2 - Clinical Trials Registry
advertisement

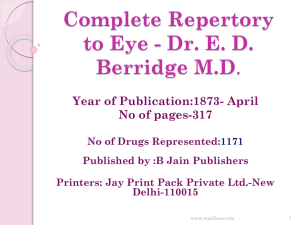
Efficacy of Homoeopathic Therapy in Cervical Spondylosis Pain Management – A Randomized Controlled Trial Regulatory Sponsor: Central Council for Research in Homoeopathy, New Delhi Funding Sponsor: Central Council for Research in Homoeopathy, New Delhi Study Product: A Randomized controlled Clinical Trial Study Team Chief Coordinator Dr. Alok Kumar, Director General In-charge Central Council for Research in Homoeopathy 61-65, Institutional Area, Opp. D-Block, Janakpuri New Delhi-110058 Co-Chief Coordinator Dr. Vikram Singh, Deputy Director (H) Central Council for Research in Homoeopathy 61-65, Institutional Area, Opp. D-Block, Janakpuri New Delhi-110058 Coordinator Dr. Jaya Gupta, Assistant Director (H) Central Council for Research in Homoeopathy 61-65, Institutional Area, Opp. D-Block, Janakpuri New Delhi-110058 Co- Coordinator Dr. Chetna Deep Lamba, Research Officer(H) Central Council for Research in Homoeopathy 61-65, Institutional Area, Opp. D-Block, Janakpuri New Delhi-110058 Investigators at centers 1.Dr. Ramesh Bawaskar,RO(H), RRI(H), Mumbai 2.Dr. Paul Sumithran, AD(H), CRI, Kottayam 3.Dr. Ramender Pal, AD(H),RRI(H),Jaipur 4.Dr. Shahid Ali, AD(H),DSU(EXT), Hydrabad 5.Dr. M. D. Arya, AD(H),CRI, Noida 6.Dr. Ashish Shivadikar, RO(H), RRI(H),Gudivada 7.Dr. Prakash Rao, AD(H), CRU, Puducherry. Protocol preparation team 1. Dr. Jaya Gupta, AD (H), CCRH, HQS. 2. Dr. Chetna Deep Lamba, RO(H), CCRH, HQS. 3. Dr. Ramesh Bawaskar, RO(H), RRI(H), Mumbai. Initial version: [8.6.11] Amended: [date] Amended: [date] 1 STUDY SUMMARY Title A multi centre randomized double blind placebo controlled clinical trial of Predefined Homoeopathic Medicines in Cervical Spondylosis Pain Management. Short Title Effect of Predefined Homoeopathic Medicines in Cervical Spondylosis Pain Management. Protocol Number Phase Methodology Study Duration Study Center (s) Objectives Version 1 Clinical Study Phase 2 Randomized Double Blind Placebo Controlled Clinical Trial 1 year Multi centre. 7 centers Primary Objective To evaluate the effectiveness of predefined homoeopathic medicines in cervical spondylosis pain management using Visual Analogue Scale for Pain. Secondary Objectives To assess pain, stiffness, limitation of movement and tenderness using Cervical Spondylosis Pain Management Scale (CSPMS). To assess the quality of life of patients treated with Patient and Clinical Global Impression scale. To find the clinical symptoms of homeopathic medicines used during trial, if any to enrich the Materia Medica. Number of Patients Diagnosis and Main Inclusion Criteria 140 cases Study Product, Route Duration of administration Reference therapy Statistical Methodology Outcome measures Male or female patients between 30-60 years fulfilling the following criteriaPatients with chief complaint of neck pain including pain in suboccipital and interscapular region within 2 weeks. One or more episodes of neck pain, neck stiffness attack on average per month for at least 3 months. Positive radiological findings for cervical spondylosis. VAS score for pain is minimum 4. Patient not on anti inflammatory or other therapy in the past 1week known to affect the study outcome. Predefined medicines, Oral route 7 days Placebo Paired T- test, Wilcoxon test, Mann-Whitney test and other appropriate test will be done during final analysis of the result. Visual Analogue Scale for Pain CSPMS Patient and Clinical Global Impression scale 2 Effectiveness of Predefined Homoeopathic Medicines in Cervical Spondylosis Pain Management – A Randomized Double Blind Placebo Controlled Trial 1. TITLE OF THE RESEARCH PROJECT A multi centre randomized double blind placebo controlled clinical trial of Predefined Homoeopathic Medicines in Cervical Spondylosis Pain Management. 2. PROJECT SUMMARY A Multi-centre Randomized Double Blind Placebo Controlled Clinical Trial of predefined homoeopathic medicines in cervical spondylosis pain management will be carried out by Central Council for Research in Homoeopathy, at its various Institutes/ Units throughout India. Participants will be selected from both sexes, age ranging between 30-60 years presenting with pain related to cervical spondylosis. The study shall have two arms viz. homoeopathic arm and placebo arm. Two series of medicines shall be used. One will comprise of medicines in 30C dilution manufactured by a licensed homoeopathic pharmaceutical company approved by the Council, the other will comprise of identical matching placebo. Assessment shall be done as per Visual Analogue Scale (VAS) and Cervical Spondylosis Pain Management Scale (CSPMS). Patients' Global Impression of Change (PGIC) scale and Clinical Global Impression (CGI) will be used for assessment. On conclusion of the study the data obtained shall be statistically analyzed with the help of a suitable statistical package (SPSS statistical package version 16) to see the effectiveness of predefined homoeopathic medicines in cervical spondylosis pain management and the results shall be disseminated to the medical fraternity. 