. Insert needle & draw up Naloxone - Aspirate syringe. Identify injecting site - Inject outer thigh, upper arm or outer part of buttock - Spread skin, insert needle in muscle - (needs pressure). • Hold like a dart & inject at 90 degrees – through clothes! • Slowly & steadily push plunger all the way down. • Remove needle & syringe - Dispose of all equipment safely. UPPER THIGH UPPER ARM RECOVERY POSITION DON’T PANIC ACT FAST ADMINISTER NALOXONE RECOVERY POSITION SAVE A LIFE! AFTER USING NALOXONE • • • • • • • • Naloxone can take several minutes (2 - 5) to start working. If responsive & breathing place in recovery position. Person may be confused - Explain to them what happened. Advise person not to walk away until they have been seen by Emergency Services. Advise them to not use any further drugs!!! Remind person that naloxone will wear off in a little while & the opiate effect will gradually return. If they refuse to go to hospital, explain to them that they might slip back into overdose over the next 2 - 3 hours. If NOT breathing start Rescue Breathing / CPR. FILM “NARCAN” Chicago Recovery Alliance SUMMARY – Things to Remember (1) Naloxone is treatment specific – It can only reverse effects of opiate/opioid OD - e.g. Heroin, Methadone, Morphine, Fentanyl, etc. Risks of Overdose • Low tolerance, injecting, mixing drugs, using alone, etc. Signs of Overdose • Snoring / gurgling sound, unable to wake, no pulse, not breathing, pallor / turning blue, pin point pupils. Response • C.A.R.A – Call Ambulance, Airways, Recovery Position, Administer Naloxone. SUMMARY – Things to Remember (2) Naloxone • Lasts between 20 minutes – 1 hour. • Overdose can last 8 hours & can return. • Call Emergency Services. • Inject into the muscle (through clothes). • Dispose of injecting equipment safely. • Stay until the ambulance arrives & reassure the person. • Tell your friends & family about it – 85% of people are not alone when they OD! EUROPEAN PRISON SYSTEMS Treatment for drug dependence aimed at both improving health of prisoners & reducing illicit drug use in prisons. Treatment options for PUD in EU prisons cover a range of modalities - Broadly categorised into 3 types: • Low-intensity drug treatment: Counselling interventions & short-term treatment - outpatient regime in prison setting. • Medium / High-intensity drug-free treatment: Inpatient wards & delivery of treatment in therapeutic communities. • Medium / Longer-term OST programmes – i.e. methadone or buprenorphine. ESTONIA and OVERDOSE • Estonia has one of highest rates of death by OD in Europe. • Opioids, 3-methylfentanyl in particular, present in 95.9 % of deaths where toxicological results known. • In many cases other substances also present. • Prior to recent roll out of community THN programme, specific responses to preventing DRDs uncommon. • Info on OD risk reduction available through low-threshold centres & outreach work to limited extent. • IEC materials available on prevention of acute DRDs & drugrelated emergencies for family & friends. “Even experienced users report difficulties in managing dosing of Fentanyl and the strength varies. Fentanyl is imported but it is not a pharmaceutical product.” Aljona Kurbatova Head of Infectious Diseases & Drug Abuse Department - National Institute for Health Development, Hiiu 42, Tallinn 11619, Estonia. DRUG-RELATED DEATHS CASES 2011 2010 2009 2008 2006 2005 2004 123 101 133 67 68 57 98 Gender: Majority Male = 87.8 % Drug Related Deaths / Million = 135.7 Mean Age 30.1 years Number of Deaths by Drug/Alcohol Intoxication in Prison 2010: There were 8 deaths within penal institutions in Estonia during 2010 - None of these were reported to be as a result of drug overdose. There was 1 suicide recorded (which was a woman). Mortality rate per 10,000 prisoners is 23.1 ESTONIA – PRISON TREATMENT • Lack of capacity for low intensity-treatment – (defined as fully matching prisoners’ demand) - identified in 5 EU countries - one of which was Estonia. • Drug-free inpatient treatment / Therapeutic Communities available - but not to majority of prisoners in need. • Methadone detox & maintenance available since 2008 Significantly increased during 2010. • 2011: Handbook produced for prison staff - How to work with PUD - (does not include info on OD emergencies & DRDs). • Pre-release OD counselling provided to limited extent. ESTONIA – COMMUNITY THN • Estonia currently establishing a community take home naloxone (THN) distribution programme. • Centrally funded - Very new scheme, it required several years of planning & negotiation. • September 2013: Programme made available in Tallinn. • Since January 2014: Available in 2 locations in Tallinn, also in Jõhvi - (in 1 location), Kohtla-Järve - (in 2 locations) & Narva - (in 1 location). • These areas most affected