OAFP Update 6-2
advertisement
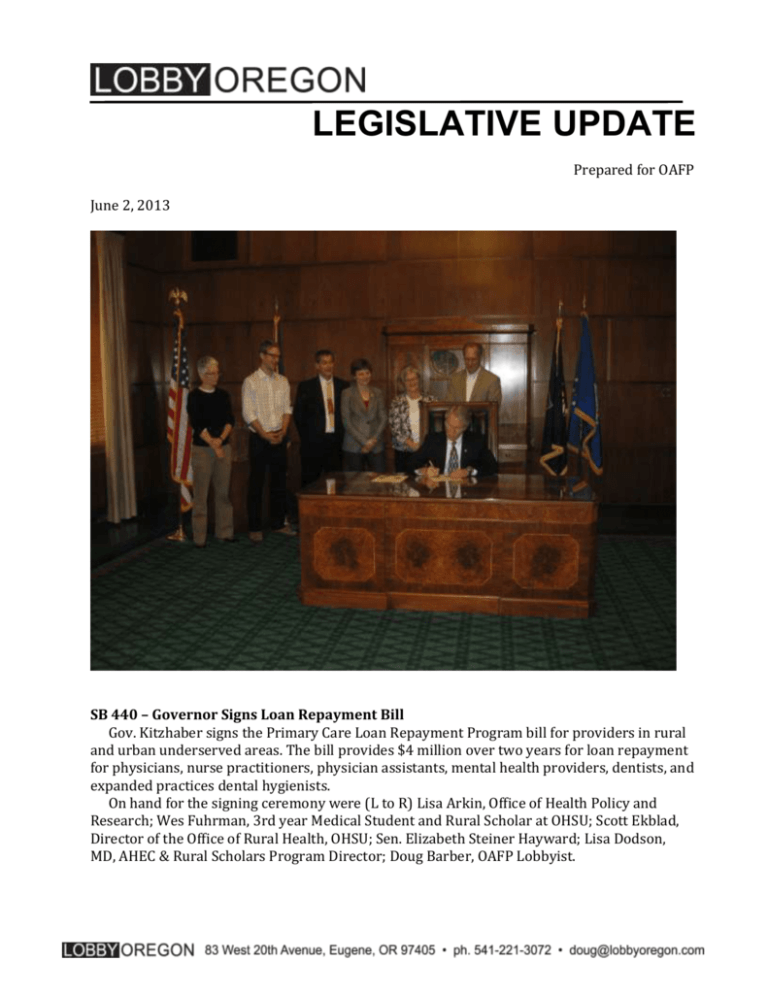
LEGISLATIVE UPDATE Prepared for OAFP June 2, 2013 SB 440 – Governor Signs Loan Repayment Bill Gov. Kitzhaber signs the Primary Care Loan Repayment Program bill for providers in rural and urban underserved areas. The bill provides $4 million over two years for loan repayment for physicians, nurse practitioners, physician assistants, mental health providers, dentists, and expanded practices dental hygienists. On hand for the signing ceremony were (L to R) Lisa Arkin, Office of Health Policy and Research; Wes Fuhrman, 3rd year Medical Student and Rural Scholar at OHSU; Scott Ekblad, Director of the Office of Rural Health, OHSU; Sen. Elizabeth Steiner Hayward; Lisa Dodson, MD, AHEC & Rural Scholars Program Director; Doug Barber, OAFP Lobbyist. 2 SB 325 – Tax Credits Committee hears possible amendments to Rural Health Tax Credits bill The Joint Committee on Tax Credits discussed four amendment issues with supporters of the Rural Health Tax Credit: 1. Requiring recipients to see Medicare and Medicaid patients 2. Changing the eligibility criteria from 60% of one’s practice to an average of 20 hours per week 3. An income cap of $250,000 for individuals and $500,000 for joint filers 4. Modifying the geographic eligibility to exclude communities between 30,000 and 40,000 population, primarily Grants Pass and McMinnville. The Oregon Rural Health Association (ORHA) proposed the first two based on a survey of tax credit recipients last summer. The Senate Health Committee added the income cap, but at the hearing, committee chair, Sen. Laurie Monnes Anderson (D-Gresham) testified, “The income cap turned out to be far more complicated to actually implement, so that may be something you want to take out.” The biggest debate is likely to come around #4, the change in geographic eligibility. About 236 practitioners would lose the tax credit if that amendment is adopted. Tax Credit Committee co-chair Sen. Ginny Burdick (D-Portland) likes the idea because it would save the state $2.36 million this biennium. But we know, based on the ORHA survey, that some practitioners will leave rural Oregon if they lose the tax credit. Overall, the credit has strong support. Rep. Cliff Bentz (R-Ontario) said, “This is hugely important to my district.” The question will be in the details. The Tax Credits Committee is expected to schedule a work session on SB 325 within the next few weeks. SB 569 – Telehealth Credentialing headed to Governor Rep. Chris Harker (D-Beaverton) briefly described on the House floor how SB 569 would streamline credentialing for Oregon’s telehealth providers. There was no discussion or debate before the House voted 59-0. The bill now goes to the Governor for his signature. HB 2902 – NP Parity in Ways and Means Because the nurse practitioner parity bill has a 13-member task force, the Ways and Means Committee had to sign off on it before the bill goes to the Senate floor for a vote. That happened on Friday. The bill has a minimal fiscal impact. Senate debate is expected some time next week. SB 721A – Concussions in club sports This bill requires coaches and referees in programs like Little League, Kids Sports and other non-interscholastic sports for kids 18 and under to have annual training on how to recognize the symptoms of a concussion and how to seek proper medical treatment. The House Health Committee raised liability concerns, so the bill was amended to make it clear that coaches and referees can only be liable if there is gross negligence. The amendment also exempts those who do not regularly coach or referee. Rep. Jason Conger (R-Bend) said, “I value very much this program and the importance of protecting kids from brain injuries.” The committee unanimously approved the new amendment and sent the bill to the floor for debate. 