Practice -7
College of Health Sciences
Department of Medical Laboratories
Second Year – Second Term
Hematology – 1
Practice NO (7)
OSMOTIC FRAGILITY Test
OSMOTIC FRAGILITY Test, AS MEASURED BY LYSIS IN HYPOTONIC SALINE
Principle
Small volumes of blood are mixed with a large excess of buffered saline solutions of varying concentration. The fraction of red cells lysed at each saline concentration is determined colorimetrically. The test is normally carried out at room temperature (15-
25°C).
Reagents
Prepare a stock solution of buffered sodium chloride, osmotically equivalent to 100 g/l
(1.71 mol/l) NaCl, as follows: Dissolve NaCl, 90 g; Na
2
HPO
4
, 13.65 g (or
Na
2
HPO
4
2H
2
O,17.115 g); and NaH
2
PO
4
.2H
2
O, 2.34 g in water. Adjust the final volume to 1 litr e. This solution will keep for months at 4°C in a well-stoppered bottle. Salt crystals may form on storage and must be thoroughly redissolved before use.
In preparing hypotonic solutions for use, it is convenient to make first a 10 g/l solution from the 100 g/l NaCl stock solution by dilution with water. Dilutions equivalent to 9.0,
7.5, 6.5, 6.0, 5.5, 5.0, 4.0, 3.5, 3.0, 2.0, and 1.0 g/l are convenient concentrations.
Intermediate concentrations such as 4.75 and 5.25 g/l are useful in critical work, and an additional 12.0 g/l dilution should be used for incubated samples.
It is convenient to make up 50 ml of each dilution. The solutions keep well at 4°C if sterile, but should be inspected for moulds before use and discarded if moulds develop.
Method
Heparinized venous blood or defibrinated blood may be used; oxalated or citrated blood is not suitable because of the additional salts added to it. The test should be carried out within 2 hours of collection with blood stored at room temperature or within 6 hours if the blood has been kept at 4°C.
Prepared By Dr Abdelrhman elResheid1
1.
2.
3.
4.
Deliver 5.0 ml of each of the 11 saline solutions into 12 × 75 mm test tubes. Add
5.0 ml of water to the 12th tube.
Add to each tube 50 μl of well-mixed blood, and mix immediately by inverting the tubes several times, avoiding foam.
Leave the suspensions for 30 min at room temperature. Mix again, and then centrifuge for 5 min at 1200 g.
Remove the supernatants and estimate the amount of lysis in each using a spectrometer at a wavelength setting of 540 nm or a photoelectric colorimeter provided with a yellow
–green (e.g., Ilford 625) filter. Use as a blank the supernatant from tube 1 (osmotically equivalent to 9 g/l NaCl).
5.
Assign a value of 100% lysis to the reading with the supernatant of tube 12
(water), and express the readings from the other tubes as a percentage of the value of tube 12. Plot the results against the NaCl concentration
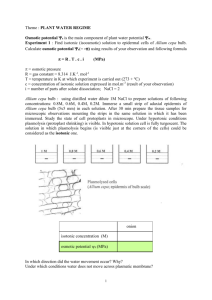
Figure 10.1 Osmotic fragility curves. Osmotic fragility curves of patients suffering from the following: sickle cell anaemia, β-thalassaemia major, hereditary spherocytosis, and “idiopathic” warm autoimmune haemolytic anaemia. The normal range is indicated by the unbroken lines
Prepared By Dr Abdelrhman elResheid2
Notes
% lyses = O.D of sample X 100
O.D of tube 12
1.
The measurement of osmotic fragility is a simple procedure that requires a minimum of equipment. It will yield gratifying results if carried out carefully.
2.
The blood must be delivered into the 12 tubes with great care. The critical point is not that the amount be exactly 50 μl, but rather that the amount added to each tube must be the same.
3.
If the amount of blood available is limited (e.g., from babies), and the spectrometer takes 1 ml cuvettes, the volumes can be scaled down to
1 ml of saline solution and 10 μl of blood. However, to deliver 10 μl of blood reproducibly is not easy.
4.