by injecting drug use & HIV. ESTONIA & THE SCOTTISH MODEL • Community OD Prevention & Management Programme based on Scottish model - Should be commended for this! • Estonia should continue to observe development of Scottish National Programme - in particular THN within prison setting – Also important to heed any lessons learnt. • Scotland has independent process evaluation of National Programme (SNP) underway - results of which may be invaluable. • Estonia will embark upon a pilot prison naloxone programme (end of the year) – Opportunity to demonstrate best practice by learning from both types of SNP prison delivery models. • Challenges for Estonia : A much more resource limited setting! OPPORTUNITIES for DEVELOPMENT • OST & IEC in prisons requires significant scaling-up. • Opportunities to introduce & develop prison OD programmes as per the Scottish model. • Pilot pre-release training & distribution programme planned End of 2014. • Robust monitoring & evaluation necessary. • Treatment providers in prime position to liaise with prison authorities to establish comprehensive throughcare systems & sign-posting to service providers able to supply naloxone. • Other innovative approaches & use of peers. LITHUANIA, OST and OD RATES • In 2011, 45 direct DRDs recorded - indicates a decreasing trend since 2007, when 72 drug-related death cases were registered. • OD deaths considered to be very low. • Comprehensive OST programmes exist. • Suggested low OD rate due to supervised consumption of OST. • Likely to reflect under-reporting &/or misreporting as well. • 3 mobile outreach & NSPs in Lithuania distributing IEC materials. • No NSP in prisons – (disinfectants provided). • Lithuania - one of only 4 EU countries that don’t allow prison doctors to prescribe long-term OST. AGE 2007 GROUP Under 15 0 15 – 19 3 20 – 24 12 25 – 29 25 30 – 34 20 35 – 39 4 39 and 8 over TOTAL 72 2008 2009 2010 2011 0 1 10 22 6 11 10 0 0 6 24 16 10 12 1 0 12 9 10 11 8 0 1 6 14 10 6 8 60 68 51 45 DRUG-RELATED DEATHS CASES Source: General Mortality Register of the Institute of Hygiene from 2010. Source: Until 2010 - Department of Statistics under Government of the Republic of Lithuania. Toxicological analyses reported for 97.8 % of DRDs in 2011. Opioids = primary substances involved in 54.5 % of DRDs with known toxicology results. 40.9 % of deaths due to mixed or unknown substances. Gender: Majority Male = 82.2 % Mean Age at Death = 33.4 years DRDs / Million = 20.9 Number of Deaths by Drug / Alcohol Intoxication in Prison 2010: 25 deaths in penal institutions in Lithuania during 2010 - None of these reported to be a result of drug overdose. 8 deaths recorded as suicide (none were women) & mortality rate per 10,000 prisoners = 28.1 LITHUANIA and OD PREVENTION • Re: Reduction of DRDs, predominant response strategy is dissemination of IEC materials. • IEC materials distributed in low threshold agencies & NSPs, specialised drug treatment centres & detox services. • Report: “Current State of Play of 2003 Council Recommendation on Prevention & Reduction of Health-Related Harm, associated with Drug Dependence in EU & Candidate Countries” affirms that risk education & OD response training is available in nearly all cities or towns with OD IEC materials available for police, prison staff, family/ friends & night club staff. • No other formal OD prevention programmes & interventions. LITHUANIA & NALOXONE “There are no plans for naloxone distribution & OD education is not routine within services. We don't see a lot of OD's - maybe there are more overdoses but perhaps they are not registered as such. Methadone access is good & it is well supervised.” Dr. Emilis Subata - Associate Professor of Vilnius University Psychiatry Clinic and Director - Vilnius Centre for Addictive Disorders - WHO Collaborative Centre for Harm Reduction Gerosios Vilties 3, Vilnius, Lithuania, LT- 03147. PROACTIVE PRISON WORK • No plans for community-based THN – Therefore, prison OD programmes unlikely at the moment. • Important (for services) to establish proactive links with prisons. • Necessary to enable effective through-care arrangements so as community services can swiftly initiate `re-tox’ as appropriate. • Community services could consider `in-reach’ work in prison setting (if permitted) - Education re: risks of OD; signs & symptoms; myths & correct actions to take. • Circulating IEC materials in prison (& community-based services) offers further opportunities for OD prevention interventions. • Involve peers in production of IEC materials. POLAND and DRUG TREATMENT • OST available in Poland - first methadone maintenance programme introduced in 1993. • 2011: 32 OST programmes (including 7 prison OST programmes) Provided services to about 2,200 clients. • Methadone mostly, although buprenorphine-based