3 SB 683 – Patient Referrals As health care systems grow and integrate, Sen. Chip Shields told the House Consumer Protection Committee he worries about what that means for patient referrals. “How does that work for the little guy? The independent physical therapist who might provide better service at a lower price.” So Shields has pushed through SB 683, what he describes as “A shot across the bow to discourage anti-competitive behavior,” that carries with it a $1000 potential penalty per investigation. Patty O’Sullivan from the hospital association says providers “Must notify patients orally and in writing if you have a financial interest in the facility to which you are referring them and must let them know they may choose a different facility.” This bill was pushed in large part by a group of independent physical therapists whose lobbyists said, “Patients are going to be educated about their choices.” The bill now goes to the House floor for debate. SB 470B – House Committee modifies Rx Monitoring Program The House Health Committee kept the core of SB 470, which would allow a prescriber to designate other people in their office to access the Prescription Drug Monitoring Program (PDMP) to help prepare charts for the day. But the committee striped out the alert system that would have automatically sent notices to prescribers if one of their patients has received a number of the same prescriptions. Rep. Jim Thompson (R-Dallas) said, “If the physician is using the system as they are supposed to, they would see that their patient has had ten prescriptions for vicodin.” Thompson said other states tried this alert system and it didn’t work because there were so many alerts it clogged the system. The committee also deleted the portion of the bill that would have allowed the Board of Pharmacy to add drugs not in Schedules II through IV to the PDMP. The bill now goes to the House floor for debate. HB 2090 – OHP Preferred Drug List This bill continues the preferred drug list and the mental health carve out. Sen. Elizabeth Steiner Hayward (D-Portland) objected in the Human Services Subcommittee of Ways and Means saying, “Carving out mental health makes it different than any other biologic disorder.” The Governor also wanted to bring mental health drugs under the preferred drug list — and the $2.6 million it would have saved. Sen. Alan Bates (D-Medford) said this is a reasonable carve out and “The CCOs can have a discussion with the physicians who are prescribing these drugs” if they want to get better control of the costs. Sen. Jackie Winters (R-Salem) also supported the carve out saying, “This has been longstanding work, so those who did not have a voice had a voice in this body.” The bill now goes to the House floor. HB 3309 – CCO “Agree or Get Out” bill amended and sent to Ways and Means The House Rules Committee changed the bill that would allow a CCO to force out a board member and punish them by paying only 58% of Medicare for five years to a pilot project that only applies to Marion and Polk counties. The Oregon Health Authority would have to report to the legislature in 2013 on the “success” of the pilot project and “recommendations for expanding the pilot project statewide.” 4 The Rules Committee voted 6-2 to send the bill to Ways and Means. Rep. Vicki Berger (RSalem) objected saying the bill has no fiscal impact. But because Ways and Means is a joint committee (made up of House and Senate members) the bill can avoid going through a Senate committee later in the process, a critical step that could have derailed the bill. The large coalition opposing the bill still opposes it, even though it has been changed to a pilot project. The latest voice in opposition comes from ShelterCare, a mental health provider in Eugene and a member of the Trillium CCO in Lane County. Their letter says HB 3309 “allows some board members (many of which represent the same profit-driven entity) to use ‘exile’ and punitive pricing to strong-arm other board members who do not have as many votes on a board.” The only groups supporting the bill that I know of, are the old COHO IPAs (FamilyCare, MVIPA, DCIPA, etc.). SB 725 – Terms of CCO contracts & CCO Public Meetings This bill would give CCOs five-year contracts with the Oregon Health Authority. All session, Rep. Greenlick has been trying to find a way to force CCOs to comply with public meetings law or make their meetings open to the public. He finally added an amendment to SB 725 with new guidelines for the CCOs’ community advisory councils. They must meet quarterly, hold meetings at least twice a year that are open to the public, and must post contact information for one member of the council. The bill now goes to the House floor. HB 2859 – Ends OHP Standard The key to this bill is that