With the method using 50 μl of blood and with non-anaemic blood, the reading for 100% lysis will be about 0.7. With a modern spectrometer, any figure between 0.5 and 1.5 is acceptable. If the value is less than
0.5, the test should be repeated using more blood or less saline (the reverse if the reading is higher than 1.5). With photoelectric colorimeters, values higher than 0.5 are often not very accurate.
5.
When transferring the supernatant from a tube to the spectrometer cuvette, care has to be taken not to disturb the pellet. If it is well packed, the supernatant can simply be poured from the tube into the cuvette; with a spectrometer provided with an automatic suction device, this is usually satisfactory. Alternatively, a plastic Pasteur pipette should be used.
6.
Even when a normal range has been established, it is essential always to run a normal control sample along with that of the patients to be tested to check, for example, the saline solutions.
The sigmoid shape of the normal osmotic fragility curve indicates that normal red cells vary in their resistance to hypotonic solutions. Indeed, this resistance varies gradually (osmotically) as a function of red cell age, with the youngest cells being the most resistant and the oldest cells being the most fragile. The reason for this is that old cells have a higher sodium content and a decreased capacity to pump out sodium.
Factors Affecting Osmotic Fragility Tests
In carrying out osmotic fragility tests by any method, three variables capable of markedly affecting the results must be controlled, quite apart from the accuracy with which the saline solutions have been made up. These are as follows:
Prepared By Dr Abdelrhman elResheid3
1.
The relative volumes of blood and saline
2.
The final pH of the blood in saline suspension
3.
The temperature at which the tests are carried out
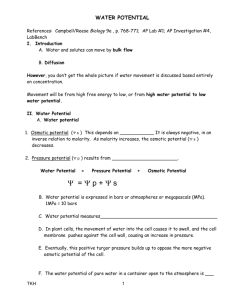
Recording the Results of Osmotic Fragility Tests
In the past, osmotic fragility most often has been expressed in terms of the highest concentration of saline at which lysis is just detectable (initial lysis or minimum resistance) and the highest concentration of saline in which lysis appears to be complete (complete lysis or maximum resistance). It is, however, useful also to record the concentration of saline causing 50% lysis
(i.e., the median corpuscular fragility [MCF]) and to inspect the entire fragility curve The findings in health are summarized in.
Osmotic fragility in health (at 20°C and pH 7.4)
Fresh blood (g/l NaCl)
Initial lysis 5.0
Complete lysis 3.0
MCF (50% lysis) 4.0
–4.45
MCF, median corpuscular fragility.
Interpretation of Results
Decreased osmotic fragility indicates the presence of unusually flattened red cells (leptocytes) in which the volume-to-surface area ratio is decreased.
Such a change occurs in iron deficiency anaemia and thalassaemia in which the red cells with a low mean cell haemoglobin (MCH) and mean cell volume
(MCV) are unusually resistant to osmotic lysis A simple one-tube osmotic fragility is a useful screening test for β thalassaemia and some haemoglobinopathies in countries with a high incidence of these abnormalities .