medications also available. • Some harm reduction projects exist in prisons - Primarily offer info on safer drug use etc. but no NSPs. • 64% of PUD accessing harm reduction projects are opiate users. • Programmes unable to engage with all PUD - many of whom are hard to reach & remain marginalised. POLAND and OVERDOSE • Data from general mortality registers indicate that DRDs seem to be relatively stable. • Overall trend downward since 2002, when 324 DRDs were registered. • In recent years, number of reported cases has fluctuated between 214 cases in 2007 & 261 in 2010. DRUG-RELATED DEATHS CASES Source: Central Statistical Office 2010 2007 2002 261 214 324 Drug Related Deaths / Million = 8.4 Historical data regarding people who inject drugs (PWID) is very unreliable. Recent changes in methodology - attempting to rectify this issue to reflect more accurate picture. No data available for 2011. Gender: Not Available Mean Age: Not Available Number of Deaths by Drug / Alcohol Intoxication in Prison in 2010: 135 deaths in penal institutions in Poland during 2010 - Data not available re: number of drugrelated deaths in prison. 34 deaths registered as being as a result of suicide – (no data about the numbers of POLAND and OD PREVENTION • Some form of OD prevention offered via harm reduction projects & specialised drug treatment / detox services, etc. • Common response strategy is risk education / response training delivered in some cities. • Provision of OD IEC materials reported to be extensive & peerinvolvement approach common. • Telephone help lines, websites & broad range of leaflets available nationwide, as well as quarterly magazine for PUD. • IEC materials on prevention of acute DRDs & drug-related emergencies available for prison staff, night club staff & sex workers who use drugs. Nothing available for family & friends. • At least 3 projects have targeted PUD, LGBT & SW populations. POLAND and NALOXONE • General aim of Polish National Programme: To reduce drug use & drug-related social & health problems. • A more comprehensive approach to OD prevention & management has the opportunity to fit well within this objective. • Consideration being given to pilot programme within community (not prison) harm reduction services for THN to PWID. • If successful, not unreasonable to lobby for wider programme roll out - including within prisons to prisoners pre-release. • Law currently forbids THN – Legislative barriers need to be overcome. • Emergency services use naloxone as antidote to OD situations. POLAND and PRISONS • 7 OST programmes in prisons. • These offer prospects for provision of education & other OD prevention interventions – subject to capacity of staff involved. • Training needs analysis (TNA) could be conducted amongst prison employees involved with PUD. • Any necessary training implemented, preferably using peers as well. ROMANIA and OVERDOSE • Sharp decline in DRDs in 2011 - partly explained by increase in novel psychoactive substances (NPS). • Use of heroin replaced by use of these substances. • NGOs dispute this data & low figures - believing that OD & DRDs are under-reported due to bureaucracy in medical settings. • Deaths often attributed to respiratory failure / another cause - with no further investigation. • 2011: Around 73.3 % of DRDs caused by opiates. • In 9 cases, presence of methadone detected. • Naloxone is available to medical / ambulance personnel & is used accordingly. DRUG-RELATED DEATHS CASES – Source: Forensic Medicine Network & National Legal Medicine Institute 2011 2010 2009 2008 2007 2006 15 34 32 33 32 21 Drug Related Deaths / Million = 1.0 Gender: Majority Male = 80 % NB: Under-reporting suspected! 30.4 Years Mean Age at Death = Number of Deaths by Drug / Alcohol Intoxication in Prison 2010: 77 deaths in penal institutions in Romania during 2010 - None of these attributed to drug overdose. 7 deaths registered as suicides - (none were women). Mortality rate per 10,000 prisoners = 27.3 ROMANIA and DRUG TREATMENT • Some OST provision in Romania - Capacity to treat 1,000 PUD. • Estimated 19,000 to 20,000 PWID in Romania - This includes people who inject NPS. • 2012 data indicates 50 % decrease in PWID population. • Coverage rate for OST is low - 742 clients reported in treatment in 2011. ROMANIA - STIGMA & DISCRIMINATION • PUD are poorly represented nationally. • Limited peer involvement activities. • Financial pressures reinforce stigma & acceptability of rationing services. • PUD considered to be ‘undeserving’ & `undesirable’ communities. • Discrimination prevails in services, between peers, as PLHIV have requested separate (segregated) services for PLHIV who also use drugs. ROMANIA and OD PREVENTION • Appears to be no formal / strategic responses to OD prevention & management. • Unaware of