3. JUSTIFICATION FOR THE STUDY AND USE OF THE RESULTS Cervical Spondylosis is a degenerative disease associated with ageing and also occupation. The growing geriatric population and sedentary occupation, increases the incidence of cervical spondylosis. In comparison with uncertainty in result and complication of surgical procedure in most cases of cervical spondylosis, the result of conservative treatment is so rewarding that surgery should not be considered unless pain persist for a few months or unless there is progressive neurological deficit. 1 None of the evidence from literature review indicates that one technique is better than another for clinically significant pain relief for patients with chronic cervical degenerative disc disease.2At this stage there is no valid study available in Homoeopathy which can prove the role of Homoeopathy for pain management in cervical spondylosis. 3 To validate the role of Homoeopathic medicine in cervical spondylosis pain management, Council aims to undertake the double blind placebo control trial with predefined Homoeopathic medicines. The result of this study will help the profession to get valid data about the usefulness of predefined homoeopathic medicines in cervical spondylosis pain management. 4. BACKGROUND The term cervical spondylosis describes chronic degenerative lesions of single or multiple interverteberal discs with formation of osteophytes in related vertebral bodies. The sequence of disc degeneration leads to the clinical syndrome of cervical pain, radiculopathy and myelopathy. Cervical spondylosis can be mechanical or metabolic both3. The most common symptom is intermittent persistent neck and shoulder pain. Neck pain is often accompanied by stiffness which progressively worsens. Pain may also radiate to the shoulders or to the occiput. Many patients present with interscapular pain, pain in the arm, forearm, and/or hand pain. Nonspecific headaches occur mostly in the sub-occipital region (lower part at the back of head) and this pain radiates to the base of the neck and to the vertex (top) of the head. 3 The use of anti-inflammatory drugs, muscle relaxants, analgesics, antidepressants, anticonvulsants, steroids, facet joint ablation, and physical therapy is the common line of treatment in modern medicine. Only a limited number of high-quality, randomized, controlled trials (RCTs) provide evidence of the effectiveness of NSAIDs or SMRs in the treatment of acute, uncomplicated musculoskeletal disorders. 4 From literature review, two studies are found on cervical spondylosis involving homoeopathic intervention , Mohan et. al.5 had recruited cases on the findings of cervical spine x-ray changes and found usefulness of homoeopathic treatment. But x-ray of spine cannot rule out the other causes of neck pain. The objective of the study was to find changes in the osteophytes; there was no objective measure of the impact of the disease on the patient. But Nayak 6 had taken the bowel nosode group of medicines and prescribed them on the basis of the corresponding micro-organism found in the stool culture and found the usefulness of the bowel nosodes in cervical spondylosis. Work done by the Council Central Research Units- Patiala and Udupi had conducted the research to clinically evaluate the action of predefined Homoeopathic medicines since August 1997. The results of the study indicated that Calcarea fluoricum, Cimicifuga and Rhus tox were useful.7 A prospective multicentric observational pilot study was also conducted by the Council at its 3 Units/Institutes during June 2009 - June 2010. The results of the study were found to be positive. Further RCT was suggested in this study for the validation of results. 8 4 Therefore, this study is proposed with predefined homoeopathic medicines in centesimal potencies with standard measurement scales in cervical spondylosis pain management. 5. STUDY OBJECTIVES 5.1. Primary Objective To evaluate the effectiveness of predefined homoeopathic medicines in cervical spondylosis pain management using Visual Analogue Scale for Pain. 5.2. Secondary Objectives To assess pain, stiffness, limitation of movement and tenderness using Cervical Spondylosis Pain Management Scale (CSPMS). To assess the quality of life of patients treated with Patient and Clinical Global Impression scale. To find the clinical symptoms of homeopathic medicines used during trial, if any to enrich the Materia Medica. 