No08InfectionControl
advertisement

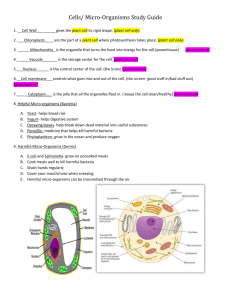
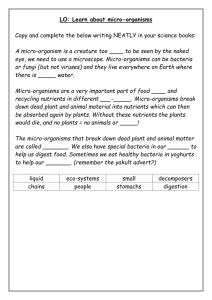
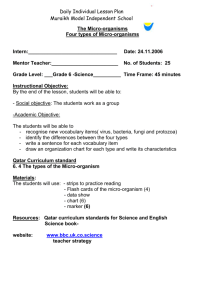
CLINICAL PRACTICE STATEMENT #8 (Issued: December 1996, replaces March 1990) INFECTION CONTROL Micro-organisms are very much a part of our world. The fact that they are invisible to the naked eye does not diminish their influence and effect on our day-to-day lives. Micro-organisms perform a variety of essential functions for us. In fact, they interact with every living creature, usually to the benefit of all. It is safe to say that life, as we know it, could not be sustained without them. Because micro-organisms can, in certain circumstances, threaten our well-being or existence, control measures have been developed to inhibit their spread. These control measures are based on a knowledge of the main factors which influence the spread of micro-organisms. These factors are: 1. Source of infection , including: i. People, both healthy and sick ii. Fomites (inactive objects or material on which disease-producing agents may be conveyed) iii. Instruments iv. Patient equipment, e.g. lines, tubes v. Food vi. Water vii. Air viii. Vectors such as mosquitoes, flies and birds. 2. Microbial (Causative) Agent . There are several categories of micro-organisms that can cause infection. These are bacteria, viruses, fungi and parasites. Some of these microorganisms are more pathogenic, i.e., likely to cause disease, than others. However, if conditions are favourable, any micro-organism is capable of causing disease in humans. 3. Portal of Exit The exit of the pathogen is dependent on the location of the microorganism in the body. Micro-organisms can be expelled from the respiratory tract during breathing, coughing, or sneezing, and from the gastrointestinal (GI) tract via saliva, emesis, faeces, or drainage from sites within the GI tract. Urine, blood, genital secretions, and drainage from wounds may also carry micro-organisms out of the body. 4. Portal of Entry These may be the same as the portals of exit. All of the portals have natural barriers that protect the body from micro-organisms. The barriers are normally effective but may allow micro-organisms to enter if the barriers are damaged or if they have been compromised by invasive medical devices, e.g., catheters. 5. Mode of Transmission Micro-organisms can be transmitted from their source by seven routes: i. Direct Hand Contact - This is the most common mode of transmission. ii. Indirect Contact - This occurs with exposure to contaminated fomites such as surgical dressings. iii. Droplet Contact - This can involve the conjunctiva, nose or mouth as a result of sneezing or coughing by an infected person. It is considered contact, rather than airborne, since droplets usually travel no more than three feet. iv. Airborne Transmission - This occurs by dissemination of an infectious agent by either droplet nuclei or dust particles in the air. The agent is widely dispersed by air currents and inhaled. v. Blood Borne Transmission - Micro-organisms are transmitted by percutaneous injury and contact with mucous or a raw wound. vi. Fomite - Fomites consist of inanimate objects such as food, clothing, drugs, equipment, or furniture. vii. Vectors - Vectors, e.g. mosquitoes, flies and birds, carry micro-organisms as part of their normal flora. 6. Susceptible Host Occasionally, circumstances arise where the normal balance between micro-organisms and their host is disturbed. This may be due to a disease process, altered immune status, infancy or old age, invasive procedures, drug therapy, poor nutrition, irradiation, etc. Should the host develop an infection as a result of this disturbance, a new reservoir of micro-organisms would be established, thus further increasing the risk of infection to other people. 7. Recommendations for Infection Control : a. Physiotherapists should wash their hands prior to and immediately after contact with each patient. i. wash vigorously with warm water and soap (pump dispenser preferred) for at least 10-15 seconds. ii. this is the best method for the prevention of transmission of organisms b. Physiotherapists should routinely use appropriate barrier precautions when contact with blood or body fluids is anticipated or when the physiotherapist has a rash or an open sore. i. gloves: Change after each patient contact. Discard after use. Do not reuse. Wash hands. ii. gowns: To be worn if handling large amounts of body fluids or if splashing of body fluids is anticipated. iii. mask and goggles: To be worn during procedures that are likely to generate droplets of blood or other body fluids. Should be worn when the patient has an extremely productive cough or when suction is employed or when the physiotherapist has a respiratory illness. c. Physiotherapists should take precautions to prevent injuries by needles, scalpels or other devices. i. do not recap any needles. ii. throw all used items into puncture resistant containers. iii. report any puncture needle, or open wound injury, immediately for appropriate treatment and monitoring. d. Disposable resuscitation equipment should be available to minimize mouth-tomouth contact. e. Up-to-date immunization status should be maintained for physiotherapists with patient-related duties. f. Physiotherapists with exudative lesions or weeping dermatitis that cannot be covered in a manner giving the patient full protection, should refrain from all patient care and handling of equipment until the condition resolves. g. Physiotherapists should ensure that adequate cleaning and garbage disposal procedures are practised: i. Equipment: Wash with germicidal agents (e.g. 1492 solution) or change surfaces that have been in contact with the patient. Surfaces which may be damaged by germicidal agents should be wiped clean and then wiped with a cloth soaked in 70% alcohol to disinfect. ii. Laundry: Wash on a high temperature cycle with normal bleach concentration and machine dry. Wet articles should be placed and transported in bags that prevent leakage. Use gloves if laundry soiled. Drycleaning and steam pressing is also appropriate. First remove contaminated surface material with damp paper towel. iii. Spills: In cleaning spills of blood or other body fluids, visible material should be wiped up with a paper towel and the area decontaminated with detergent solution. Gloves to be worn. iv. Garbage: Dispose in plastic bag, tie securely. h. If obtaining a specimen, the physiotherapist must ensure that the specimen is placed in a leak proof container. Dispose of as per municipal health requirements. i. Physiotherapists requiring additional information are referred to the regional infection control resource. References Infection Control Guidelines for Isolation and Precaution Techniques, Health and Welfare Canada, 1990 Infection Control, Introduction, Fraser-Burrard Hospital Society, 1995