any OD educational programmes or specific policies re: OD prevention & it is unclear as to what’s occurring. • This conflicts with info from the `Current State of Play of the 2003 Council Recommendation on the Prevention and Reduction of Health-Related Harm, associated with Drug Dependence in the EU and Candidate Countries’ - States THN is available with doses being distributed to PUD, peers & relatives who have completed first aid training & training on OD management. PRISON RECOMMENDATIONS • Prison in-reach & training of prison staff: pre-release counselling on OD risks & prevention + training in first aid & OD management. • More effective systems for throughcare to increase opportunities for treatment & developing interventions re: OD prevention. • EU Prison Rules specify prisoners be offered medical examination close to time of release - Routine ‘exit’ health examination not common in Europe - Should be enforced as a requirement. • Distribution of naloxone among opioid users leaving prison unlikely at the moment… Should continue to be promoted & lobbied for as a fundamental measure to reducing DRDs. BREAK – 15.15 SESSION SIX Identifying Gaps and Opportunities to Building Capacity A SWOT Exercise Strengths Weaknesses Opportunities Threats 5 FUNDAMENTAL QUESTIONS :1. The key qualities of your organisation which makes an OD Prevention & Management Programme possible? 2. What are the weaknesses of the organisation & system you represent? – 3. How & where could you gain support? – What is a feasible (draft) plan for the future? 4. What are the barriers? – What prevents development of a comprehensive OD & THN Programme? 5. Identify the opportunities & solutions. BARRIERS to ACTION • • • • Firstly, barriers exist for PUD Secondly for witnesses (to an OD) Thirdly for service providers & Fourthly for policy makers & national stakeholders. These dynamics & barriers (systems, social, personal & interpersonal) can be applied to action planning areas for: • • • • Assessing need Planning Implementation Evaluation & continued development of OD programming. Reference: IDPC http://dl.dropboxusercontent.com/u/64663568/library/IDPC-training-toolkit/Module-2.pdf CLOSING EXERCISE Brief group exercise to summarise & close the day - Prior to the EHRN Evaluation Form being completed. • Please state two things that you have gained / learned from today, or which has made an impression – • And, how you will / might be able to take this forward? Consider your `mission statement’ this morning too! THANKYOU – HAVE A GOOD EVENING SAVE A LIFE - THN TAKE HOME NALOXONE SESSION SEVEN Summary of Day One Introduction to Day Two Solution-Focused (Opening) Exercise DAY TWO Introduction and Summary of Day One • Any Questions & Expectations? • Outline of Day Two Good Practice Models • Review of models available in Scotland, Denmark, Italy & Spain. • Challenges • The application of good practice models to each of the focus countries. Establishing a Programme - Country Action Planning • Formulation of individual (country) Plans of Action. Next Steps – Mentoring and Supervision • Details of further support, supervision & mentoring which will be available following this course. Constructionist Evaluation Exercise Feedback & EHRN Evaluation SESSION EIGHT Good Practice Models – Scotland, Denmark, Italy & Catalonia UK OVERDOSE DATA / FACTORS • Last 10 years, most UK deaths linked with opiates, primarily heroin/morphine (n = 820) & methadone (n = 765). • 2010 – 2011: 23 % decrease in heroin/morphine deaths. • 2010 – 2011: 52 % increase in methadone deaths. • Scotland: More methadone deaths recorded than heroin deaths – First time since 1997. • Due to reduced heroin supply reported in late 2010 & early 2011? • Scottish DRD Database (2010): 162 methadone deaths - 53 % (86) NOT on OST at time of death. • 11 % increase in Tramadol deaths between 2010 & 2011 – (4x more than in 2003). • Alcohol implicated with one or more drugs in 29 % of deaths. DRUG RELATED DEATHS in the UK 2011 2010 2009 2008 2,250 1,930 2,481 2,569 UK Gender: 73.9 % male Mean Age: 40.8 584 485 545 574 SCOTLAND National Records of Scotland Figures UK DRUGS STRATEGY • Access to effective treatment is a priority of UK drug strategies. • Treatment capacity increased substantially but can still be improved. • Treatment Demand Indicator (TDI) data = People presenting to treatment - From 4 separate country systems in UK. • Scotland: Data monitored via Scottish Drug Misuse Database (SDMD). • In accordance with Scottish Drugs Strategy, PUD offered range of treatment: OST; residential & community rehabilitation; community detox & psychosocial / motivational interventions. • Between April & June 2012, 90 % people gained access to specialist treatment within 3 weeks. SCOTLAND STRATEGY • National Drug Strategy - ‘The