The osmotic fragility of red cells that have an abnormal membrane, such as those of HS and hereditary elliptocytosis (HE), increases abnormally after incubation Similar results occur in hereditary stomatocytosis. The results with red cells with a glycolytic deficiency, such as those of pyruvate kinase (PK) deficiency, are variable. In severe deficiencies, osmotic fragility may increase
Prepared By Dr Abdelrhman elResheid4
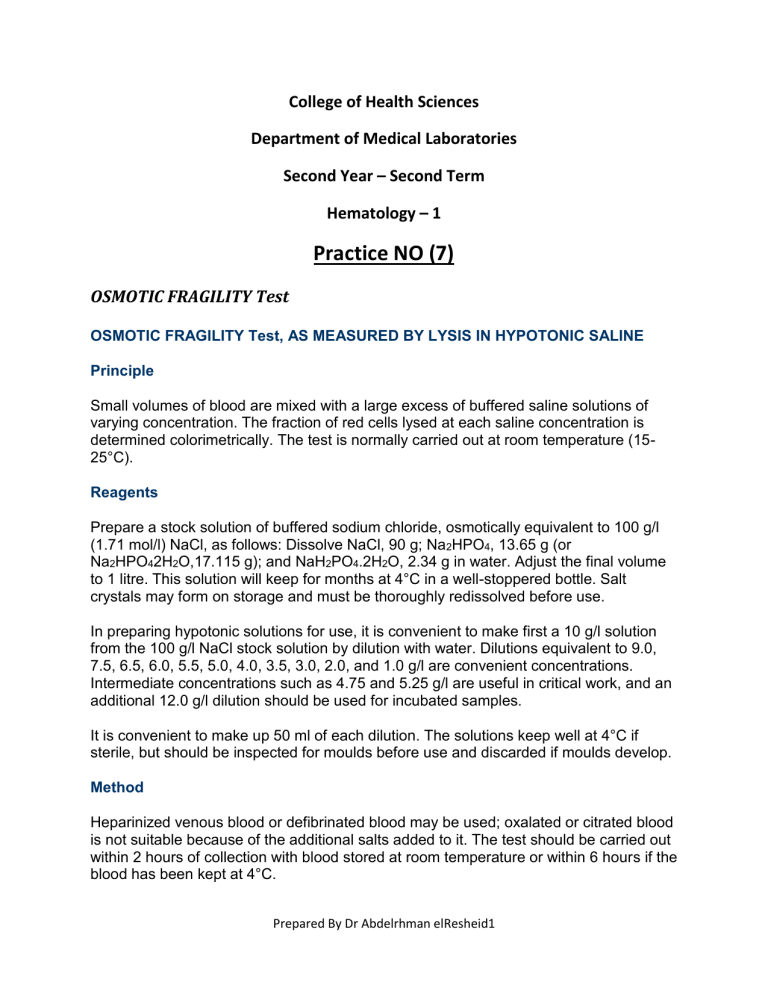
Figure 10.3 Osmotic fragility curves of three patients suffering from hereditary spherocytosis belonging to the same family (brother, sister and uncle [Le Ay]). The area between the unbroken lines represents the normal range. measurement of red cell osmotic fragility provides a useful indication as to whether a patient's red cells are normal because an abnormal result invariably indicates abnormality. The reverse is, however, not true (i.e., a result that is within the normal range does not mean that the red cells are normal). The findings in some important haemolytic anaemias are summarised in Table 10.2 .
Prepared By Dr Abdelrhman elResheid5
Table 10.2
-- Osmotic fragility in haemolytic anaemias: a summary
Condition Notes
A. Associated with increased osmotic fragility (OF)
Hereditary spherocytosis
(HS)
Entire curve may be “shifted to the right,” or most of it may be within the normal range but with a “tail” of fragile cells. Curve within normal range in 10 –20% of cases.
After incubation for 24 hours, abnormalities usually more marked, but still some false-negative results.
Splenectomy does not affect MCF but reduces the tail of fragile cells
Hereditary elliptocytosis (HE)
As in HS, but in general changes less marked
Abnormal OF usually correlates with severity of haemolysis (i.e., OF is normal in nonhaemolytic HE)
Hereditary stomatocytosis
Other inherited membrane abnormalities
As in HS with large osmotically fragile cells with low
MCHC
Results variable; with milder disorders curve more likely to be abnormal after incubation for 24 hours
Autoimmune haemolytic anaemia
Tail of fragile cells roughly proportional to number of spherocytes; rest of curve normal (or even left-shifted on account of high reticulocytosis)
B. Associated with decreased OF
Thalassaemia
Enzyme abnormalities
MCF decreased in all forms of thalassaemia, except in some α-thalassaemia heterozygotes; usually the entire curve is left-shifted
OF usually normal (anaemia originally referred to as hereditary nonspherocytic), but tail of highly resistant cells may be seen on account of high reticulocyte court
After incubation for 24 hours, there may be a tail of fragile cells
Increased resistance to osmotic lysis and increased
MCHC
Hereditary xerocytosis
Iron deficiency Curve shifted to left, wholly or partly, depending on proportion of hypochromic red cells
OF, osmotic fragility; HE, hereditary elliptocytosis; HS, hereditary spherocytosis; MCF, median corpuscular fragility; MCHC, mean cell haemoglobin concentration.
Prepared By Dr Abdelrhman elResheid6