6. Operational Definition of Variables Cervical spondylosis- Spondylosis refers to age-related degenerative changes in spinal column. Occupations that place increased loads on the head predispose individuals to the development of cervical spondylosis. Symptoms caused by cervical spondylosis can be categorized broadly into three clinical syndromes; axial neck pain, cervical radiculopathy and cervical myelopathy.3 Postural neck pain- Neck pain during a particular posture and relieved as soon as changing that posture.3 Cervical Spondylosis Pain Management Scale (CSPMS)- To assess pain, stiffness, limitation of movement and tenderness has been developed by the Council (Annexure-8). Patients' Global Impression of Change (PGIC) scale - evaluates the activity limitations, symptoms, emotions, and overall quality of life.9 Clinical Global Impression (CGI) - evaluates the severity of illness, global improvement and efficacy index will be used for assessment at the end of the study.10 Centesimal potencies- The potencies used in centesimal scale are known as centesimal potencies. This was introduced by Dr. C. F. S. Hahnemann in 5th edition of Organon of Medicine in aphorism 270. Aggravation: Heightening of present symptoms of patient or overall worsening of patient’s condition. It may be of three types: Homoeopathic Aggravation: Because homoeopathic medicines are capable of producing similar symptoms as those of disease symptoms in somewhat higher degree, symptoms seems to be aggravated, after administering the most correct similimum ,this is called as homoeopathic aggravation. A quick and short homoeopathic aggravation is mostly desired after administration of homoeopathic medicines. 5 Medicinal Aggravation: Because of overdosing of medicines or when a partially indicated medicine is applied, some of the medicinal symptoms (non-homoeopathic symptoms) appear in a patient which is called as medicinal aggravation. Disease Aggravation: As a process of natural history of disease, disease condition aggravates which is called as disease aggravation. This happens when a wrong medicine has been employed Amelioration/ relief: Decrease in symptom score or improvement in general condition of patient or both is called as Amelioration or relief. Status quo: No change in patient’s condition. Adverse event: An adverse event is any symptom, sign, illness or experience that develops or worsens in severity during the course of the study. Intercurrent illnesses or injuries should also be regarded as adverse events. 7. METHODOLOGY 7.1 Type of Study and General Design This will be multicentric, prospective, double blind randomized placebo control clinical trial. The patients shall be divided into two groups. Group 1 shall be dispensed from Series I and Group 2 shall be dispensed from Series II. The groups formed shall be randomly assigned for either Series I or Series II through random numbers obtained from www.randomizer.org.11 7.2 Sites of the study It will be a multicentric study, which will be conducted at following Institutes under the Council. 7.3. 1. Drug standardization Ext unit, Hyderabad 2. Regional Research Institute, Mumbai 3. Regional Research Institute, Jaipur 4. Central Research Institute(H), Kottayam 5. Central Research Institute (H), Noida 6. Regional Research Institute(H), Gudivada 7. Clinical Research Unit (H), Puducherry Duration of study 1 year including follow up period of 8 days for each patient. 6 7.4. Sample Selection and Size Assuming 50% (P1) improvement with medicinal group and 25% (P2) improvement with placebo group, the required sample size for this study is 116 (58 per group) with α=0.05 and power 80%. Including dropout rate of 20%, the total sample size required is 140 (70 per group). As the study is to be conducted at 7 centres, the 20 samples (10 per group) will be required per centre. 7.5. Selection Criteria The patients will be enrolled from the OPDs of the study center (s) on the basis of presenting symptoms/signs of cervical spondylosis and laboratory investigational screening. 7.5.1. Inclusion criteria Patients meeting all of the following criteria will be eligible for study participation: Male or female patients between 30-60 years. Patients with chief complaint of neck pain including pain in suboccipital and interscapular region within 2 weeks. One or more episodes of neck pain, neck stiffness attack on average per month for at least 3 months. Positive radiological findings for cervical spondylosis. VAS score for pain is minimum 4. Patient not on anti inflammatory or other therapy in the past 1week known to affect the study outcome. 7.5.2. Exclusion criteria Patients meeting any of the following criteria will be excluded: Cervical myelopathy or radiculopathy. Patient with neck pain and normal x-ray Cervical spine. Patients on physiotherapy. Having neck trauma/ fracture/ surgery history/ congenital spinal abnormalities. Any systemic diseases of bones and joints. Other non-specific neck pain lesions—acute neck strain, postural neck ache, or whiplash. Suffering from any systemic diseases such as hypertension, diabetes mellitus, Cardio/ Cerebrovascular diseases etc. Inability to comply with the study protocol, alcoholics, drug users including psychiatric diseases. Pregnant and lactating women. Patients deemed ineligible by the investigators. Patient unwilling to sign the written informed consent form. 7 7.6. Investigations ESR C -reactive protein Rheumatoid (RA) factor Serum Calcium Serum Phosphorus Serum alkaline phosphatase X-ray cervical spine showing upto C7 ( Lateral view. Pull the shoulders downwards and if C7 is not visible, exclude the patient) 7.7. Primary end point To assess the changes in the pain severity through Visual Analogue Scale. 