Road to Recovery’ - since 2008. • Recommended range of services - including alerting PUD to dangers of lower tolerance as way to help prevent DRDs. • Strategy highlights role Primary Care / Medical Practitioners could play in recognising risk & potential fatalities. • Crucially, strategy identifies need to give people confidence to know when to intervene, what to look for & what to do - as key to helping reverse the OD trend. • Recommends adequate training & relevant IEC materials for staff, service users, family & friends. • Increasing awareness brings improvements over time. SCOTLAND – (SNP) NATIONAL (NALOXONE) PROGRAMME • Fundamentally, vision of strategy was implemented through a National Naloxone Programme ~ (henceforth ‘the National Programme’ or/ SNP). • Pilots: 2006 - 2007 & 2009. • First programme being centrally coordinated & funded by Scottish Government. • Aiming to reach all those at risk of opioid OD, including people in prison. • Aim: To contribute to reduction in fatal opiate/opioid ODs in Scotland = Higher than UK average. LEGISLATION & POM • Medicines normally supplied on named patient basis. • Naloxone is a parenteral (i.e. injectable) - Prescription Only Medicine (POM) - Under UK Medicines Act (1968). • Supply of naloxone, as a POM, can only be made on a named patient basis using either a prescription or a Patient Group Direction (PGD). • PGD is a legal device that allows appropriately qualified nurses / pharmacists to supply POMs in specific defined circumstances. POM EXCEPTIONS • Limited list of exceptions - In 2005 naloxone added to list. • 2005 amendment allowed development of THN schemes. • Whilst supply of naloxone must be to named person - can legally be administered by anyone present at scene - (who is in position to intervene before ambulance arrives) - to anyone suspected to have overdosed - in order to save a life. • Supplies not restricted to PUD receiving treatment - Available to anyone identified to be at risk of OD irrespective of current or previous contact with treatment services. DEVELOPMENT • National Programme launched late 2010 & commenced in 2011. • To date, 13 (of 14) Local Health Boards (LHBs) opted in. • Regional variations with regard to delivery models. • Community Peer Education approach – Extended to prison programme. • Developing last 3 ½ years. • Successful delivery depends upon multi-disciplinary professionals & trained peers from communities of PUD. PRISON IMPLEMENTATION • Main prison model (at the moment) identifies prisoners at risk (i.e. opiate users) on admission / during sentence & naloxone supplied on release. • Nurse ensures naloxone placed with prisoners’ belongings - stored at reception & returned on release from custody. • February 2011: Prison supply of THN kits introduced incrementally. • June 2011: All Scottish prisons taking part in programme & approx. 100 prison staff trained - introduction & implementation phase. • Significant success so long as national commitment + consistency of distribution can be maintained. SCOTLAND – A PEER-LED APPROACH • Peer-led OD prevention & management training to other prisoners with history of opioid use. • `Brief Interventions’ training as per community model. • Improves credibility & uptake. • Support from Prison Services & National Coordinator. • National Programme demonstrates good governance. • Now developing model & THN within Female Prison Estate. SELECTION CRITERIA & TRAINING • Peers selected after skills-based assessment. • Peer-led training is facilitated. • Ability to engage with training programme is main factor. • Training of peer trainers = half-day drugs awareness - (including stigma & discrimination). • Followed by 2 days OD prevention & management `training for trainers’. • Same content also delivered for (prison) staff training. BRIEF INTERVENTIONS TRAINING Most effective, peer-led approach • Peer trains peers - 1:1 brief intervention model – this encourages more people to engage. • Can take as little as 15 minutes depending on individual knowledge & capabilities. • Exceptions when peers need more time - interventions tailored to meet specific needs. • More thorough `Basic Life Support’ training if requested - this component generally delivered via IEC materials. • Peer trainers skilled enough to adapt (to person in front of them) & determine level of training required. TRAINING OUTLINE – (1) Brief Interventions (BI) Training for delivery of a naloxone distribution programme covers: • Why there is a need for naloxone? • The drugs involved in opioid OD • Risk factors for opioid OD • How to recognise an OD • What to do and what not to do Then… TRAINING OUTLINE – (2) - It is followed by a practical skills session: • Teaches people how to inject naloxone. • How to administer basic life support. • How to place