Pharm _lecture2008
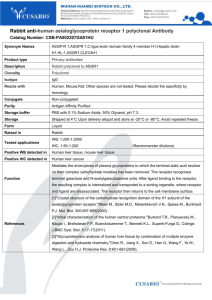
advertisement

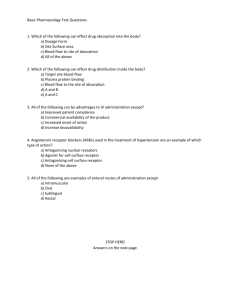
MU PT 7890 Case Management I General Principals of Pharmacology A. Pharmacokinetics - the process by which a drug is absorbed, distributed, metabolized, and eliminated by the body. What the body does to the drug. 1. Route of Administration Enteral = alimentary canal o Oral: subject to “first pass”: portal vein to the liver o Sublingual: directly to venous return. No first pass e.g. nitroglycerin o Buccal: directly to venous return. No first pass o Rectal: given if vomiting or unconscious. Poor absorption Advantages: Non invasive; Ease of drug administration; Mouth and the GI tract have a rich blood supply for pancorporeal dispersal of the medication; Avoids large fluctuations in drug delivery Disadvantages: Drugs must be lipid soluble; Drugs can be irritating to the mucosa of the mouth and the gut. Parenteral = outside alimentary canal o IV o intramuscular (IM): vaccines, botulinum (prolonged release into venous circulation) o subcutaneous (SQ): insulin, Norplant (contraceptive) o transdermal patch: e.g. nitro patch or fentanyl-opiod patch o transdermal iontophoresis and phonophoresis: lidocaine or dexamethasone are driven through dermal layer to local tissue o intrathecal, epidural: for administering analgesic, anesthetic, or antispasmodic (botulinum) Advantages: Fast delivery of the medications (IV, inhalation); Efficient maintenance of therapeutic ranges (IV); More predictable; Can give large quantities of medication Disadvantage: Invasive Topical- creams, eye/ear drops, nasal sprays (NS), inhalers (INH) (sometimes topical is lumped under parenteral) 2. Bioavailability: amount of drug that actually makes it to the intended downstream target. Influenced by route of administration and how easily it can cross cell membrane barriers (size, shape, charge, lipid soluble or protein-bound) 3. Metabolism / Biotransformation: deactivation by the liver, the “Great Detoxifier” (hydrolysis, oxidation, reduction, conjugation) 4. Elimination / Excretion: primarily by kidneys. minor roles played by: GI tract (bile salts), lungs (inhaled drugs), sweating, saliva, breast milk B. Pharmacodynamics – What the drug does to the body C. Pharmacotherapeutics - is using drug therapy to stimulate or depress certain biochemical or physiological functions in our patient to provide relief of symptoms or ideally to favorably alter the course of their disease. Therapeutic Index (TI) = Toxic dose / Effective dose This indicates the relative safety of a drug. For example: Acetominophen 27 Valium 3 Methotrexate, vincristine 1 Digitalis and Coumadin also have low (narrow) TI. Frequent blood draws needed to monitor levels. E. Mechanism of Action – 1. Agonist - drug mimics an endogenous substance that would normally stimulate a receptor 2. Antagonist - drug which binds a receptor site, doesn't stimulate it, but does block other substances from stimulating it F. Drug Nomenclature 1. Chemical name - example - n-acetyl-para-amino phenol 2. Generic drug name - example – acetaminophen. The FDA catalogs the drug by its generic name 3. Trade name / Brand name- example Tylenol. This is the name the manufacturer gives to the drug that distinguishes it from the same (generic) drug made by other drug companies. G. Off-label use A prescription drug may be prescribed for a purpose / diagnosis that is not approved by the FDA. No clinical trials have been done to study this off-label use. Example: gabapentin, Neruontin is an antiseizure medicine. It is commonly prescribed off-label for the pain of peripheral neuropathy. Cardiovascular and Pulmonary Medicines A. Antihvpertensives 1. Diuretics - causes diuresis which decreases plasma volume which decreases cardiac output which decreases blood pressure