it changes the Oregon Health Plan to one benefit package – OHP Plus. It eliminates OHP Standard benefits for the “expansion population” which allows Oregon to expand Medicaid eligibility for single adults up to 138% FPL. Because of that change, starting in January 2014, the federal government will pay 100% of the cost for that group and they will all receive the OHP Plus benefits. But on the floor of the House it was simply described as “aligning OHP with new Medicaid standards.” Rep. Tim Freeman (R-Roseburg) objected saying, “This is a huge policy shift, asking Cover Oregon to determine eligibility for the Oregon Health Plan.” Rep. Mitch Greenlick (D-Portland) responded, “Eligibility still remains with OHA. The application goes through Cover Oregon but OHA makes the determination.” The House voted 38-21 to approve the plan. It now goes to the Senate for a vote. SB 724A – CCO Non-traditional Accounting & Direct Payment to ASCs This is the so-called “air-conditioner bill” the would create a new accounting category for CCOs so they don’t have to include nontraditional items, like the Governor’s famous air conditioner example, under administration. House Health Committee chair Rep. Mitch Greenlick (D-Portland) joked that, “It is not my recommendation that air conditioners be billed to the Governor’s office.” The bill was also amended to address the issue of payments to out-of-network ambulatory surgery centers. The centers complain that when the checks (sometimes very large checks) are sent to the policyholder, the policyholder cashes them and doesn’t pay the bill. The solution is that from now on, the check will be made out to both the policyholder and the center. The committee approved the bill and sent it to the floor for debate. 5 SB 753 – OHP Fraud Detection sent to Rules This bill, which has the support of the Oregon Health Authority, would have the Oregon Health Plan use third-party software to flag possible fraudulent claims to be investigated before they are paid. The vendor is paid a percentage of recovered funds, so there is no cost to the state. SB 753 passed the Senate unanimously and had one brief hearing in the House Health Committee. But for some unexplained reason it got hung up, so Chair Greenlick sent the bill to the House Rules Committee to keep it alive. HB 2385 – Senate Committee passes DUII Mandate On a straight party-line vote, the Senate Health Committee approved requiring health insurance companies to pay for court-ordered DUII treatment. The debate came down to whether this constitutes a new insurance mandate under the Affordable Care Act (ACA). If it is, the state has to pay for it. In testimony to the committee, Rep. Phil Barnhart (D-Eugene) said, “It is quite clear that it is not a new mandate.” Barnhart cited information from the Center for Consumer Information and Oversight (CCIO) saying not paying for the treatment was discrimination. Sen. Jeff Kruse (R-Roseburg) disagrees saying, “Quite often the feds are wrong. I do think this is a new mandate. This is court ordered. That is a different critter.” Committee chair Sen. Laurie Monnes Anderson (D-Gresham) pushed the bill through saying, “I feel strongly if you have insurance, and have not been dropped by insurance, that treatment should be covered by your insurance.” The bill now goes to the Senate floor for debate. But that may not be the end for this issue. There is at least the possibility of a federal lawsuit to determine whether these new insurance requirements qualify as mandates under the ACA. SB 539 – Wellness program demonstration program The federal Affordable Care Act prohibits the use of wellness incentives in the individual insurance market except through a 10-state wellness program demonstration project. SB 539 instructs DCBS to apply for participation in that demonstration project. The House Health Committee approved the bill and sent it to the floor for debate. HB 3160 – UTPA bill sent to Rules Sen. Chip Shields (D-Portland) did not have the votes to pass his bill to add insurance to the Unfair Trade Practices Act (TRPA). But the bill isn’t dead yet. On the last day, on a straight party-line vote, he had his Consumer Protection Committee send the bill to the Senate Rules Committee. That means the bill will stay in play for the remainder of the session. ###