someone in the recovery position. • Naloxone administered by IM (intramuscular) injection into outside of thigh through clothing. Usually via IEC materials - pictures + written information & verbal explanation. OTHER BENEFITS • This kind of peer engagement has benefit of reducing stigma & discrimination. • Allows staff to appreciate knowledge & skills of peer trainers. • Contributes to general awareness-raising - prison employees & healthcare professionals • Promotes need for widespread THN for those at risk in prison. • Positive links with nurses can improve uptake of naloxone - if responsible for supplying naloxone to prisoners upon release. • Scottish Programme committed to & is increasingly demonstrating good levels of peer involvement in the implementation of OD programmes - including those in prisons. BENEFITS and EFFECTIVENESS Number of Prison OD Programmes 16 All prisons providing programme slightly differently. Number of Prison Take Home Naloxone (THN) Kits Issued – 746 715 (2012/13) (2011/12) Prison Gender Distribution for 2012/13 76.6 % 23.1 % 0.3 % Male Female Unknown 23.1% of kits supplied to women in prison - higher uptake, compared with male prisoners. Women represent less than 6 % of total prison population. Age Distribution for 2012/13 Prisoner age profile younger than community recipients. Prison data shows age profile also relatively younger. Number of Prison Peer Trainers Consent to Recording of Personal Data Comparative Uptake of THN 20.1 % 44.5 % 34.5 % Under 25 Aged 25 – 34 years Aged 35 and over 11 5 First groups of peers trained – Edinburgh Prison. 98.7% Most people do not object to such data being collected! 375 More 2012/13 - Prisons & community. SCOTLAND – NATIONAL PROGRAMME SUMMARY • Considered model of good practice (Wales has similar services, along with other countries) - But in Europe, Scotland more so at the moment. • Higher profile due to increased coverage at national level – Both in prisons (& comprehensively within community). • Political Will & Commitment: The National Programme has Governmental (Public Health) Investment. • Having national infrastructure, collaborative approach & integration is critical to evolving success. • Other advances & innovative THN – (e.g. INS – Highlands, independent of the National Programme). OTHER INNOVATIONS • Lord Advocates Guidelines relaxed regulations governing naloxone to permit non-health professionals to hold it in settings where people may be at risk – (e.g. homeless hostels, shelters, etc.). • This guidance on naloxone totally unique - allows POM to be supplied to a service, which wouldn’t normally store “stock” medication. • Prisoners & homeless people are vulnerable populations, more likely to OD & access hostels, etc. MONITORING & EVALUATION • Independent Process Evaluation – Any lessons to be learned (?) • Evaluation to identify best practice, barriers & enablers to further roll-out &, if possible: • Any other behaviours that have been influenced as a result of training & the use or impact of naloxone. • Monitoring & evaluation important to evidence progress & interventions – To ensure future funding. CHALLENGES – (BARRIERS) Notley et al. (2012) - Several barriers (to treatment): • SYSTEMS: Poor communication between services, etc. • SOCIAL: Mainly, stigma – especially amongst PUD / PLHIV / HCV. • PERSONAL & INTERPERSONAL: Perceived lack of choice & personal control… SYSTEMS – (1) • Many challenges training this population – Both, staff & prisoners. • Prison regime can cause problems given length of time available to deliver `Training for Trainers’ Peer Programme + • Other operational / security issues often arise in prison setting. • Prison distribution varies in establishments – Prison programmes may all be slightly different in their delivery models. • Sustainability issues: Important to develop effective throughcare systems - (whereby newly released prisoners are linked with community programmes, particularly in the absence of THN). SYSTEMS – (2) • Prisons (part of National Programme) – BUT supply not as high as expected - Particularly given awareness of prisoners as high risk population & evidence to support this. • Important to note: women 69 x more likely to die of drug-related causes during first week post-release (compared with men who are 28 times more likely to die during that period). • Ongoing liaison, strategic work & commitment required re: uptake & development. • Sustainability: New prisoners will have to be trained to replace peer trainers who are released from / transferred to another prison. SOCIAL • Many challenges training this population – Both, staff & prisoners. • STIGMA & DISCRIMINATION. • Training refusals – fears of identifying self - insecure environment (i.e. group & with staff). • Confidentiality issues generally. • Changing