7.8. Secondary end point To assess the changes in CSPMS. To assess the rating of Patient and Clinical Global Impression (CGI) scale. 7.9. Primary safety end points Any adverse event in both the groups. 7.10 Randomization After final selection of medicine, Group 1 shall be dispensed from Series I and Group 2 shall be dispensed from Series II. The groups formed shall be randomly assigned for either Series I or Series II Random generated codes shall be made available from computer based software available from www.randomizer.org.11 The coding of series I and Series II shall be done by the pharmacist at headquarters. Randomization chart shall be available with the Investigator, Co-coordinator, pharmacist and Program officer for administrative purpose. Enrolment number of the patient shall be used for the purpose for randomization. Initial randomization shall be maintained during all follow up visits. 8. Unit of analysis and Observation The patients for the trial will be enrolled from the OPDs of the centers. Patients presenting with cervical pain to the OPD doctor will be considered for the trial. After taking consent, if a patient is found eligible, the investigator will enroll the patient into study. Assessment of pain from Visual analogue scale shall be done daily (at home). 8 Follow up will be done on 3rd day of study period and the CSPMS shall be filled by the physician along with the follow up form. If the patient is not reporting on due date then contact should be made by any means and details should be recorded. Final assessment shall be done on 8th day. CSPMS and Assessment of the quality of life of patients with Patient and Clinical Global Impression (CGI) scale shall be filled up on the 8th day of the study period. 8.1 Enrollment process The enrollment process will have 4 stages of participant selection before trial of homoeopathic therapy commences. Stage 1: Preliminary verbal screening by the OPD doctor Participants shall be recruited from those coming to Out Patients’ Department of the centre where the study has been assigned. While each centre will evolve its own advocacy procedures for attracting research subjects (advertisements, media, camps, handouts, etc.). They will all follow the standard recruitment procedure. The procedure involves a two stage screening prior to initiation of the consent procedure. The first screening is a verbal screening by the attending physician in the OPD. The OPD doctor will verbally screen the patients by enquiring the following: Is the age between 30 and 60 years? Patients with chief complaint of neck pain within 2 weeks. If yes to both, then the OPD doctor shall refer the patient to the concerned investigator for further screening (Annexure-1). Stage 2: Preliminary screening by the investigator Patient shall be screened by the investigator using a preliminary screening form [Annexure 2]. One who is eligible to enter the study as per Annexure 2 will be fully informed about the study as mentioned in the patient information sheet [Annexure 3] in the regional language. The investigators from all the Institutes/ Units involved in the study will obtain written informed consent of the patients prior to Detailed Screening on written informed consent form [Annexure 4]. If the patient does not happen to be literate, left hand thumbprint may be substituted for signature, duly witnessed by somebody in addition to the person requesting consent. Stage 3: Detailed screening/ Case Recording: 9 The patient shall undergo detailed screening [Annexure 5]. After detailed case taking, acute totality should be build up and only those cases falling within predefined medicines (with justifications) shall undergo the investigations [Annexure 6] as mentioned under section-6.7. of protocol. Thereafter, the patients fulfilling the criteria laid down under inclusion/exclusion will be enrolled in the study. On the basis of enrollment number, the patient shall be randomized as Group 1 and Group 2 [Annexure 7]. Stage 4: Baseline assessment CSPMS (Annexure 8) 9. Proposed Intervention 9.1. Source of medicine Two series of medicines shall be used. One will comprise of medicines in 30C dilutions manufactured by a licensed homoeopathic pharmaceutical company approved by the Council, the other will comprise of identical matching placebo. 