Important Side Effects - hypokalemia, hyperuricemia, hyperglycemia 2. Beta-blockers - block Beta-adrenergic receptors on sympathetic neuronal endings which decreases norepinephrine release therefore decreasing blood pressure Important Side Effects - bradycardia, bronchospasm, blocks hypoglycemic symptoms 3. ACE Inhibitors - Stop conversion of Angiontensin I to II in blood vessels resulting in vasodilation and decreased blood pressure Important Side Effects - hyperkalemia, lightheadedness, cough 4. Angiotensin II Receptor Blockers - Blocks angiotensin II at receptor 5. Calcium Channel Blockers - cause relaxation of cardiac & smooth muscle by blocking voltage sensitive calcium channels therefore causing vasodilation and decreased blood pressure Important Side Effects - muscle weakness, GERD, constipation B. CHF Drugs 1. Diuretics 2. Digitalis Glycosides - increases how forcefully the heart contracts. Important Side Effects - bradycardia, fatigue, dizziness, visual problems, increased toxicity w/ hypokalemia. Almost always will have a simultaneous prescription for potassium (K) supplement. C. Anti-angina Drugs 1. Nitrates- decreases stress on the heart via vasodilation Important Side Effects - light headedness and headache 2. Beta-blockers 3. Calcium Channel Blockers D. Treatment of Coagulation Disorders 1. Anti-coagulants: use to prevent and treat venous thromboembolism Heparin & like drugs - inhibit thrombin & factor X in the coagulation pathway. Warfarin/Coumadin - antagonizes Vitamin K which is important for several of the coagulation factors to work. 2. Anti-platelet / Antithrombotic: inhibit platelet (thrombocyte) aggregation. Used to prevent arterial thrombus Aspirin (ASA) & Plavix E. Antihyperlipidemics 1. Statins or HMG-CoA Reductase Inhibitors – blocks the enzyme for cholesterol synthesis in the liver. Important Side Effects - myalgias, gas, diarrhea, dyspepsia, increased liver enzymes F. Respiratory Drugs 1. Beta-2 Adrenergic Agonist- bronchodilators via direct stimulation of the beta-2 receptor Important Side Effects - CNS stimulants, increased pulse 2. Anticholinergics - Primarily COPD ..decrease secretions & some bronchodilation Important Side Effects – “SLUD” ↓ salivation (dry mouth), ↓ lacrimation (dry eyes), ↓ urination (risk of urinary retention), ↓ defecation (constipation) 3. Steroids - mostly for asthma exacerbations – rescue use Important Side Effects - delayed wound healing, increase glucose levels 4. Leukotrine Modifiers: long acting agent, antinflammatory properties 5. Cromones: long acting agent, reduces mast cell (secretory glands) reactivity in the airways Quiz Preview: _____ simvastatin (Zocor) A. diuretic _____ triamcinolone (Azmacort) B. beta-blocker _____ digoxin (Lanoxin) C. anticoagulant _____ isosorbide dinitrate (Isordil) D. angiotensin-converting enzyme (ACE) inhibitor _____ albuterol (Proventil) E. bronchodilator – beta agonist _____ furosemide (Lasix) F. vasodilator _____ metoprolol (Lopressor) G. positive inotrope _____ lisinopril (Zestril) H. antihyperlipidemic _____ warfarin (Coumadin) I. anti-inflammatory - steroid Other eligible drug classes for the quiz and exam: Cardiac alpha adrenergic blocker central alpha agonist calcium channel blocker angiotensin II receptor antagonist antiplatelet thrombolytic antiarrhythmic drugs (don’t need to remember which sub-class) not expected to distinguish the different classes of diuretics Pulmonary leukotrine inhibitors cromones anticholinergic skip xanthine derivatives References: Bill Morrissey PharmD R.Ph, Kilgore’s Medical Pharmacy, Columbia MO Ciccone, C. (2007). Pharmacology in Rehabilitation. (4th ed.). Philadelphia: F. A. Davis Company.




![Shark Electrosense: physiology and circuit model []](http://s2.studylib.net/store/data/005306781_1-34d5e86294a52e9275a69716495e2e51-300x300.png)