attitudes of staff towards this group. • Training uptake more successful as individual `brief intervention’ (rather than group setting). • BI model replicates approach in the community. • Necessary to address needs (& training) of female prisoners. PERSONAL & INTERPERSONAL • Many challenges training this population – Both, staff & prisoners. • Necessary to acknowledge & challenge stigma & discrimination. • Necessary to change attitudes & prevent stereotyping (both ways). • Necessary to acknowledge & endeavour to change the systemic barriers. • Necessary to acknowledge & endeavour to work with the different dynamics & barriers – find out what works best! • Necessary to be flexible & willing to promote the programme – able to work with, both, adversity & diversity. FAMILIES & CARERS • Long recognised - families are crucial component of effective response to OD prevention & management. • Many families keen to get involved but lots of ethical & human rights issues re: issuing medication without explicit consent of individual at risk. • As such, family/carers’ can’t be supplied naloxone – presents major barrier but some PUD willing to consent. • Families’ can/are encouraged to, receive training as this is a crucial element for recognising/promptly dealing with an OD. • THN would be invaluable to those who have a significant other returning home after a period in prison, or detox / rehab centre – (? IN Naloxone may be better – easier for this group to use)! DENMARK – OD PREVALENCE • Register applies European definition of DRDs - Includes: “deaths caused by injurious use of drugs, addiction & drug psychoses, as well as deaths by poisoning, namely intentional & unintentional poisoning...” • 2011: Cause of Deaths Register - 285 DRDs. • 2010: 204 DRDs - Lowest recorded number since 1995. • 77.5 % DRDs = Males. • Mean Age = 44.7 years. DENMARK – A COLLABORATION • City of Copenhagen collaborated with Danish Drug Users Union (DDUU) as equal partners in the programme - establishing naloxone pilot - Direct involvement in planning & development. • Project's primary objective: To determine content & structure of OD Prevention course & how to deliver such training to peers. • Ongoing training, support & debriefing also provided by DDUU. • Those engaged in planning (of project) believe that, involving people who have daily / frequent contact with PUD, enables access to environments which are otherwise closed to professionals. • DDUU instrumental in establishing 1-year pilot project Distributing naloxone in one Danish municipality in order to assess its relevance for wider scale-up. DENMARK – A PEER-LED APPROACH • 2010: One year pilot project. • City of Copenhagen funded Health Centre to educate peers (called OD Therapists) to respond to OD. • 28 peers trained to respond to an OD - Allocated several doses of naloxone to use in the community. • 14 OD cases reversed in 10 months. • Copenhagen has demonstrated a simple & sustainable way to prevent OD deaths in Denmark. DENMARK – NALOXONE PROGRAMME • Based on recommendations (pilot model), programme now being trialled in 4 or 5 of larger cities across Denmark. • Since then, a community – (local `citizens group’ which has previous experience of setting-up mobile injection rooms, with volunteers at first, then the work was funded) - Have established their own naloxone project - (Antidote). • No naloxone programmes within prisons currently. • Given (established) peer networks providing (range of) harm reduction interventions, this may be area which can be addressed in terms of future development – (i.e. Prison THN). RECOMMENDATIONS from DENMARK • DDUU recommends prescription requirement for naloxone is removed - Drug is made available `over the counter’ (OTC). If not, the future development of OD Programmes may be restricted by medical resources that are already scarce. • Also agreed: equipment should be simplified – (Project used pharmaceutical form, already available in Denmark - has to be drawn up manually). • Make available other types of naloxone: pre-loaded syringes & intra-nasal (IN) spray – (generally) much easier to use. • DDUU recognises value of other groups being trained, including family, friends & employees in shelters, etc., as well as those people receiving opioid analgesics for pain management. To Summarise: DENMARK Project shows OD prevention is effective & efficient when delivered in close cooperation with local drug environment via peer-led approach – as supported by numerous international studies. Copenhagen Project - High degree of user involvement at all levels: a) DDUU involved in project planning, development, implementation & evaluation. b) OD Prevention Kits produced by PUD. c) Continuous assessment of equipment & project design undertaken - in collaboration with