9.2. Selection of medicine Based on the outcome of the previous studies and considering acute totality of pain of cervical spondylosis, the following medicines have been shortlisted for the homoeopathic arm in the study. List of trial medicines: 1. Paris quadrifolia 2. Calcarea carb. 3. Gelsimium 4. Cocculus indicus 5. Cimicifuga 6. Rhus toxicodendron 7. Causticum Selection of the medicine will be done after case taking on the basis of acute totality. The prescription shall be justified from different books of Materia Medica & Repertories. A compendium of therapeutics is enclosed for reference as appendix. 9.2.1. First prescription The indicated medicine or identical placebo shall be given in 30C potency. Doses: 4 pills of size No. 30 will be given in 21 doses. 9.2.2. Repetition of doses 3 doses shall be given at 6 hourly interval daily for 7 days. 9.3. Follow up (Annexure 10). 10 Treatment period shall be 7 days. The patient shall daily record the status of pain on VAS. The investigator shall fill the CSPMS and follow up form on 3rd day. 9.4. General Management No auxiliary measures shall be advised to the patient that may alleviate the pain. 10. ETHICAL REVIEW The study protocol will be in accordance with the latest revision of the Helsinki, declaration on human experimentation. Although homoeopathic medicines, proposed to be used during the study, are homoeopathic pharmacopeal preparations (no new drug is proposed to be tried) yet necessary clearance of the Ethical Committee and Scientific Advisory Committee has been obtained for this study. 11. PLAN FOR ASSESSMENT AND ANALYSIS OF RESULTS All the patients will be taught to recognize the signs of worsening & improvement of the illness according to those outlined in assessment form. They will be advised to report to the Institute/Unit if any of the signs develop at any time before the scheduled visit. Daily record of pain score has to be maintained for 8 days in VAS Scale. Patient shall undergo final assessment between 8th to 10th day. The CSPMS (Annexure-8) shall be filled up on 1st, 4th & 8th day of study period. If the patient does not report on a fixed date effort shall be made to contact him/her in any way. The data will be maintained in a excel sheet so that it can be procured every month and when necessary for interim analysis. Assessment of the quality of life by Patients' Global Impression of Change (PGIC) scale and Clinical Global Impression (CGI) on 8th day (Annexure 10and 11). In the eventuality of an adverse event, the participant shall be referred for appropriate medical care. Throughout the trial, participant shall be at liberty to withdraw her consent or refuse to continue treatment. Those who withdraw from the trial without prior intimation and stop coming for follow up or further treatment shall be treated as not reported. The participants i.e. withdrawn and not reported shall be treated as drop-out for compilation of final data at the conclusion of the study. 12. PROGRAM TO BE USED FOR DATA ANALYSIS The SPSS statistical package version 16 will be used to analyze the data. Paired T- test, Wilcoxon test, Mann-Whitney test and other appropriate test will be done during final analysis of the result. 13. PREMATURE WITHDRAWAL OF THE PATIENT 11 Every patient is free to withdraw from the trial at any time for any reason and without prejudice, or may withdraw on the advice of the investigator. Furthermore; the following circumstances may also arise for withdrawal: Any adverse event which needs referral of the patient. Necessity for taking medications or drugs which according to the exclusion criteria are not permitted during the trial or for other reasons. Personal circumstances which cause the patient not to intake the study medication. Other reasons, e.g. in-patient hospitalization, change of residence that may prevent the collection of follow-up data. Any patient who withdraws from the trial will undergo a complete final examination if possible, or at least a final telephone interview at the time of withdrawal from the study, with regard to the state of the patient's health, and if necessary, also from the point of view of drug safety and the validity of study results. The reasons for the withdrawal are to be recorded in the in the patient's case record. 14. PREMATURE STUDY TERMINATION The Council is entitled to terminate the trial prematurely at any time for medical and/or organizational reasons. This decision will normally be made on the recommendation of the Council. Should the trial be terminated prematurely, as far as possible each individual patient should undergo a complete final examination or at least a final telephone interview, with regard to the state of the patient's health, and if necessary, from the point of view of drug safety and validity of the trial results. 15. RECORD HANDLING 15.1 Record keeping The original records of patients will be maintained at the study centers and the photocopies of the same will be sent to the CCRH headquarters on completion of study and photocopies will be kept by the investigator. The original records will be handed over to the In-charge which will be preserved at the Institutes / Unit level for five years. All centres will send monthly report. Final concluding report shall be submitted to Hqrs. within 45 days of conclusion of the study. 15.2 Study management at site 12 Each center will be responsible for setting up an information system to keep track of all patients screened, enrolled and will maintain a filing system to keep all study records –study protocol, related documentation and medicine distribution records. The investigator is responsible for the completeness and accuracy of the study materials. 16. MONITORING AND INSPECTION Project monitoring and reviews: Each enrolled case record will be submitted to the study coordinator at CCRH headquarters as soon the case is enrolled for verification of the case record with all forms. Monitoring at site will be conducted during the study period for protocol compliance. 17. TRAINING Training will be imparted to all the investigators at CCRH headquarters and thereafter the investigator will train the concerned staff at each of their center respectively. 18. PROTOCOL AMENDMENTS The investigator has to meet the study requirements as specified in the protocol. Protocol amendments are possible only in exceptional cases (e.g. where the health or well-being of the patient is affected) and only after authorization by the Council. Every amendment must be justified in writing and signed by all those concerned. Circulating protocols will be numbered and a list of their distribution will be remained. The investigator will update all circulating protocols by adding the amendment. In the case of administrative or technical amendments which do not affect the health of patients, an administrative change is possible after agreement of all those concerned. These are also to be justified in writing and all those concerned are to be informed. Should a protocol amendment change the design of the trial fundamentally, or increase the potential risk to patients, a renewed approval by the Ethics Committee and Protocol Review Board as well as a renewed patient's informed consent is required, also from those patients already enrolled into the trial, as far as they are affected by this change. 19. COMMUNICATION/ PUBLICATION OF STUDY RESULTS All data derived from the study shall be the property of the Council. The papers on the outcome from the study shall be published under joint authorship (task force study). Authorship credit shall be based on 1) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; 2) drafting the article or revising it critically for important 13 intellectual content; and 3) final approval of the version to be published. Authors should meet conditions 1, 2, and 3. 20. LIMITATIONS OF STUDY Non-achievement of sample size at a particular site/center – i. In case of non achievement of sample size in the study period, there will be option for extension of the study for a further limited period after due approval of Scientific Advisory Committee of the Council. ii. If a particular site/center fails to achieve the sample size in first 6 months, or not complying to the protocol, the study will be discontinued and there will be an option for inclusion of one more center after due approval of Scientific Advisory Committee. 21. TIME LINE Draft protocol, submit to EC June 2011 Recruitment in main study After approval from SAC and registration with CTRI. Completion of study 1 year from the day of initiation. Data compilation and analysis 3months after completion of study. 22. REFERENCES 1. R. Braakman. J. Neurol Neurosurg Psychiatry. Management of cervical spondylotic myelopathy and radiculopathy.1994 March; 57(3): 257–263. 2. Jacobs W, Willems PC, van Limbeek J, Bartels R, Pavlov P, Anderson PG, Oner FC. Single or double-level anterior interbody fusion techniques for cervical degenerative disc disease. Cochrane Database of Systematic Reviews 2011, 4-1-38. 3 Ramani. Text book cervical spondylosis. Jaypee Brothers publishers,2004. 4. Beebe, Frank A1; Barkin, Robert L; Barkin, Stacie, A Clinical and Pharmacologic Review of Skeletal Muscle Relaxants for Musculoskeletal Conditions,American Journal of Therapeutics: March/April 2005 - Volume 12 - Issue 2 - pp 151-171. 5. Mohan G.R. et. al. Cervical Spondylosis- a clinical study. British Homoeopathic Journal. July.1996. 6. Nayak C. Study on Effectiveness of Homoeopathic Bowel Nosodes in the treatment of Cervical Spondylosis on the basis of Stool Culture Report. Indian Journal of Research in Homoeopathy. Vol. 2 , No. 1., 2008. 7. Central Council for Research in Homoeopathy. Annual Report 2001-2002. 8. Unpublished manuscript of the Council’s study. 14 9. http://chiroplushealthcare.com/PGIC.PDF accessed on 08.06.2011 10. http://www.servier.com/App_Download/Neurosciences/Echelles/CGI.pdf accessed on 08.06.2011 11. http://www.randomizer.org/form.htm accessed on 10.06.2011 15