associated health professionals & other project stakeholders. Investment in PUD, services & rolling out a programme Recognised as a Public Health gain!!! ITALY • Data Issues generally – Monitoring & Evaluation • Said to be OTC & thus, more widely available?! Which is obviously better & improves access… • However, little information on any current programmes at the time of reporting. ITALY • Naloxone said to be distributed in community settings - Via NSPs, outreach, drug services & over the counter (OTC) in pharmacies. • Unable to find specific evidence to support this (at time of interview), nor any details regarding models for service delivery. • Unaware of any prison OD programmes currently being implemented. • Important to note: Issues with availability & translation of documents & therefore, this may not be an accurate reflection of the situation in Italy. SPAIN - CATALONIA This description relates to a programme in Catalonia. • Unaware of any structured, Spanish-wide OD programmes. In Catalonia, all of the following have protocols on OD Prevention & Management: • Hospital detox units • Harm reduction (HR) services • Outpatient (OPD) drug treatment centres • Therapeutic communities In Catalonia, approx. 7,000 people receive methadone treatment – General population = 7.5 million people. CATALONIA – NALOXONE PROGRAMME • Naloxone = Medically prescribed drug. • Its’ wider distribution & use is only permitted in order to save a life. • Assessed by Doctor prior to being dispensed naloxone - As many ampoules as needed. • Naloxone provided for treatment in emergency medical services, & in all harm reduction services, drug-consumption rooms (DCRs) & some outpatient drug treatment centres. DCRs • Drug consumption rooms (DCRs) able to reach many with naloxone programmes. • The centres have public health targets to train PUD - (opioid users). • PUD paid to attend the programme – (Incentives). • Initially, naloxone training extremely comprehensive but also rigid & protracted. • Training now more flexible as confidence has grown. ACTIVITIES and OUTCOMES • Some peer educators (former PUD) reported to be working informally from apartments to distribute naloxone. • Over 150 drug workers trained to educate PUD on OD prevention & management. • Between 2009 & 2012, approx. 3,000 PUD trained – • 4,500 Naloxone kits having been distributed. PRISON PROGRAMMES • Much work undertaken to progress prison-based Naloxone Programme in Catalonia. • 3 years developing operational protocols – (Strong opposition from trade unions re: naloxone kits with needles - despite plan for kits given upon release). • Recent meeting, at which, use of intra-nasal (IN) naloxone administration was suggested, as a solution. • No decision made at time of interview – (November, 2013). • Agreed that OD educational programmes will be delivered in all Catalan prisons. BREAK 11.30 am SESSION NINE Establishing a Programme ESTABLISHING a PROGRAMME The Process • Situation analysis / Needs assessment. • Legal framework. • National guidance & investment – training & education. • Negotiated, agreeable policies between PUD, emergency services – (ambulance & the police). • Technical support & programme development. • Types of kit. • Programme promotion. • Incentives & peer involvement. • Monitoring & evaluation. http://www.harm-reduction.org/sites/default/files/pdf/overdose_prevention_en_2012_02_07_0.pdf EXERCISE • Which components of each / any of the good practice models could apply to your country? • Consider the process for establishing such a programme and who would be responsible for each part? • How can others be engaged in the process? SESSION TEN Action Planning & Review Next Steps – Mentoring & Follow-Up Evaluation & Close ESTABLISHING COUNTRY ACTION PLANS • What actions or changes will occur (identify tasks)? • Who will carry out these changes? • By when will they take place, and for how long? • What resources (i.e., money, staff) are needed to carry out these changes? • Communication (who should know what?) • How will it be monitored and evaluated? CONSTRUCTIONIST REVIEW • A networking exercise to collectively review, appraise & refine evolving action plans… • And then, to discuss the next steps… BREAK – 15.15 MENTORING and FOLLOW-UP (Facilitating a journey into the unknown) CONSIDERING OPTIONS • Establishing a feasible mentoring model to refine and support country action plans • Balancing resources with flexibility in approach • Exploring options of on-line, email, telephone and blog approaches to follow up • Balancing individual, NGO and countrywide expectations for follow up ONE OVERDOSE DEATH is ONE TOO MANY! International Drug Users Remembrance Day July 21st ESSENTIAL REFERENCES • http://www.harmreduction.org/sites/default/files/pdf/overdose_prevention_en_2012_02_07_0.pdf